
National Vital
Statistics Reports
Volume 69, Number 2 January 30, 2020
This report was revised
on July 15, 2020, to
impute missing values
for race and Hispanic
origin for consistency
with other publications,
slightly changing
non-Hispanic maternal
deaths in Figure 2,
Tables D and 1, and
pages 1 and 5 text.
Maternal mortality is a high-profile health indicator used in
domestic and international settings (1–3). In the United States,
the National Center for Health Statistics’ (NCHS) National Vital
Statistics System (NVSS) is the source for official mortality
statistics, including those on maternal mortality. NCHS uses
the World Health Organization (WHO) definition for maternal
mortality: deaths of women while pregnant or within 42 days
of being pregnant, from any cause related to or aggravated by
the pregnancy or its management, but not from accidental or
incidental causes (i.e., neither caused nor complicated by the
woman being pregnant at the time of or within 1 year of death).
The classification of deaths involving pregnancy, childbirth and
puerperium specifically excludes external causes (i.e., accidents,
homicides, and suicides) as incidental. Late maternal deaths
(occurring between 43 days and 1 year of death) are also not
included as part of the WHO definition of maternal mortality.
NVSS has produced maternal mortality statistics for more
than a century based on causes of death reported on death
certificates. Over time, other data collection efforts emerged,
such as the Pregnancy Mortality Surveillance System in 1986,
and evidence demonstrated that the NVSS data underestimated
maternal mortality (4–9). To address the underreporting of
maternal deaths in vital statistics, a separate pregnancy checkbox
item was added to the U.S. Standard Certificate of Death in 2003;
see other reports that describe the checkbox implementation
in more detail (10,11). NCHS initially paused publication of
maternal mortality trends as states were transitioning to the
checkbox format. However, as implementation of the standard
checkbox took longer than expected, NCHS paused publication
of annual maternal mortality rates as well. As a result, NCHS has
not published an official estimate of the U.S. maternal mortality
rate since 2007. Now that all states have implemented a checkbox
as of the 2018 data year (noting that California implemented a
different checkbox from that on the U.S. Standard Certificate of
Death), NCHS is resuming publication of the maternal mortality
rate starting with 2018 data.
Maternal Mortality in the United States: Changes
in Coding, Publication, and Data Release, 2018
by Donna L. Hoyert, Ph.D., and Arialdi M. Miniño, M.P.H., Division of Vital Statistics
Abstract
This report describes changes in how the National Center for
Health Statistics (NCHS) will code, publish, and release maternal
mortality data and presents official 2018 maternal mortality
estimates using a new coding method. Due to the incremental
implementation of the pregnancy status checkbox item on the 2003
revised U.S. Standard Certificate of Death, NCHS last published
an official estimate of the U.S. maternal mortality rate in 2007.
As of 2018, implementation of the revised certificate, including
its pregnancy checkbox, is complete for all 50 states (noting that
California implemented a different checkbox than that on the U.S.
Standard Certificate of Death), allowing NCHS to resume the routine
publication of maternal mortality statistics. However, an evaluation
of data quality indicated some errors with the reporting of maternal
deaths (deaths within 42 days of pregnancy) following adoption of
the checkbox, including overreporting of maternal deaths among
older women. Therefore, NCHS has adopted a new method (to be
called the 2018 method) for coding maternal deaths to mitigate
these probable errors. The 2018 method involves further restricting
application of the pregnancy checkbox to decedents aged 10–44
years from the previous age group of 10–54. In addition, the 2018
method restricts assignment of maternal codes to the underlying
cause alone when the checkbox is the only indication of pregnancy
on the death certificate, and such coding would be applied only to
decedents aged 10–44 based solely on the checkbox when no other
pregnancy information is provided in the cause-of-death statement.
Based on the new method, a total of 658 deaths were identified in
2018 as maternal deaths. The maternal mortality rate for 2018 was
17.4 deaths per 100,000 live births, and the rate for non-Hispanic
black women (37.3) was 2.5 to 3.1 times the rates for non-Hispanic
white (14.9) and Hispanic (11.8) women. Rates also increased with
age. Maternal mortality rates calculated without using information
obtained from the checkbox are also presented for 2002, 2015,
2016, 2017, and 2018 to provide comparisons over time using a
comparable coding approach across all states.
Keywords: death certificate • pregnancy status checkbox •
National Vital Statistics System
Introduction
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES
Centers for Disease Control and Prevention
National Center for Health Statistics
National Vital Statistics System
NCHS reports can be downloaded from: https://www.cdc.gov/nchs/products/index.htm.
2 National Vital Statistics Reports, Vol. 69, No. 2, January 30, 2020
Implementation of the pregnancy checkbox item accounts
for a substantial increase in both the number of deaths identified
as maternal and the resulting maternal mortality rates (10–12),
with the impact varying by age, race and Hispanic origin, and
state. When combining data for all states where the number of
states adopting the checkbox increased differentially over time,
the observed trend in maternal mortality appears to indicate
an increase. However, it has been shown that this is mainly a
reflection of the states’ incremental implementation of the
checkbox over a 14-year period. It could not be determined
whether this effect is due to better ascertainment of true maternal
deaths, or to increases in deaths coded as maternal in error, or
some combination of both (11,13).
Coding procedures adopted with the checkbox
implementation in 2003 and used through 2017 (referred to
throughout this report as the 2003–2017 method) are based on
causes of death reported on death certificates and information
on pregnancy status reported in the checkbox item. The
coding instructions specify assigning a maternal code from the
International Classification of Diseases, 10th Revision (ICD–10)
to all medical conditions reported if there is any indication of
pregnancy on a death certificate. Such indications include when
causes specific to pregnancy, delivery, or the puerperium are
reported in the cause-of-death section of the death certificate;
pregnancy is mentioned among the medical conditions reported
on the death certificate; or a response in the checkbox item that
indicates the woman had been pregnant at the time of death
or in the preceding year. If the checkbox response is the only
indication of a pregnancy in the past year on the death certificate,
the term “checkbox-only” is used to refer to these deaths. The
2003–2017 method restricted application of the checkbox item to
ages 10–54 years (see the next section on “Evidence and Effects
of Checkbox Errors” for more details on reporting patterns for
women aged 55 and over).
Based on research on the quality of maternal mortality data
using information obtained from the checkbox (10,11), NCHS has
adopted a new method for coding maternal deaths to mitigate
some of the quality concerns identified by multiple evaluations
of information on pregnancy status provided in the checkbox.
NCHS has also adopted a new method for displaying the coded
causes of death for maternal deaths in the mortality data file.
This report describes the changes in how NCHS will code and
release maternal mortality data and provides maternal mortality
rates for 2018 using the new coding method. The 2018 maternal
mortality rates using the new method are compared with rates
calculated using the 2003–2017 method to highlight differences
that result from applying the two coding methods. Maternal deaths
for 2015–2018 were also recoded without using the information
in the checkbox, as would have been the case before 2003. The
rates for 2015–2018 were then compared with the rate for 2002
to provide comparable information on trends in maternal deaths.
Considerations for assessing trends are also discussed.
Evidence and Effects of Checkbox Errors
Recent research has demonstrated that errors are common
in the reporting of pregnancy status using the checkbox. Rossen
et al. reviewed the literature on reporting errors in the checkbox
and reported a range of false-positive rates (i.e., indication of
pregnancy or pregnancy in the past year when the decedent was
not actually pregnant or pregnant in the last year) as high as
50% (11). An analysis conducted internally by NCHS that linked
hospital records with death certificates for selected hospitals
suggested potential false positive rates of 54% and 56% for the
checkbox in 2014 and 2016, respectively. Note, however, that
these results are not based on nationally representative data
(see Technical Notes, “Checkbox item analysis based on National
Hospital Care Survey data linked to National Death Index,” for
further information).
Davis et al. (12) examined patterns by age and discussed the
likelihood of misclassification with increasing age. Subsequent
research supported the thought that false positives resulting from
errors in the checkbox item were concentrated among decedents
in their 40s and 50s (14). Research on data from four states
(Georgia, Louisiana, Michigan, and Ohio) found that a pregnancy
indicated by the checkbox for those under age 40 was more likely
to be corroborated, and a pregnancy for those aged 45 and over
was more likely to not be corroborated—for example, 19% of
decedents aged 45–49 with a positive checkbox response (i.e.,
pregnant or pregnant in the last year) had actual evidence of a
pregnancy (14).
To evaluate the use of the checkbox for women aged 40
and over, checkbox entries were tabulated by age of decedent
and compared with the number of births for these age groups.
In the NVSS mortality data for 2013 (including all states except
Alabama, Alaska, Colorado, Hawaii, Massachusetts, North
Carolina, Virginia, and West Virginia, which did not use the
standard checkbox in 2013), 797 deaths of women aged 40 and
over had a checkbox entry indicating they were pregnant at the
time of death or pregnant in the last year from any cause; 652
of these pregnancies were reported as occurring among those
aged 45 and over; and 147 of these pregnancies were reported
as occurring over age 85. The number of decedents reported
as pregnant or pregnant in the last year is unrealistically large
at older ages and, by ages 60–64, far surpasses the reported
number of women giving birth in those age groups (Table A).
The exact cause of these errors is unclear. If the checkbox
errors are random (i.e., certifiers are selecting the wrong
checkbox item with the same regularity across all ages, or even
with a lower error rate at the older ages), the absolute number
of errors would be larger at the older ages simply because the
volume of all deaths increases as age increases. To illustrate this,
Table B uses data from before the checkbox was implemented
to show the number of female deaths for decedents under age
25 through 54 from all causes, the number of maternal deaths
identified from the cause-of-death section of the certificate,
and the number of maternal deaths that potentially would be
added assuming that the checkbox would have introduced a
hypothetical constant error rate of 0.03%. The number of deaths
potentially added in error increases with age. For those aged
45–54, an error rate in the checkbox item of 0.03% could result
National Vital Statistics Reports, Vol. 69, No. 2, January 30, 2020 3
in an additional 74 deaths, inflating the actual number of maternal
deaths by 452%. For the data years used for Table B (1999–2002,
before the checkbox was implemented), no maternal deaths were
reported beyond age 54.
When information on pregnancy is found only in the
checkbox with no mention of maternal causes in the cause-of-
death section, the net result of errors in reporting pregnancy
status is a substantial overreporting of maternal mortality,
especially for older women (12,15,16). In the study by Catalano
et al., ages 45 and over were identified as those for which a
response in the pregnancy checkbox is more likely to be an error
(14). The results from Table B align with this finding.
New Approach for Coding Maternal
Deaths: Description of 2018 Method
A new method (referred to as the 2018 method) for coding
maternal deaths has been adopted to mitigate the effect of
reporting errors in the checkbox item and to retain cause-of-
death detail lost in the application of the 2003–2017 method.
Table A. Number of births and deaths with positive pregnancy
responses in the checkbox: United States, 2013
[Deaths could include any cause (International Classification of Diseases, 10th
Revision codes A00–Y89) but checkbox entry indicates pregnant at time of death,
pregnant within 42 days of death, or pregnant between 43 days and 1 year of
death]
Age Births Deaths
40–44 . . . . . . . . . . . . . . . . . . . 134,540 145
45–49 . . . . . . . . . . . . . . . . . . . 10,329 89
50–54 . . . . . . . . . . . . . . . . . . . 780 148
55–59 . . . . . . . . . . . . . . . . . . . 74 33
60–64 . . . . . . . . . . . . . . . . . . . 7 51
65–69 . . . . . . . . . . . . . . . . . . . – 45
70–74 . . . . . . . . . . . . . . . . . . . – 51
75–79 . . . . . . . . . . . . . . . . . . . – 46
80–84 . . . . . . . . . . . . . . . . . . . – 42
85 and over . . . . . . . . . . . . . . – 147
– Quantity zero.
NOTE: Alabama, Alaska, Colorado, Hawaii, Massachusetts, North Carolina, Virginia, and
West Virginia did not have the standard checkbox in 2013.
SOURCE: NCHS, National Vital Statistics System.
This new method will be used for all jurisdictions (see Technical
Notes, “California data and coding methods”). Procedures will
generally remain the same for records with reported terms or
phrases indicating pregnancy and obstetric causes in the cause-
of-death statement for all ages. The 2018 method introduces two
changes to the 2003–2017 method in the coding of maternal
deaths. The first change is that coding of maternal (and late
maternal) deaths will further restrict application of the checkbox
item to decedents aged 10–44 instead of 10–54 as is done with
the 2003–2017 method. The checkbox will not be used for
decedents aged 45 and over in light of the findings discussed
above on the checkbox quality for women in this age group
(14). The result is that for female decedents aged 45 and over,
maternal codes will not be assigned if the only indication of a
pregnancy was in the checkbox using the 2018 coding method.
This change does not affect coding procedures for decedents
aged 10–44.
The second change involves how causes of death for
maternal (and late maternal) deaths are reported on the mortality
file. When the pregnancy checkbox item indicated that the
decedent was pregnant or pregnant within the preceding year,
application of the 2003–2017 method assigned all medical
conditions reported on the death certificate for decedents aged
10–54 to maternal codes, rather than to nonmaternal codes for
the causes listed on the certificate. However, doing so provided
no means of identifying the record as a checkbox-only case
without additional information beyond what is normally available
in the standard data files (e.g., literal text), and no way to
identify potential errors for specific records. In addition, for the
checkbox-only records, the maternal codes assigned often retain
less detail about the causes reported. The change implemented
with the 2018 coding method for decedents aged 10–44 only
codes the underlying cause of death to a maternal code when
the checkbox is the only indicator of a pregnancy in the last year
(i.e., only the underlying cause will be modified, except in cases
where the underlying cause is an external or incidental cause,
which is the practice regardless of method). The result of this
change is that most of the original detail lost when applying the
2003–2017 method is retained, and the record better reflects
what was actually reported on the death certificate. In addition,
when using this new format, checkbox-only records will be
flagged with an indicator on the mortality files.
Table B. Number of deaths potentially added if 0.03% of certificates have a checkbox in error
Age All female deaths Maternal deaths
Maternal
mortality rate
(deaths per 100,000
live births)
Number of deaths
potentially added if
0.03% of certificates
have a checkbox in error
Maternal mortality
rate including those
potentially added in
error (deaths per
100,000 live births)
Under 25 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 39,796 384 6.5 12 6.7
25–39 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 102,796 1,018 10.4 31 10.7
40–54 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 324,934 141 37.0 97 62.4
40–44 . . . . . . . . . . . . . . . . . . . . . . . . . . 79,796 120 33.2 24 39.8
45–54 . . . . . . . . . . . . . . . . . . . . . . . . . . 245,138 21 107.6 74 486.6
NOTES: Using counts from the National Vital Statistics System, mortality data for 1999–2002 for all female and maternal deaths for the ages are shown for illustration. These numbers were
previously published according to how maternal deaths were determined before 2003. The error rate of 0.03% was selected based on the percentage of female decedents in 2013 aged 55 and
over with a positive pregnancy checkbox.
SOURCE: NCHS, National Vital Statistics System, Mortality.
4 National Vital Statistics Reports, Vol. 69, No. 2, January 30, 2020
Generally, more information is reported on death certificates
than is directly reflected in the underlying cause of death. This
additional information is captured in multiple cause-of-death
data that are available on the data files. Multiple cause-of-death
data are retained in two forms: entity axis and record axis. The
entity axis preserves details on where causes associated with
the codes were reported on the death certificate. The record
axis reflects some transformation of the entity axis codes to
facilitate analysis, eliminates duplicate codes, and includes the
underlying cause code. Record axis and entity axis generally
would differ somewhat between coding methods (for examples,
see Technical Notes). Using the 2018 method, for checkbox-only
records, those aged 10–44 would have only one maternal code,
which would appear in the record axis as the underlying cause.
The entity axis would consist entirely of nonmaternal codes. Also
using the 2018 method, checkbox-only records for those aged
45–54 would consist only of nonmaternal codes in both entity
and record axis. For the records with terms or phrases related to
pregnancy or obstetric conditions, in the cause-of-death section
of the certificate, the multiple-cause data would be the same as
before.
The changes incorporated with the 2018 method (see
Technical Notes for examples) are summarized as:
• Coding of maternal deaths will restrict application of the
checkbox item to decedents aged 10–44. The checkbox will
not be applied in the coding of cause of death for decedents
aged 45 and over when no other cause-of-death information
related to pregnancy is indicated on the certificate; however,
the original checkbox entries will be retained on the file for
this age group.
• If the checkbox is the only indication of a pregnancy for female
decedents aged 10–44, a maternal code will be assigned as
the underlying cause, except in cases where the underlying
cause is an external or incidental cause, which would not be
coded as maternal regardless of coding method. A maternal
code will be assigned only to the underlying cause and not
to other conditions reported on the certificate. The other
original causes will be retained on the record.
Cases in which a pregnancy or obstetric condition is
reported in the cause-of-death section will continue to be coded
as maternal deaths regardless of age.
Maternal Mortality in 2018
In 2018, a total of 658 women were identified as having
died of maternal causes in the United States (Table 1) using the
2018 coding method. The maternal mortality rate for 2018 was
17.4 deaths per 100,000 live births. The maternal mortality rate
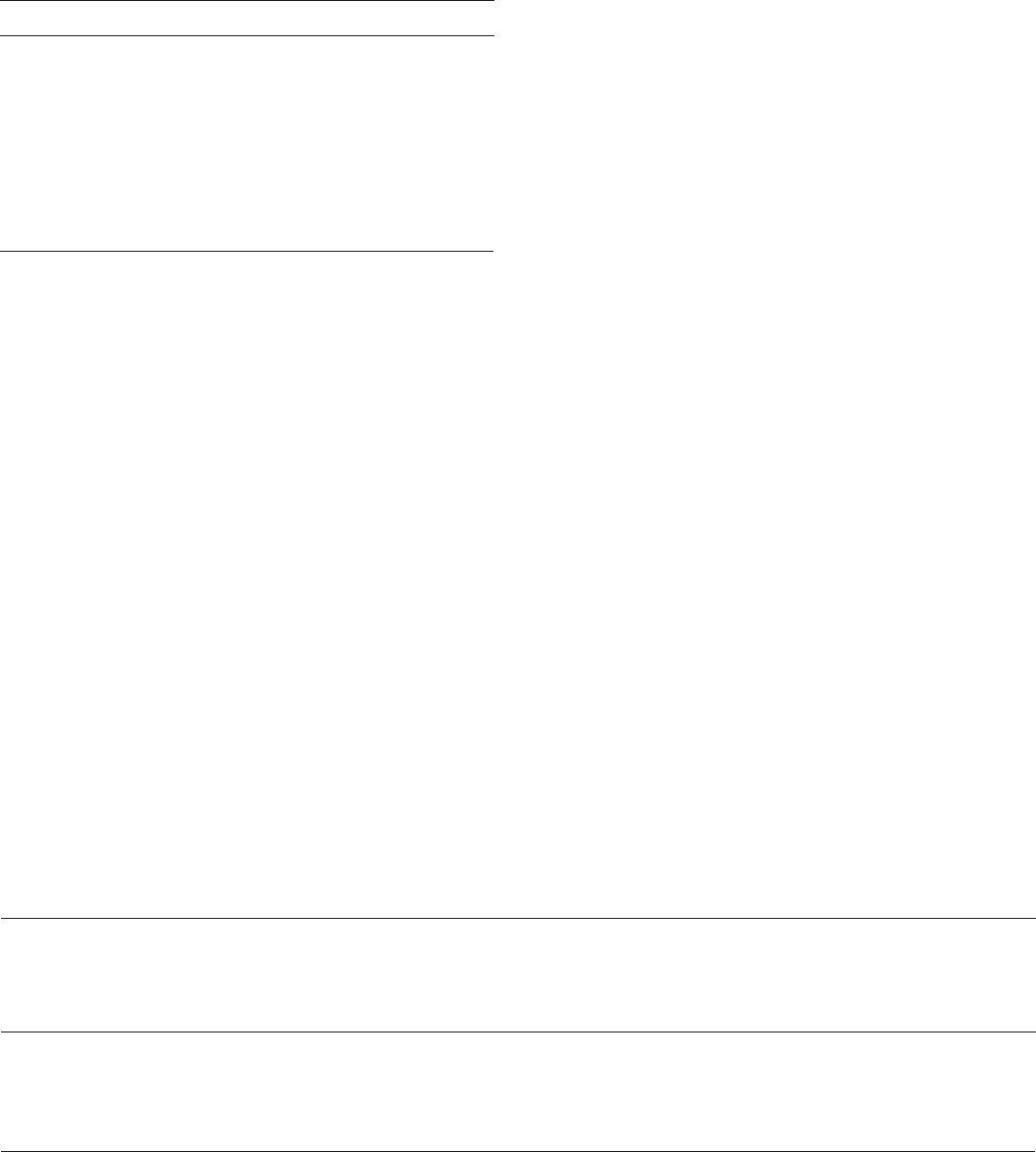
increases with successively older age groups (Figure 1), with the
rate for women aged 40 and over (81.9) equal to 7.7 times that
for women under age 25 (10.6).
Figure 1. Maternal mortality rates, by age: United States, 2018
Deaths per 100,000 live births
SOURCE: National Vital Statistics System, Mortality.
17.4
10.6
16.6
81.9
0 20 40 60 80 100
All ages
Under 25
25–39
40 and over

National Vital Statistics Reports, Vol. 69, No. 2, January 30, 2020 5
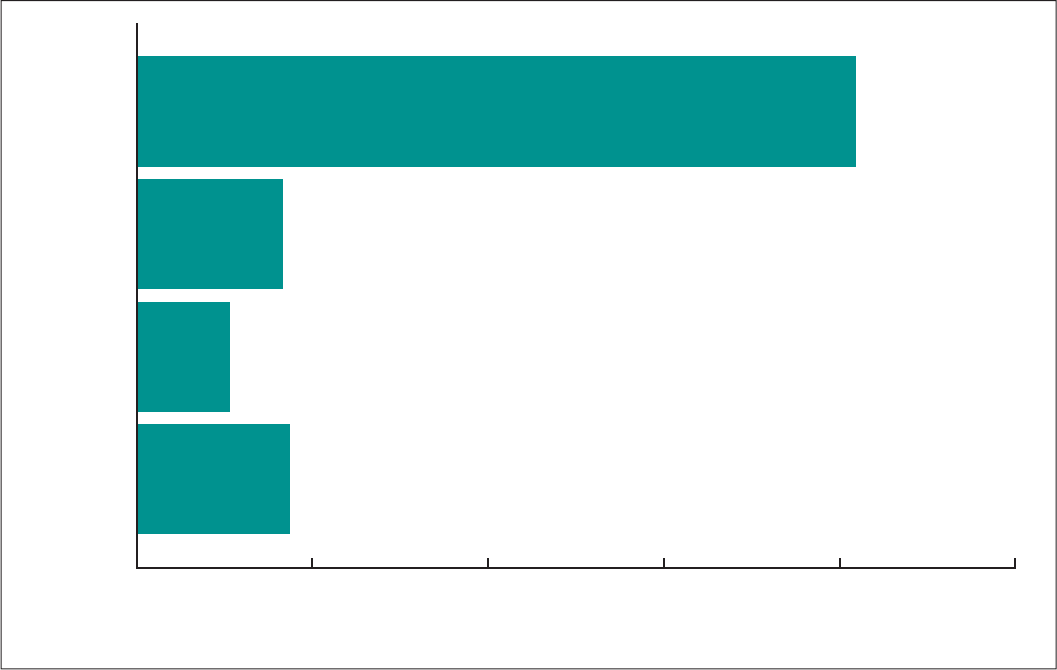
As shown in Figure 2, the maternal mortality rate for non-
Hispanic black women (37.3 deaths per 100,000 live births) was
2.5 times the rate for non-Hispanic white (14.9) and 3.1 times the
rate for Hispanic women (11.8) (Note: Rates are shown by single
race group; see Technical Notes for information on bridged-race
results and more information on the differences between single
and bridged race). In 2018, the ratio for non-Hispanic white
women to Hispanic women was 1.3.
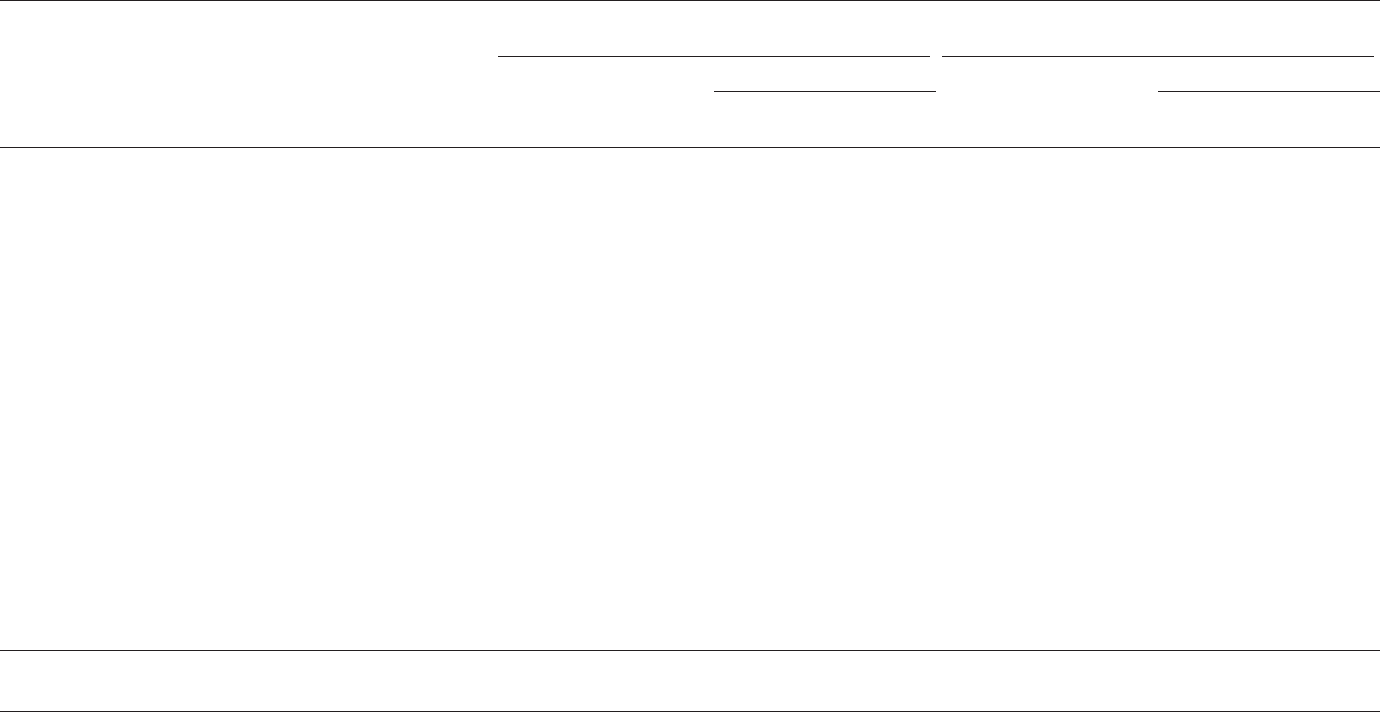
Maternal deaths may be viewed using more detailed causes
of death, which are broadly divided into direct and indirect
obstetric causes (Table 2; note that some of the more detailed
cause categories have vague titles or small numbers). Using the
2018 method, more deaths were classified to direct obstetric
causes (A34, O00–O95) (77%) than to indirect obstetric causes
(O98–O99) (23%) in 2018. Figure 3 shows the percent distribution
of selected maternal death causes (which each account for
4%–6% of maternal deaths), a category for indirect causes
(accounts for 23% of deaths), and the category “Remaining direct
obstetric causes,” which encompasses many codes (e.g., O10,
O12, O21–O43, O47–O66, O68–O71, O73–O75, and O95) and
accounts for about one-half of the deaths. Described in terms
of maternal mortality rates, Abortive outcomes, which primarily
are ectopic pregnancies, and Hemorrhage of pregnancy and
childbirth and placenta previa both occurred at a rate of 0.8
deaths per 100,000 live births in 2018. The rate for Eclampsia
and pre-eclampsia was 0.9 deaths per 100,000 live births, and
the rate for Obstetric embolism was 1.1 deaths per 100,000 live
births.
Not included in Figures 1–3 are the 277 deaths that were
reported as occurring more than 42 days but less than 1 year after
delivery in 2018, for a late maternal mortality rate of 7.3 deaths
per 100,000 live births. Late maternal deaths are not included as
part of the official maternal mortality rate (see Technical Notes,
“Late maternal deaths”).
Results From 2018 Method Compared
With 2003–2017 Method
Tables 1 and C show maternal mortality rates for 2018
calculated based on both the 2003–2017 method and the 2018
method. Given that the change in use of the checkbox with the
2018 method is applied to women aged 45–54, the maternal
mortality rates are the same for age groups under 25, 25–39,
and 40–44 for both methods (Table 1). The ratio of the maternal
mortality rates for those aged 40 and over to under age 25
(Table C) is 16.6 when using the 2003–2017 method and 7.7
when using the 2018 method, reflecting the higher error rate
in identifying maternal deaths at older ages in the 2003–2017
method and the decision to restrict the use of the checkbox to
those under age 45. For women aged 45 and over, there are
only seven deaths when using the 2018 method’s expanded
SOURCE: National Vital Statistics System, Mortality.
Deaths per 100,000 live births
0
10
20
30
40
11.8
Hispanic
37.3
Non-Hispanic black
14.9
Non-Hispanic white
Race and Hispanic origin
Figure 2. Maternal mortality rates, by single race and Hispanic origin: United States, 2018

6 National Vital Statistics Reports, Vol. 69, No. 2, January 30, 2020
restriction on age, which results in a rate that does not meet
NCHS standards of reliability (73.1). Using the 2003–2017
checkbox method, the ratio of the maternal mortality rates
among those aged 45 and over to those under age 25 is 124.1,
and 6.9 when using the 2018 method, but these again are based
on rates that are statistically unreliable.
Maternal mortality rates for non-Hispanic black
women (Tables 1 and D) were consistently higher than for
non-Hispanic white (Note: Rates are shown by single race group;
see Technical Notes for information on bridged-race results and
more information on the differences between single and bridged
race) and Hispanic women based on both methods. The ratio
of the rates for non-Hispanic black women to non-Hispanic
white women was 2.4 with the 2003–2017 method and 2.5 with
the 2018 method. The ratio for non-Hispanic black to Hispanic
women was 3.2 using the 2003–2017 method and 3.1 using the
2018 method.
Table 2 shows numbers and maternal mortality rates by
cause based on the different coding methods. The distribution of
the causes of death is similar for these two methods (Figure 4).
In 2018, the maternal mortality rate for indirect obstetric causes
was 5.1 deaths per 100,000 live births using the 2003–2017
method, whereas when using the 2018 method, the rate was 3.9.
For direct obstetric causes, the rate was 15.4 deaths per 100,000
live births using the 2003–2017 method, compared with 13.4
when using the 2018 method. Within the direct causes, rates
were 0.8 deaths per 100,000 live births for Other complications
predominantly related to the puerperium using the 2003–2017
method, and 0.7 using the 2018 method; 1.0 for Eclampsia and
pre-eclampsia using the 2003–2017 method, and 0.9 using
the 2018 method; and 1.2 for Obstetric embolism using the
2003–2017 method, and 1.1 using the 2018 method. Maternal
mortality rates increase with increasing age for the different
causes of death regardless of method.
Comparison of Rates With Those of
Pre-checkbox Era
NCHS last published information on the U.S. maternal
mortality trend in 2002. It is not appropriate to compare maternal
mortality for 2018 with previous years when the checkbox had
not been adopted by all states and the number of states adopting
the checkbox increased each year. Observed changes in the rate
reflect the increasing number of states adopting the checkbox
rather than a change in the risk of maternal death. The maternal
Figure 3. Percent distribution of maternal deaths, by
cause of death: United States, 2018
0
20
40
60
80
100
2018 method
SOURCE: National Vital Statistics System, Mortality.
22.6
52.3
4.3
6.5
4.6
5.3
4.4
Remaining direct obstetric
causes
Total indirect obstetric causes
Other complications
predominantly related to
the puerperium
Obstetric embolism
Hemorrhage and placenta previa
Eclampsia and pre-eclampsia
Abortive outcome
Percent
Indirect
obstetric
causes
Direct
obstetric
causes
Table C. Maternal mortality rates and ratio of maternal
mortality rates, by coding method and maternal age:
United States, 2018
[Rates are per 100,000 live births. Ratio of maternal mortality rates is for
specified maternal age to those under age 25]
With checkbox
(2003–2017
coding method)
With checkbox for
ages 44 and under;
without checkbox
for 45 and over
(2018 coding method)
Age Rate Ratio Rate Ratio
Under 25 . . . . . . . . . . . . . . . . . . . . . . . . . 10.6 1.0 10.6 1.0
25–39 . . . . . . . . . . . . . . . . . . . . . . . . . . . 16.6 1.6 16.6 1.6
40 and over . . . . . . . . . . . . . . . . . . . . . . 175.7 16.6 81.9 7.7
40–44 . . . . . . . . . . . . . . . . . . . . 82.6 7.8 82.6 7.8
45 and over . . . . . . . . . . . . . . . 1,315.9 124.1 *73.1 *6.9
* Figure does not meet NCHS standards of reliability.
SOURCE: NCHS, National Vital Statistics System.
Table D. Maternal mortality rates and ratio of maternal
mortality rates, by coding method and single race and
Hispanic origin: United States, 2018
[Rates are per 100,000 live births. Ratio of maternal mortality rates is for
non-Hispanic black women compared with non-Hispanic white and Hispanic
women]
Race and Hispanic origin
With checkbox
(2003–2017
coding method)
With checkbox for
ages 44 and under;
without checkbox
for 45 and over
(2018 coding method)
Rate Ratio Rate Ratio
Non-Hispanic white . . . . . . . . . . . . . . . . 18.2 2.4 14.9 2.5
Non-Hispanic black . . . . . . . . . . . . . . . . 43.5 1.0 37.3 1.0
Hispanic . . . . . . . . . . . . . . . . . . . . . . . . . 13.7 3.2 11.8 3.1
SOURCE: NCHS, National Vital Statistics System.

National Vital Statistics Reports, Vol. 69, No. 2, January 30, 2020 7
mortality rate calculated without using the checkbox, as would
have been done before 2003 (referred to as the pre-2003
method), provides statistics calculated in the most equivalent
way possible (i.e., without the checkbox) for the entire United
States over time (10). These comparisons are provided in this
report to show comparisons using the most recent data and
as many recent time points as possible. As of this report, data
have been recoded without using the checkbox for only the
2015–2018 data years.
Table E shows maternal mortality rates for 2002 (8.9),
2015 (8.7), 2016 (8.7), 2017 (11.5), and 2018 (8.7). Except for
2017 (11.5), the rates were not statistically different from the
rate in 2002 (8.9). These results are similar to the other reports
previously mentioned, which also demonstrate that the maternal
mortality rate did not increase significantly either after accounting
for the staggered implementation of the checkbox by states
(using the modeled approach) (11) or as if the checkbox had
never been implemented (10). It is possible that recoding cause
of death without using the checkbox can miss some deaths that
would have been identified had the checkbox not been present,
such as if the certifier did not list a maternal cause in the cause-
of-death section of the death certificate because pregnancy was
indicated in the checkbox.
Figure 4. Percent distribution of maternal deaths, by cause of death using two coding methods: United States, 2018
Maternal Mortality Data Release Moving
Forward
Starting with the 2018 data year, the 2018 method will be
incorporated as part of NCHS’ standard production of the public-
use mortality data. The 2018 mortality data are being released
at the same time as this report and will include maternal deaths
coded according to the 2018 method. All official statistics on
maternal mortality from 2018 and subsequent years will be
based on the 2018 method.
Starting with the 2018 data file, the underlying-cause and
multiple-cause (both entity axis and record axis) fields will be
the same as originally coded for the records reporting terms
and phrases indicating pregnancy or obstetric conditions
0
20
40
60
80
100
2018 method2003–2017 method
NOTE: Totals may not add to 100 due to rounding.
SOURCE: National Vital Statistics System, Mortality.
Remaining direct obstetric causes
Total indirect obstetric causes
Other complications predominantly
related to the puerperium
Obstetric embolism
Hemorrhage and placenta previa
Eclampsia and pre-eclampsia
Abortive outcome
Percent
22.6
52.3
4.3
6.5
4.6
5.3
4.4
24.8
53.0
3.7
5.7
4.1
4.9
3.7
Indirect
obstetric
causes
Direct
obstetric
causes
Table E. Maternal mortality rates using the pre-2003 method:
United States, 2002 and 2015–2018
[Rates are per 100,000 live births]
Year Number of deaths Rate
2002 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 357 8.9
2015 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 345 8.7
2016 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 345 8.7
2017 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 442 11.5
2018 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 331 8.7
NOTE: Data for 2002 are included for comparison with the 2015–2018 values.
SOURCE: NCHS, National Vital Statistics System.
8 National Vital Statistics Reports, Vol. 69, No. 2, January 30, 2020
for decedents of all ages. For checkbox-only records, not all
conditions on the record will be assigned maternal codes as
was previously done. Instead, only the underlying cause will be
modified. Entity axis fields will not be modified. In addition, in
the record axis fields, the nonmaternal code that would have
been selected as the underlying cause if no checkbox item had
been available will be flagged (see data documentation for the
2018 mortality file for details). For decedents aged 45–54 with
a positive checkbox item and no reported information related to
pregnancy in the cause-of-death section, the underlying-cause
and multiple-cause fields will reflect coding done without using
the checkbox item; see Technical Notes for an illustration with a
couple of examples. The checkbox value will still be available in
the mortality files as a separate field.
For the data files that have been released previously
(2003–2017), maternal records are being recoded without
using the checkbox item (pre-2003 method) and will also be
recoded according to the 2018 method. These data, along with
the original coding (2003–2017 method) and the pregnancy
checkbox item, will be incorporated into an additional, separate
restricted-use data file that will be available to researchers
through the NCHS Research Data Center. The official data files
for 2003–2017 already released will not be changed. Reclassified
data for 2015–2017 are being released along with this report.
Data for 2003–2014 will be added to this file as the recoding for
each year is completed. These data will provide researchers with
access to cause-of-death codes using alternate coding methods
and provide maximum flexibility for analysis using different
methods and assumptions. As addressed earlier, the pre-2003
method underestimated maternal deaths, the 2003–2017
method overestimated maternal deaths for older women, and
the 2018 method is designed to lessen the effect of likely errors
in the checkbox. Trend analyses for data pre-2018 using either
the 2003–2017 or 2018 method are limited by the incremental
implementation of the checkbox.
Implications Related to Use of 2018
Method
The checkbox item was added to correct for underestimation,
and initial results showed an increase in reporting of maternal
deaths. With time, however, questions arose about whether
the increase stemmed from an unknown mixture of improved
measurement and increased misclassification (12,13,15). The
2018 method is intended to mitigate errors (14) in the pregnancy
checkbox item and provide an improved estimate of maternal
mortality. However, it does not correct all errors, nor does it
address all issues with the data. The 2018 method may result
in an underestimate of maternal mortality at ages 45 and over
and may still overestimate maternal mortality for ages 10–44. If
certifiers alter what they report in the cause-of-death statement
because of the availability of the checkbox, that might affect the
adequacy of the 2018 method. The 2018 method will not have
an impact on records where pregnancy may have contributed
to death but the certifier failed to report it in either the cause-
of-death statement or the checkbox item. Other modifications—
such as changes in ways certifiers completed cause-of-death
information on the death certificate, changes in guidance
provided to certifiers, shifts in completing death certification on
paper compared with electronic death registration, or changes
in outreach to query the quality of the information over time—
may be other factors that could potentially have influenced the
balance between improvement and misclassification captured
in the checkbox item but cannot be easily quantified. With the
exception of external causes, the 2018 coding method also does
not address cases in which the cause of death was incidental
to pregnancy (i.e., the decedent was pregnant in the last year,
but pregnancy was not a factor contributing to death). The
expectation is that more deaths are identified as maternal deaths
than appropriate in this scenario, because information on the
death certificate is typically insufficient to exclude causes that
may, in fact, be incidental.
Additional efforts will be needed to identify and correct
errors and improve reporting. Linking deaths for women of
reproductive age to birth and fetal death records as part of routine
vital statistics reporting in NVSS can help detect cases that fail
to report pregnancies in the past year as well as help investigate
checkbox-only cases that do not seem to have corroborating
indications of a pregnancy in the past year. Guidance on death
certificate reporting for certifiers can be effective, especially for
certifiers who are not familiar with the task of completing a death
certificate. A key step in any effective improvement is to ensure
that the accuracy and quality of information is incorporated into
vital statistics data as it is originally recorded.
References
1. World Health Organization. World health statistics, 2018:
Monitoring health for the SDGs, sustainable development goals.
Geneva, Switzerland. 2018. Available from: https://apps.who.int/
iris/bitstream/handle/10665/272596/9789241565585-eng.pdf.
2. Office of Disease Prevention and Health Promotion. Healthy People
2020. Maternal, infant, and child health objectives. Available from:
https://www.healthypeople.gov/2020/topics-objectives/topic/
maternal-infant-and-child-health/objectives.
3. World Health Organization, United Nations International Children’s
Emergency Fund, United Nations Fund for Population Activities,
World Bank Group, United Nations Population Division. Trends
in maternal mortality: 1990 to 2015. 2015. Available from:
https://apps.who.int/iris/bitstream/handle/10665/194254/
9789241565141_eng.pdf;jsessionid=59889EA1DABF6E
8A9D61747C035432B7?sequence=1.
4. Creanga AA. Maternal mortality in the United States: A review
of contemporary data and their limitations. Clin Obstet Gynecol
61(2):296–306. 2018.
5. MacDorman MF, Declercq E, Thoma ME. Trends in maternal
mortality by sociodemographic characteristics and cause of
death in 27 states and the District of Columbia. Obstet Gynecol
129(5):811–8. 2017.
6. MacKay AP, Rochat R, Smith JC, Berg CJ. The check box:
Determining pregnancy status to improve maternal mortality
surveillance. Am J Prev Med 19(1 Suppl):35–9. 2000.
7. Horon IL, Cheng D. Enhanced surveillance for pregnancy-
associated mortality—Maryland, 1993–1998. JAMA 285(11):
1455–9. 2001.
National Vital Statistics Reports, Vol. 69, No. 2, January 30, 2020 9
8. Building U.S. capacity to review and prevent maternal deaths.
Report from maternal mortality review committees: A view into
their critical role. 2017. Available from: https://www.cdcfoundation.
org/sites/default/files/files/MMRIAReport.pdf.
9. Zaharatos J, St Pierre A, Cornell A, Pasalic E, Goodman D. Building
U.S. capacity to review and prevent maternal deaths. J Womens
Health (Larchmt) 27(1):1–5. 2018.
10. Hoyert DL, Uddin SFG, Miniño AM. Evaluation of the pregnancy
status checkbox on the identification of maternal deaths. National
Vital Statistics Reports; vol 69 no 1. Hyattsville, MD. National
Center for Health Statistics. 2020.
11. Rossen LM, Womack LS, Hoyert DL, Anderson RN, Uddin SFG.
The impact of the pregnancy checkbox and misclassification
on maternal mortality trends in the United States, 1999–2017.
National Center for Health Statistics. Vital Health Stat 3(44). 2020.
12. Davis NL, Hoyert DL, Goodman DA, Hirai AH, Callaghan WM.
Contribution of maternal age and pregnancy checkbox on maternal
mortality ratios in the United States, 1978–2012. Am J Obstet
Gynecol 217(3):352.e1–352.e7. 2017.
13. Joseph KS, Lisonkova S, Muraca GM, Razaz N, Sabr Y, Mehrabadi
A, Schisterman EF. Factors underlying the temporal increase in
maternal mortality in the United States. Obstet Gynecol 129(1):91–
100. 2017.
14. Catalano A, Davis NL, Petersen EE, Harrison C, Kieltyka L, You
M, et al. Pregnant? Validity of the pregnancy checkbox on death
certificates in four states, and characteristics associated with
pregnancy checkbox errors. Am J Obstet Gynecol. 2019 [Epub
ahead of print].
15. MacDorman MF, Declercq E, Cabral H, Morton C. Recent increases
in the U.S. maternal mortality rate: Disentangling trends from
measurement issues. Obstet Gynecol 128(3):447–55. 2016.
16. Baeva S, Archer NP, Ruggiero K, Hall M, Stagg J, Interis EC, et al.
Maternal mortality in Texas. Am J Perinatol 34(6):614–20. 2017.
17. Kochanek KD, Murphy SL, Xu JQ, Arias E. Deaths: Final data for
2017. National Vital Statistics Reports; vol 68 no 9. Hyattsville,
MD: National Center for Health Statistics. 2019.
List of Detailed Tables
1. Maternal mortality rates and number of maternal deaths, by
race and Hispanic origin and age: United States, 2018 ...... 10
2. Maternal mortality rates and number of maternal deaths by
coding method for selected causes, by age: United States,
2018 ............................................ 11

10 National Vital Statistics Reports, Vol. 69, No. 2, January 30, 2020
Table 1. Maternal mortality rates and number of maternal deaths, by race and Hispanic origin and age: United States, 2018
[Maternal causes are those assigned to categories of the International Classification of Diseases, 10th Revision, 1992. Maternal deaths occur while pregnant or within
42 days of being pregnant. Race values are not bridged. Rates are per 100,000 live births]
Race and Hispanic origin and age
Maternal mortality (A34, O00–O95, O98–O99) Late maternal mortality (O96)
With checkbox
1
(2003–2017
coding method)
With checkbox for ages
44 and under
1
; without
checkbox for 45 and over
(2018 coding method)
With checkbox
1
(2003–2017
coding method)
With checkbox for ages
44 and under
1
; without
checkbox for 45 and over
(2018 coding method)
Rate
All persons
2
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 20.5 17.4 7.9 7.3
Under 25 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10.6 10.6 5.6 5.6
25–39 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 16.6 16.6 7.0 7.0
40 and over . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 175.7 81.9 44.1 25.2
40–44 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 82.6 82.6 26.4 26.4
45 and over . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1,315.9 * 261.1 *
Non-Hispanic white . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 18.2 14.9 8.0 7.3
Under 25 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10.5 10.5 5.6 5.6
25–39 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 13.8 13.8 6.8 6.8
40 and over . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 182.6 72.0 53.6 *
40–44 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 70.4 70.4 * *
45 and over . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1,635.9 * * *
Non-Hispanic black . . . . . . . . . . . . . . . . . . . . . . . . . . . . 43.5 37.3 14.5 13.9
Under 25 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 15.3 15.3 * *
25–39 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 38.2 38.2 14.5 14.5
40 and over . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 434.0 239.9 * *
40–44 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 243.9 243.9 * *
45 and over . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 2,431.0 * * *
Hispanic . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 13.7 11.8 5.1 4.5
Under 25 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7.6 7.6 * *
25–39 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 12.4 12.4 4.5 4.5
40 and over . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 90.0 * * *
40–44 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . * * * *
45 and over . . . . . . . . . . . . . . . . . . . . . . . . . . . . . * * * *
Number
All persons
2
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 777 658 301 277
Under 25 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 96 96 51 51
25–39 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 458 458 194 194
40 and over . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 223 104 56 32
40–44 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 97 97 31 31
45 and over . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 126 7 25 1
Non-Hispanic white . . . . . . . . . . . . . . . . . . . . . . . . . . . . 357 291 157 142
Under 25 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 41 41 22 22
25–39 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 207 207 103 103
40 and over . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 109 43 32 17
40–44 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 39 39 16 16
45 and over . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 70 4 16 1
Non-Hispanic black . . . . . . . . . . . . . . . . . . . . . . . . . . . . 240 206 80 77
Under 25 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 27 27 15 15
25–39 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 137 137 52 52
40 and over . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 76 42 13 10
40–44 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 39 39 10 10
45 and over . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 37 3 3 –
Hispanic . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 121 105 45 40
Under 25 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 21 21 11 11
25–39 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 72 72 26 26
40 and over . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 28 12 8 3
40–44 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 12 12 3 3
45 and over . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 16 – 5 –
* Rate does not meet NCHS standards of reliability.
– Quantity zero.
1
California did not have the standard checkbox item.
2
Total includes more race and Hispanic groups than shown, including more than one race.
SOURCE: NCHS, National Vital Statistics System, Mortality.

National Vital Statistics Reports, Vol. 69, No. 2, January 30, 2020 11
Table 2. Maternal mortality rates and number of maternal deaths by coding method for selected causes, by age: United States, 2018
[Maternal causes are those assigned to categories of the International Classification of Diseases, 10th Revision (ICD–10), 1992. Maternal deaths occur while pregnant or within 42 days of being pregnant]
Cause of death (based on ICD–10)
With checkbox
1
(2003–2017 coding method)
With checkbox for ages 44 and under
1
; without checkbox for
45 and over (2018 coding method)
All
persons Under 25 25–39
40 and over
All
persons Under 25 25–39
40 and over
Total 40–44
45 and
over Total 40–44
45 and
over
Rate per 100,000 live births
Maternal causes . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . (A34,O00–O95,O98–O99) 20.5 10.6 16.6 175.7 82.6 1,315.9 17.4 10.6 16.6 81.9 82.6 *
Direct obstetric causes . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . (A34, O00–O95) 15.4 7.6 12.8 126.8 68.2 846.0 13.4 7.6 12.8 67.7 68.2 *
Pregnancy with abortive outcome . . . . . . . . . . . . . . . . . . . . . . . . . . .(O00–O07) 0.8 * 0.8 * * * 0.8 * 0.8 * * *
Ectopic pregnancy . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .(O00) 0.6 * * * * * 0.6 * * * * *
Spontaneous abortion . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .(O03) * * * * * * * * * * * *
Medical abortion . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .(O04) * * * * * * * * * * * *
Other abortion . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .(O05) * * * * * * * * * * * *
Other and unspecified pregnancy with
abortive outcome . . . . . . . . . . . . . . . . . . . . . . . . . . . . . (O01–O02,O06–O07) * * * * * * * * * * * *
Other direct obstetric causes . . . . . . . . . . . . . . . . . . . . . . . . . . (A34,O10–O92) 14.1 6.6 11.7 119.7 60.5 846.0 12.1 6.6 11.7 60.7 60.5 *
Eclampsia and pre-eclampsia . . . . . . . . . . . . . . . . . . . . . . . . (O11,O13–O16) 1.0 * 1.0 * * * 0.9 * 1.0 * * *
Hemorrhage of pregnancy and childbirth
and placenta previa . . . . . . . . . . . . . . . . . . . . . . . (O20,O44–O46,O67,O72) 0.8 * 0.9 * * * 0.8 * 0.9 * * *
Complications predominantly related to
the puerperium . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . (A34,O85–O92) 1.9 * 1.9 * * * 1.9 * 1.9 * * *
Obstetrical tetanus . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . (A34) * * * * * * * * * * * *
Obstetric embolism . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .(O88) 1.2 * 1.2 * * * 1.1 * 1.2 * * *
Other complications predominantly related to
the puerperium . . . . . . . . . . . . . . . . . . . . . . . . . . . . . (O85–O87,O89–O92) 0.8 * 0.7 * * * 0.7 * 0.7 * * *
All other direct obstetric causes . . . . . . . . .(O10,O12,O21–O43,O47–O66,
O68–O71,O73–O75) 10.3 5.1 7.9 99.2 46.9 741.5 8.5 5.1 7.9 45.7 46.9 *
Obstetric death of unspecified cause . . . . . . . . . . . . . . . . . . . . . . . . . . . . .(O95) 0.6 * * * * * 0.6 * * * * *
Indirect obstetric causes . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .(O98–O99) 5.1 3.0 3.8 48.8 * 470.0 3.9 3.0 3.8 * * *
Death from any obstetric cause occurring more than 42 days
but less than 1 year after delivery . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . (O96)
2
7.9 5.6 7.0 44.1 26.4 261.1 7.3 5.6 7.0 25.2 26.4 *
See footnotes at end of table.
12 National Vital Statistics Reports, Vol. 69, No. 2, January 30, 2020
Table 2. Maternal mortality rates and number of maternal deaths by coding method for selected causes, by age: United States, 2018—Con.
[Maternal causes are those assigned to categories of the International Classification of Diseases, 10th Revision (ICD–10), 1992. Maternal deaths occur while pregnant or within 42 days of being pregnant]
Cause of death (based on ICD–10)
With checkbox
1
(2003–2017 coding method)
With checkbox for ages 44 and under
1
; without checkbox for
45 and over (2018 coding method)
All
persons Under 25 25–39
40 and over
All
persons Under 25 25–39
40 and over
Total 40–44
45 and
over Total 40–44
45 and
over
Number
Maternal causes . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .(A34,O00–O95,O98–O99) 777 96 458 223 97 126 658 96 458 104 97 7
Direct obstetric causes . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . (A34, O00–O95) 584 69 354 161 80 81 509 69 354 86 80 6
Pregnancy with abortive outcome . . . . . . . . . . . . . . . . . . . . . . . . . . .(O00–O07) 29 3 21 5 5 – 29 3 21 5 5 –
Ectopic pregnancy . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .(O00) 24 3 19 2 2 – 24 3 19 2 2 –
Spontaneous abortion . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .(O03) 2 – 1 1 1 – 2 – 1 1 1 –
Medical abortion . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .(O04) – – – – – – – – – – – –
Other abortion . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .(O05) 1 – – 1 1 – 1 – – 1 1 –
Other and unspecified pregnancy with
abortive outcome . . . . . . . . . . . . . . . . . . . . . . . . . . . . . (O01–O02,O06–O07) 2 – 1 1 1 – 2 – 1 1 1 –
Other direct obstetric causes . . . . . . . . . . . . . . . . . . . . . . . . . . (A34,O10–O92) 534 60 322 152 71 81 459 60 322 77 71 6
Eclampsia and pre-eclampsia . . . . . . . . . . . . . . . . . . . . . . . . (O11,O13–O16) 38 2 27 9 5 4 35 2 27 6 5 1
Hemorrhage of pregnancy and childbirth
and placenta previa . . . . . . . . . . . . . . . . . . . . . . . (O20,O44–O46,O67,O72) 32 2 24 6 3 3 30 2 24 4 3 1
Complications predominantly related to
the puerperium . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . (A34,O85–O92) 73 10 52 11 8 3 71 10 52 9 8 1
Obstetrical tetanus . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . (A34) – – – – – – – – – – – –
Obstetric embolism . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .(O88) 44 5 33 6 5 1 43 5 33 5 5 –
Other complications predominantly related to
the puerperium . . . . . . . . . . . . . . . . . . . . . . . . . . . . . (O85–O87,O89–O92) 29 5 19 5 3 2 28 5 19 4 3 1
All other direct obstetric causes . . . . . . . . .(O10,O12,O21–O43,O47–O66,
O68–O71,O73–O75) 391 46 219 126 55 71 323 46 219 58 55 3
Obstetric death of unspecified cause . . . . . . . . . . . . . . . . . . . . . . . . . . . . .(O95) 21 6 11 4 4 – 21 6 11 4 4 –
Indirect obstetric causes . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .(O98–O99) 193 27 104 62 17 45 149 27 104 18 17 1
Death from any obstetric cause occurring more than 42 days
but less than 1 year after delivery . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . (O96)
2
301 51 194 56 31 25 277 51 194 32 31 1
* Rate does not meet NCHS standards of reliability.
– Quantity zero.
1
California did not have the standard checkbox item.
2
Late maternal death.
SOURCE: NCHS, National Vital Statistics System, Mortality.

National Vital Statistics Reports, Vol. 69, No. 2, January 30, 2020 13
Technical Notes
Tabulations of cause-of-death statistics in this report are
based solely on the underlying cause of death. The underlying
cause is defined by the World Health Organization as “the
disease or injury which initiated the train of morbid events
leading directly to death, or the circumstances of the accident or
violence which produced the fatal injury.” The underlying cause
is selected from the conditions entered by the medical certifier
in the cause-of-death section of the death certificate. When
more than one cause or condition is entered by the medical
certifier, the underlying cause is determined by the sequence
of conditions on the certificate, provisions of the International
Classification of Diseases (ICD), and associated selection rules
and modifications. Generally, more medical information is
reported on death certificates than is directly reflected in the
underlying cause of death. This is captured in National Center for
Health Statistics’ (NCHS) multiple cause-of-death data as entity
axis and record axis data.
For the years for which data has already been released,
Figures I and II provide some examples of how the recoded data
would be presented on a data file.
Checkbox item analysis based on National
Hospital Care Survey data linked to National
Death Index
The National Hospital Care Survey (NHCS) data linked
to the National Death Index (NDI) were analyzed by NCHS as
a case study to explore the potential accuracy of use of the
pregnancy checkbox item according to maternal mortality coding
procedures in U.S. death certificates. This analysis sought to
determine potential false positive (overuse) or false negative
(underuse) uses of the pregnancy checkbox. The linked NHCS–
NDI data contain information about hospital visits (inpatient and
emergency department encounters) in the year before death for
those patients who died. The analysis was based on the premise
that for a decedent currently pregnant or pregnant in the year
before death, the pregnancy checkbox would be used as it was
intended to indicate that the decedent was currently pregnant
(checkbox value of 2), pregnant within 42 days (value of 3), or
pregnant within 43 days to 1 year (value of 4). Assuming that the
person responsible for filling out the death certificate is aware of
the decedent’s recent medical history, including pregnancy, then
the expectation is that the checkbox would be correctly used. If
no evidence existed of a current pregnancy or pregnancy within
the year prior to death, or no information about pregnancy is
available, the expectation is that the checkbox would not be
used, and a value of 1 (not pregnant), 7 (not on certificate),
8 (not applicable), or 9 (unknown if pregnant within the past
year) would be used accordingly.
This analysis assessed whether overuse or underuse of the
checkbox occurred, using this unique source of linked hospital
care and death data. Overuse was assessed by first identifying
all death records in the linked file that had a pregnancy checkbox
value indication of 2, 3, or 4. Given that these decedents were
linked to hospitalization data in the previous year, the goal
Figure I. Example of record with checkbox and mention
of pregnancy or obstetric condition in cause-of-death
statement
I a) Rupture ectopic O00.9
pregnancy
b)
c)
II
Underlying cause O00.9
Entity axis codes—First two positions indicate where the
condition was reported (i.e., which line and where on the line)
11O009
Record axis codes—Underlying cause is listed first, followed
by other codes listed alphanumerically
O009
NOTES: For this example, the record would be coded the same with or without the
checkbox. The entity and record axis codes would be the same for both the 2003–2017
and 2018 methods.
SOURCE: NCHS, National Vital Statistics System, Mortality.
Pregnancy checkbox =
Pregnant at time of
death
Figure II. Example of checkbox-only record for decedent
aged 10–44
Coding using 2003–2017 method
I a) Brain stem herniation O99.3
b) Intracerebral hemorrhage O99.4
c) Brain arteriovenous
malformation O99.8
II
Underlying cause O99.8 (Other specified
diseases and
conditions
complicating
pregnancy, childbirth
and the puerperium)
Entity axis codes—First two positions indicate where the
condition was reported (i.e., which line and where on the line)
11O993 21O994 31O998
Record axis codes—Underlying cause is listed first, followed
by other codes listed alphanumerically)
O998 O993 O994
NOTES: For this example, the record would be coded differently with or without the
checkbox. Using the 2003–2017 method, all of the codes are O codes, whereas with the
2018 method, only the underlying cause is converted to an O code.
SOURCE: NCHS, National Vital Statistics System, Mortality.
Coding using 2018 method
I a) Brain stem herniation R58
b) Intracerebral hemorrhage I71.0
c) Brain arteriovenous
malformation I70.9
II
Underlying cause I71.0 O99.4 (Diseases of
the circulatory
system complicating
pregnancy, childbirth
and the puerperium)
Entity axis codes—First two positions indicate where the
condition was reported (i.e., which line and where on the line)
11R58 21I710 31I709
Record axis codes—Underlying cause is listed first, followed
by code that would have been the underlying cause without the
checkbox, followed by other codes listed alphanumerically
O994 I7101
1
I709 R58
1
The numeral 1 in the fifth position indicated the code that would be the underlying cause
without the checkbox.
Pregnancy checkbox =
Pregnant at time of
death
Pregnancy checkbox =
Pregnant at time of
death
14 National Vital Statistics Reports, Vol. 69, No. 2, January 30, 2020
was to see if the records would have some indication of a
pregnancy-related hospital encounter, including delivery, or that
a pregnancy would be noted in their record of care for a given
inpatient or emergency department visit. Pregnancy-related
hospital encounters were defined based on any diagnosis codes
using International Classification of Diseases, Ninth Revision or
10th Revision, Clinical Modification (ICD–9–CM or ICD–10–CM)
or SNOMED for that encounter. If no indication of a pregnancy-
related diagnosis in the previous year was listed for these
decedents, then these records would be considered a potential
overuse of the pregnancy indication on the checkbox, or a
false positive use of the checkbox (i.e., the checkbox indicated
pregnancy when it should not have).
Underuse of the pregnancy indication on the checkbox
was assessed by first identifying all records of pregnancy-
related hospitalizations for persons who died within the year of
their hospitalization and then determining those records with
a pregnancy checkbox value of 1, 7, 8, or 9. Given that these
decedents had a record of a pregnancy-related hospitalization
in the previous year, the expectation is that the checkbox value
would indicate a current or recent pregnancy. Otherwise, if
no value indicating current or recent pregnancy existed in the
checkbox item, these records were considered an underuse of
the pregnancy indication of the checkbox, or a false negative
use of the checkbox (i.e., the checkbox should have indicated a
pregnancy when it did not).
The 2014 NHCS data were linked to the 2014–2015 NDI, and
2016 NHCS data were linked to the 2016–2017 NDI, to allow for an
assessment of mortality at intervals of interest (e.g., death at 30,
60, or 90 days postdischarge or 1-year survival postdischarge).
The linkage process has been detailed elsewhere: https://
www.cdc.gov/nchs/data/datalinkage/NHCS14_NDI14_15_
Methodology_Analytic_Consider.pdf and https://www.cdc.
gov/nchs/data/datalinkage/NHCS16_NDI16_17_Methodology_
Analytic_Consider.pdf.
Note that NHCS data for both 2014 and 2016 are based only
on the relatively small percentage of hospitals that responded to
the survey (16% in 2014 and 27% in 2016) and are not nationally
representative. Therefore, this case study is not intended to be
a nationally representative assessment of checkbox usage.
In addition, this analysis only includes visits that occurred at
sampled hospitals, and the possibility exists that the patient may
have been seen primarily at a nonsampled hospital during the year
before birth or that the mention of a pregnancy was omitted from
the record. Lastly, this analysis may miss cases of pregnancies
for which no event occurred necessitating a hospitalization or
emergency department visit (e.g., abortive outcomes).
Potential overuse of checkbox—false positives
To create the analytic sample to assess overuse of the
pregnancy checkbox, 150 women in the 2014 linked NHCS–NDI
and 220 women in the 2016 linked NHCS–NDI file were identified
with a checkbox value of 2, 3, or 4. In the 2014 NHCS, 81 of
the 150 decedents who were identified as pregnant within the
year before death by the checkbox (values 2, 3, or 4) had no
pregnancy-related hospital encounter within 1 year of death,
including no record of delivery. Of these 81 decedents, 32 were
under age 30, 15 were aged 30–39, and 34 were aged 40 and
over. Based on this analysis, 54% of records with a pregnancy
checkbox value indicating a current or recent pregnancy had no
pregnancy-related hospitalization nor any mention of pregnancy
in the hospitalization record in the previous year and were
considered false positives.
In the 2016 linked NHCS–NDI data, 124 of the 220 decedents
who were identified as pregnant within the year before death by
the pregnancy checkbox (values 2, 3, or 4) had no pregnancy-
related hospital encounter within 1 year of death. Of the 124
decedents, 47 were aged under 30, 36 were aged 30–39, and 41
were aged 40 and over. Based on this analysis, 56% of records
with a pregnancy checkbox value indicating a current or recent
pregnancy had no pregnancy-related hospitalization nor mention
of pregnancy in the record of hospitalization in the previous year
and were considered false positives.
Potential underuse of checkbox—false negatives
In the 2014 NHCS, 236 decedents with a pregnancy-related
hospitalization in the previous year were identified. Of these,
157 decedents had both a pregnancy-related hospital encounter
within 1 year of death and a pregnancy checkbox value of 1, 7, 8,
or 9 (not indicating pregnancy). Of the 157 decedents, 62 were
aged under 30, 62 were aged 30–39, and 33 were aged 40 and
over. Based on this analysis, 67% of 236 records of a pregnancy-
related hospitalization in the previous year did not have current
or recent pregnancy indicated by the pregnancy checkbox on the
death certificate and were considered false negatives.
In the 2016 NHCS, 253 decedents with a pregnancy-related
hospitalization in the previous year were identified. Of these,
158 had both a pregnancy-related encounter within 1 year of
death and a pregnancy checkbox value of 1, 7, 8, or 9. Of the
158 decedents, 64 were under age 30, 62 were aged 30–39, and
32 were aged 40 and over. Based on this analysis, 62% of 236
records with a pregnancy-related hospitalization in the previous
year did not have current or recent pregnancy indicated by the
pregnancy checkbox and were considered false negatives.
Summary
This analysis attempts to discern use of the pregnancy
checkbox from a data source linking hospitalization encounters
and deaths among patients. The purpose was to assess the use
of the checkbox according to whether a record of pregnancy in a
hospitalization event occurred in the period of time defined by the
checkbox (i.e., within 1 year). For both the 2014 and 2016 linked
files, approximately 53% of records were false positive cases of
pregnancy indication on the checkbox, while approximately 65%
of records were false negative cases of pregnancy indication
on the checkbox. The ability to examine use of the pregnancy
checkbox on the death certificate linked with hospitalization data
predating death provided a unique way to examine and highlight
potential misreporting of the checkbox, which may, in turn, affect
estimates of maternal mortality.
National Vital Statistics Reports, Vol. 69, No. 2, January 30, 2020 15
Late maternal deaths
Late maternal deaths (occurring between 43 days and 1 year
of death) are not included in the calculation of the official maternal
mortality rates, which are based on maternal deaths occurring
while pregnant or within 42 days of being pregnant. Late maternal
deaths are included in other maternal death measures, such as
in the calculation of pregnancy-related deaths, defined as the
death of a woman while pregnant or within 1 year of the end of a
pregnancy, as measured by the Centers for Disease Control and
Prevention’s Pregnancy Mortality Surveillance System (4). In the
National Vital Statistics System, identification of late maternal
deaths is similar to that for maternal deaths, in that the coding
procedures are based on causes of death reported on death
certificates and information on pregnancy status reported in the
checkbox item. Therefore, late maternal deaths are also affected
by the change in the coding methods.
Some late maternal deaths are identified via checkbox-only
records. In this situation, the checkbox is the only indication
of pregnancy, and the checkbox indicates that the pregnancy
occurred between 43 days and 1 year of death. In the 2018 coding
method, coding of late maternal deaths will restrict application of
the checkbox item to decedents aged 10–44 years. The checkbox
will not be applied in coding cause of death for decedents aged
45 and over. If the checkbox is the only indication of a pregnancy
for female decedents aged 10–44, a late maternal code will be
assigned as the underlying cause. However, a late maternal code
will be assigned only to the underlying cause and not to other
conditions reported on the certificate.
California data and coding methods
California has included a checkbox on the death certificate
since 2003, but it is not the one used on the U.S. Standard
Certificate of Death. The pregnancy checkbox used by California
asks only if a pregnancy occurred within the year of death and
does not differentiate timing of pregnancy. Under the 2003–2017
coding method, a positive response to this nonstandard category
without further specification of timing in the cause-of-death
statement was treated as if the pregnancy occurred between 43
days and 1 year before death (i.e., a late maternal death), and,
therefore, these deaths would not be coded as maternal deaths
or included in the calculation of the maternal mortality rate (10).
This could overestimate the number of deaths identified as late
maternal deaths and underestimate the maternal mortality rate
in California.
Application of the 2018 coding method will differ for
California compared with the rest of the jurisdictions. For
checkbox-only cases, no difference will exist between California
and the other states for women aged 45 and over, because these
cases will not be coded as maternal deaths under the 2018
coding rules. However, checkbox-only records in California
among women aged 10–44 will also not be coded as maternal
deaths, whereas they would be so coded in the other states where
the checkbox indicates a pregnancy before 43 days. Checkbox-
only deaths in California for those aged 10–44 will instead be
coded as late maternal deaths. For California and the rest of the
states, all deaths with cause-of-death information in addition to
the checkbox have the potential to be coded as maternal deaths
depending on the information included in the cause-of-death
section. The coding of the cause will follow usual coding and
use information from the checkbox, if available, to determine
timing. Quantifying the impact of coding all California checkbox-
only deaths as late maternal deaths on the maternal mortality
rate is difficult, but it is plausible that the national maternal
mortality rate may be somewhat underestimated. California will
begin using the standard checkbox in 2020, and changes in the
national maternal mortality rate as a result of this changeover
will be evaluated upon release of the 2020 data.
Race and Hispanic origin
The 2003 revision of the U.S. Standard Certificate of Death
allows the reporting of more than one race (multiple races), in
accordance with the revised standards issued by the Office of
Management and Budget in 1997. Information on this change
is presented elsewhere (17). The number of states reporting
multiple races increased over time, so that by midyear 2017,
all were reporting multiple races. To provide uniformity and
comparability of the data before all areas have data in multiple-
race format, the responses of those for whom more than one
race was reported (multiple races) were bridged to a single race.
The bridging procedure for multiple-race women is similar to the
procedure used to bridge the multiple-race population estimates.
Information detailing the processing and tabulation of data by
race is presented elsewhere (see https://www.cdc.gov/nchs/
data/dvs/Multiple_race_documentation_5-10-04.pdf).
Race and Hispanic origin are two distinct attributes and
are reported separately on the death certificate. Data shown for
Hispanic women include women of any race. Hispanic origin is
not imputed if it is not reported.
This report presents data by single-race group when only
one race was reported. A separate report (10) on maternal
mortality presented data for earlier years and showed data
by bridged race. The following Table is similar to Table 1 but
presents the information using bridged data.
Random variation
Mortality data are not subject to sampling error but may
be affected by random variation. That is, the number of deaths
that actually occurred may be considered as one of a large
series of possible results that could have arisen under the same
circumstances; see Technical Notes (17) for more complete
discussion of random variation, confidence intervals, and
statistical tests for rates.
Suppression of unreliable rates—An asterisk is shown in
place of a mortality rate based on fewer than 20 deaths, the
equivalent of a relative standard error of 23% or more. The
minimum of 20 deaths is the current standard for NCHS’ Division
of Vital Statistics, below which rates are considered to be too
statistically unreliable for presentation.
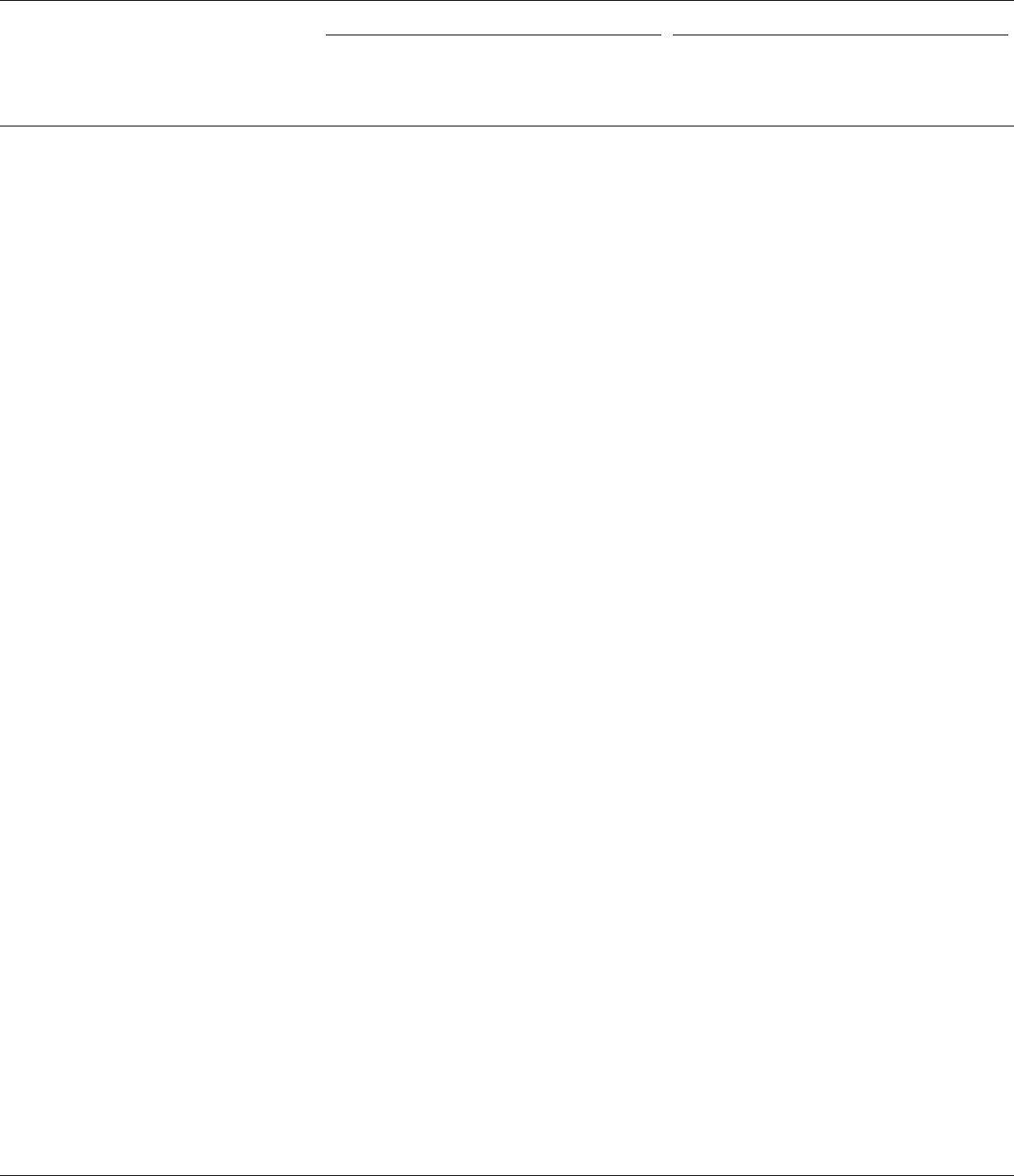
16 National Vital Statistics Reports, Vol. 69, No. 2, January 30, 2020
Table. Maternal mortality rates and maternal deaths, by bridged race and Hispanic origin and age: United States, 2018
[Maternal causes are those assigned to categories of the International Classification of Diseases, 10th Revision, 1992. Maternal deaths occur while pregnant or within
42 days of being pregnant. Race values are bridged. Rates are per 100,000 live births]
Race and Hispanic origin and age
Maternal mortality (A34, O00–O95, O98–O99) Late maternal mortality (O96)
With checkbox
1
(2003–2017
coding method)
With checkbox for ages
44 and under
1
; without
checkbox for 45 and over
(2018 coding method)
With checkbox
1
(2003–2017
coding method)
With checkbox for ages
44 and under
1
; without
checkbox for 45 and over
(2018 coding method)
Rate
All persons
2
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 20.5 17.4 7.9 7.3
Under 25 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10.6 10.6 5.6 5.6
25–39 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 16.6 16.6 7.0 7.0
40 and over . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 175.7 81.9 44.1 25.2
40–44 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 82.6 82.6 26.4 26.4
45 and over . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1,315.9 * 261.1 *
Non-Hispanic white . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 18.1 14.8 7.9 7.2
Under 25 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10.4 10.4 5.4 5.4
25–39 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 13.7 13.7 6.8 6.8
40 and over . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 179.6 70.8 52.7 *
40–44 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 69.2 69.2 * *
45 and over . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1,609.6 * * *
Non-Hispanic black . . . . . . . . . . . . . . . . . . . . . . . . . . . . 42.1 36.3 14.0 13.5
Under 25 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 14.9 14.9 * *
25–39 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 37.5 37.5 14.2 14.2
40 and over . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 421.1 232.7 * *
40–44 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 236.6 236.6 * *
45 and over . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 2,368.8 * * *
Hispanic . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 13.7 11.8 5.1 4.5
Under 25 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7.6 7.6 * *
25–39 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 12.4 12.4 4.5 4.5
40 and over . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 90.0 * * *
40–44 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . * * * *
45 and over . . . . . . . . . . . . . . . . . . . . . . . . . . . . . * * * *
Number
All persons
2
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 777 658 301 277
Under 25 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 96 96 51 51
25–39 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 458 458 194 194
40 and over . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 223 104 56 32
40–44 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 97 97 31 31
45 and over . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 126 7 25 1
Non-Hispanic white . . . . . . . . . . . . . . . . . . . . . . . . . . . . 361 295 158 143
Under 25 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 42 42 22 22
25–39 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 210 210 104 104
40 and over . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 109 43 32 17
40–44 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 39 39 16 16
45 and over . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 70 4 16 1
Non-Hispanic black . . . . . . . . . . . . . . . . . . . . . . . . . . . . 244 210 81 78
Under 25 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 28 28 15 15
25–39 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 140 140 53 53
40 and over . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 76 42 13 10
40–44 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 39 39 10 10
45 and over . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 37 3 3 –
Hispanic . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 121 105 45 40
Under 25 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 21 21 11 11
25–39 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 72 72 26 26
40 and over . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 28 12 8 3
40–44 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 12 12 3 3
45 and over . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 16 – 5 –
* Rate does not meet NCHS standards of reliability.
– Quantity zero
1
California did not have the standard checkbox item.
2
Total includes more race and Hispanic groups than shown.
SOURCE: NCHS, National Vital Statistics System, Mortality.

National Vital
Statistics Reports
Volume 69, Number 1 January 30, 2020
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES
Centers for Disease Control and Prevention
National Center for Health Statistics
National Vital Statistics System
NCHS reports can be downloaded from: https://www.cdc.gov/nchs/products/index.htm.
Evaluation of the Pregnancy Status Checkbox on
the Identification of Maternal Deaths
by Donna L. Hoyert, Ph.D., Division of Vital Statistics, Sayeedha F.G. Uddin, M.D., M.P.H., Office of the
Director, and Arialdi M. Miniño, M.P.H., Division of Vital Statistics
Keywords: maternal mortality • death certificate • National Vital
Statistics System
Introduction
Maternal mortality has historically been used as a key
indicator of the health of a population. Currently, it is one of a
limited number of health indicators included in the Sustainable
Development Goals that address countries’ success in improving
human wellbeing without harming the environment (1). In the
United States, the U.S. National Vital Statistics System (NVSS)
at the National Center for Health Statistics (NCHS) generates the
official mortality statistics, including maternal mortality rates,
that are used within the United States and internationally. NVSS
identifies deaths of pregnant or recently pregnant women using
information reported on the women’s death certificates.
NVSS follows guidance from the World Health Organization’s
(WHO) International Classification of Diseases, 10th Revision
(ICD–10) and uses ICD terminology when identifying maternal
deaths (Figure 1) (2,3). The WHO definition of maternal deaths
does not include late maternal deaths, which are defined as
deaths with a pregnancy occurring 43 days to 1 year before the
death.
Adoption of pregnancy status checkbox item
Research before 2003 (4–7) noted that NVSS underestimated
maternal mortality when compared with other data sources
and that identification of these deaths could be improved with
additional effort. One approach some states took to improve
identification of maternal deaths was to add pregnancy status
indicators to their death certificates. However, these indicators
were not standardized or consistent across the states that
adopted them. McKay et al. (4), using early 1990s death
certificate data from 16 states, found that 29% of deaths among
females occurring within 1 year of pregnancy could be identified
Abstract
Objectives—This report quantifies the impact of the
inclusion of a pregnancy status checkbox item on the U.S.
Standard Certificate of Death on the number of deaths classified
as maternal. Maternal mortality rates calculated with and without
using the checkbox information for deaths in 2015 and 2016 are
presented.
Methods—This report is based on cause-of-death
information from 2015 and 2016 death certificates collected
through the National Vital Statistics System. Records originally
assigned to a specified range of ICD–10 codes (i.e., A34,
O00–O99) when using information from the checkbox item
were recoded without using the checkbox item. Ratios of deaths
assigned as maternal deaths using checkbox item information
to deaths assigned without checkbox item information were
calculated to quantify the impact of the pregnancy status
checkbox item on the classification of maternal deaths for 47
states and the District of Columbia. Maternal mortality rates for
all jurisdictions calculated using cause-of-death information
entered on the certificate with and without the checkbox were
compared overall and by characteristics of the decedent.
Results—Use of information from the checkbox, along with
information from the cause-of-death section of the certificate,
identified 1,527 deaths as maternal compared with 498 without
the checkbox in 2015 and 2016 (ratio = 3.07), with the impact
varying by characteristics of the decedent such as age at death.
The ratio for women under age 25 was 2.15 (204 compared with
95 deaths) but was 14.14 (523 compared with 37 deaths) for
women aged 40–54. Without the adoption of the checkbox item,
maternal mortality rates in both 2015 and 2016 would have been
reported as 8.7 deaths per 100,000 live births compared with 8.9
in 2002. With the checkbox, the maternal mortality rate would be
reported as 20.9 and 21.8 deaths per 100,000 live births in 2015
and 2016.
Maternal Mortality
Statistics
NEW
To access other NCHS reports about maternal mortality,
public-use data files, and resources, visit
https://www.cdc.gov/nchs/maternal-mortality/.
CS313496

FIRST CLASS MAIL
POSTAGE & FEES PAID
CDC/NCHS
PERMIT NO. G-284
National Vital Statistics Reports, Vol. 69, No. 2, January 30, 2020
U.S. DEPARTMENT OF
HEALTH & HUMAN SERVICES
Centers for Disease Control and Prevention
National Center for Health Statistics
3311 Toledo Road, Room 4551
Hyattsville, MD 20782–2064
OFFICIAL BUSINESS
PENALTY FOR PRIVATE USE, $300
For more NCHS NVSRs, visit:
https://www.cdc.gov/nchs/products/nvsr.htm.
For e-mail updates on NCHS publication releases, subscribe online at: https://www.cdc.gov/nchs/govdelivery.htm.
For questions or general information about NCHS: Tel: 1–800–CDC–INFO (1–800–232–4636) • TTY: 1–888–232–6348
Internet: https://www.cdc.gov/nchs • Online request form: https://www.cdc.gov/info
DHHS Publication No. 2020–1120 • CS314215
Contents
Abstract .......................................................1
Introduction ....................................................1
Evidence and Effects of Checkbox Errors ..............................2
New Approach for Coding Maternal Deaths: Description of 2018 Method .....3
Maternal Mortality in 2018 .........................................4
Results From 2018 Method Compared With 2003–2017 Method ...........5
Comparison of Rates With Those of Pre-checkbox Era ...................6
Maternal Mortality Data Release Moving Forward .......................7
Implications Related to Use of 2018 Method ..........................8
References .....................................................8
List of Detailed Tables ............................................9
Technical Notes ................................................13
Acknowledgments
This report was prepared in the Division of Vital Statistics (DVS) under the
direction of Steven Schwartz, Director, DVS; Hanyu Ni, Associate Director
for Science, DVS; and Robert N. Anderson, Chief, Mortality Statistics Branch
(MSB). Rajesh Virkar, Chief, Information Technology Branch (ITB), and Joseph
Bohn (ITB) provided computer programming support and prepared the data file.
Medical coders in the Data Acquisition, Classification and Evaluation Branch and
nosologists in MSB provided coding support. Lisa Mirel, Division of Analysis and
Epidemiology, provided data analysis based on National Hospital Care Survey–
National Death Index linked data. Brady Hamilton (DVS) provided information on
births by detailed age. Isabelle L. Horon (DVS) and Amy Branum, NCHS Acting
Associate Director for Science, reviewed and provided comments on earlier
report drafts. The report was edited and produced by NCHS Office of Information
Services, Information Design and Publishing Staff: Jane Sudol edited the report,
and typesetting and graphics were done by Michael W. Jones (contractor).
Suggested citation
Hoyert DL, Miniño AM. Maternal mortality in the
United States: Changes in coding, publication,
and data release, 2018. National Vital Statistics
Reports; vol 69 no 2. Hyattsville, MD: National
Center for Health Statistics. 2020.
Copyright information
All material appearing in this report is in
the public domain and may be reproduced
or copied without permission; citation as to
source, however, is appreciated.
National Center for Health Statistics
Jennifer H. Madans, Ph.D., Acting Director
Amy M. Branum, Ph.D., Acting Associate
Director for Science
Division of Vital Statistics
Steven Schwartz, Ph.D., Director
Hanyu Ni, Ph.D., M.P.H., Associate Director
for Science
