
BRIEFING
EPRS | European Parliamentary Research Service
Author: Nicole Scholz
Members' Research Service
PE 646.363 – April 2020
EN
Organ donation and transplantation
Facts, figures and European Union action
SUMMARY
The issue of organ donation and transplantation gained renewed political momentum as one of the
initial health priorities of the current Croatian Presidency of the Council of the EU.
There are two types of organ donation: deceased donation and living donation. Organ
transplantation has become an established worldwide practice, and is seen as one of the greatest
medical advances of the 20th century. Demand for organ transplantation is increasing, but a
shortage of donors has resulted in high numbers of patients on waiting lists.
Medical, legal, religious, cultural, and ethical considerations apply to organ donation and
transplantation. In the EU, transplants must be carried out in a manner that shows respect for
fundamental rights and for the human body, in conformity with the Council of Europe's binding
laws, and compliant with relevant EU rules. World Health Organization principles also apply.
Organ donation rates across the EU vary widely. Member States have different systems in place to
seek people's consent to donate their organs after death. In the 'opt-in' system, consent has to be
given explicitly, while in the 'opt-out' system, silence is tantamount to consent. Some countries have
donor and/or non-donor registries.
Responsibility for framing health policies and organising and delivering care lies primarily with the
EU Member States. The EU has nevertheless addressed organ donation and transplantation through
legislation, an action plan and co-funded projects, and the European Parliament has adopted own-
initiative resolutions on aspects of organ donation and transplantation.
Stakeholders have submitted a joint statement on a shared vision for improving organ donation and
transplantation in the EU. An evaluation of the EU's action plan identified the need for a new,
improved approach. Innovative products and procedures, such as artificially grown organs and 3D
bio-printing, might lend themselves as future possibilities to reduce our reliance on organ donors.
In this Briefing
Bolstering cooperation to save lives
Organ donation and transplantation basics
EU policy and action
International and European organisations
Stakeholders' views
Looking ahead

EPRS | European Parliamentary Research Service
2
Glossary
Donor after brain death (DBD): a deceased donor for whom death has been determined by neurological
criteria. Also referred to as deceased heart-beating donor.
Donor after circulatory death (DCD): a deceased organ donor for whom death has been determined by
circulatory and respiratory criteria. Also referred to as deceased non-heart-beating donor.
Living donor: a living human being from whom cells, tissue or organs have been removed for the purpose of
transplantation.
Transplantation: the transfer (engraftment) of human cells, tissues or organs from a donor to a recipient with
the aim of restoring function(s) in the body. When transplantation is performed between different species (for
instance, animal to human), it is referred to as xenotransplantation.
Source: Global Glossary of Terms and Definitions on Donation and Transplantation, WHO; Newsletter
Transplant 2019, EDQM/Council of Europe.
Bolstering cooperation to save lives
The issue of organ donation and transplantation is back on the political agenda. As one of the initial
health priorities of the current Croatian Presidency of the Council of the EU, it was included in the
18-month 'trio' programme prepared by the current and two preceding presidencies (Romania and
Finland), which noted that 'cooperation in the field of transplantation and organ donation at EU
level can be strengthened to save lives'. The Croatian Presidency stated in its
programme that, based
on Croatia's positive experience with organ donation and transplantation, it would make 'special
efforts to explore the possibilities of closer and improved cooperation among Member States'.
Organ donation and transplantation basics
Organ donation can be defined as the act of giving one or more organs (or parts thereof), without
compensation, for transplantation into someone else. There are two types of organ donation:
deceased donation and living donation. This means that donated organs come from either a
deceased or a living donor, giving rise, respectively, to deceased-donor and living-donor
transplants. There are two categories of deceased donor: those where donation takes place after
brain death and those where it takes place after circulatory death (see Glossary). The objective of
organ donation is to greatly enhance – or save – the life of the person who receives the transplanted
organ; organ transplantation is often the
only treatment for end-stage organ failure, such as liver
and heart failure. Since the first successful kidney transplant in the United States in 1954, organ
transplantation has become an established worldwide practice considered to be one of the 20th
century's
exceptional medical advances. Demand for organ transplantation is increasing, but there
are not enough organs available to meet the need. Shortage of donors is considered to be a major
limiting factor in treating patients with chronic organ failure, and has resulted in long waiting lists
for patients.
Ethical considerations and fundamental human rights
There are a number of medical, legal, religious, cultural and ethical considerations associated with
organ donation and transplant. In addition to being a life-saving practice, organ donation is often
regarded as an expression of human solidarity. It is considered to be consistent with
the beliefs of
most major religions, including Roman Catholicism, Islam, most branches of Judaism and most
Protestant faiths. According to the United Network for Organ Sharing (UNOS), research has shown
that, unless a religious group has taken action to prohibit organ donation and transplantation, it is
assumed that such donation is permissible: 'Donation is encouraged as a charitable act that saves or
enhances life; therefore, it requires no action on the part of the religious group. Although this is a

Organ donation and transplantation
3
passive approach to affirming organ and tissue donation and transplantation, it seems to be the
position of a large population of the religious community'.
According to the Council of Europe's Guide to the quality and safety of organs for transplantation
,
the handling and disposal of human organs must be carried out in a manner that shows respect for
fundamental rights and for the human body. Moreover, ethical standards of all aspects of organ
donation and transplantation must conform to the
Oviedo Convention on Human Rights and
Biomedicine and the Additional Protocol on the transplantation of organs and tissues of human
origin (see the Council of Europe section below). EU Member States must also comply with the
relevant EU rules (see below under EU policy and action). As the Council of Europe's guide notes,
other important guidelines to be respected from an ethical point of view include the WHO Guiding
Principles on Human Cell, Tissue and Organ Transplantation and the Declaration of Istanbul on
organ trafficking and transplant tourism (see
World Health Organization). A 2012 review article on
international practices of organ donation highlights the following main points: deceased donation
rates vary markedly around the world; living donation is the mainstay of transplantation in many
countries; many of the unacceptable transplantation practices stem from the exploitation of
vulnerable living donors; and all developments in donation should have equity, quality, and safety
at their core.
Donation and transplantation activity in Europe
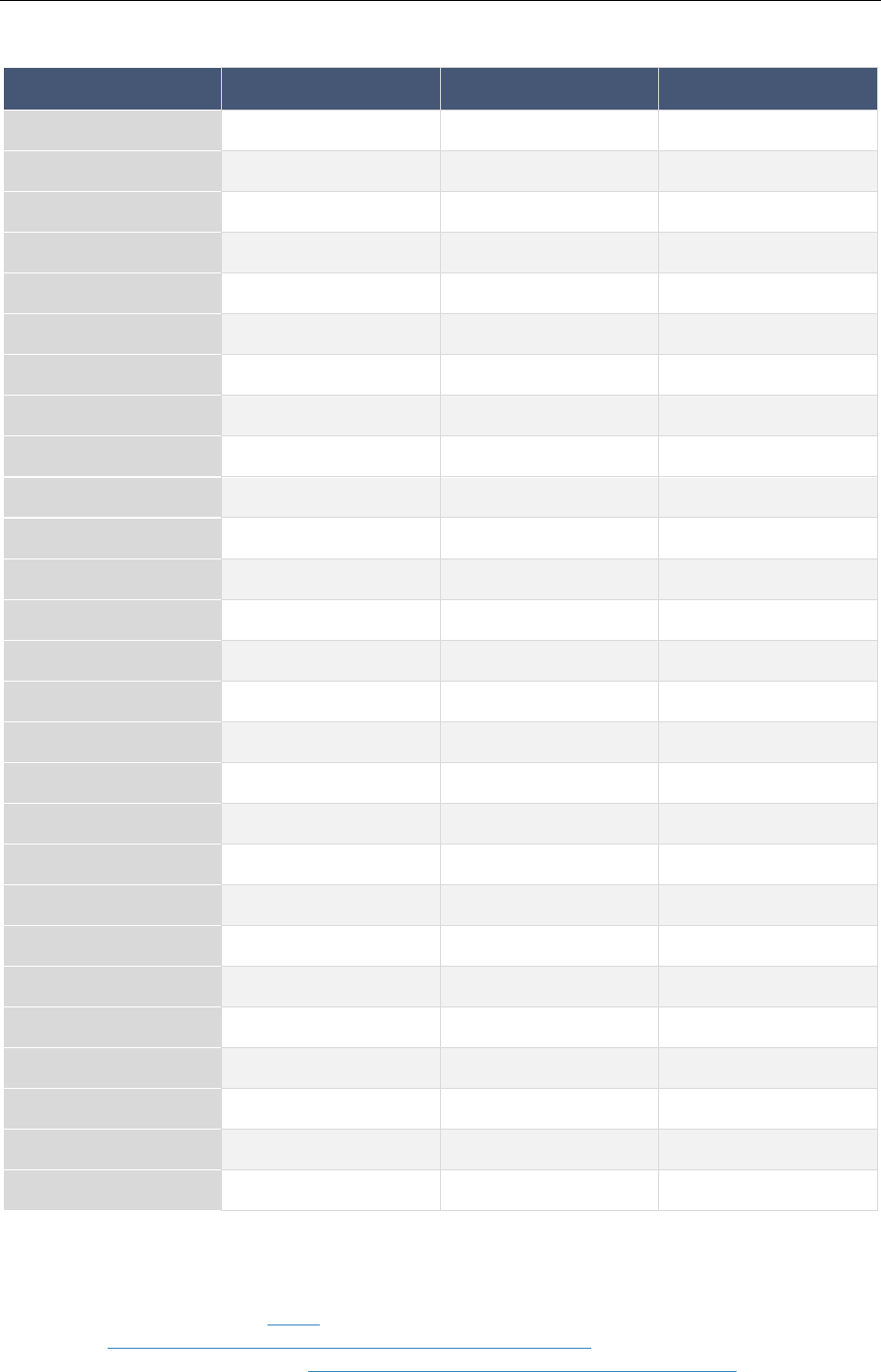
The most frequently transplanted organs in the EU are kidneys (see Table 1). Other commonly
transplanted organs include livers, hearts and lungs. The small bowel and pancreas can also be
transplanted. New types of transplantation are meanwhile being developed all the time.
Table 1 – Number of organs transplanted in 2018 (in 28 EU countries, 509.7 million inhabitants)
Kidney
Liver
Heart
Lung
Pancreas
Small
bowel
Total organs
transplanted
21 227
(19.9 % from
living donors)
7 940
(2.8 % from
living donors)
2 287
1 980
745
42
34 221
Source: Newsletter Transplant 2019, EDQM, Council of Europe.
Nowadays in Europe, the main source of transplantable organs is donations from donors after brain
death, ahead of those from donors after circulatory death and from living donors. According to the
European Commission's 2017
study on the uptake and impact of the EU action plan on organ
donation and transplantation (2009-2015) in the EU Member States, deceased donation is a source
for kidney, liver, heart, lung, pancreas and small bowel transplants. Living donation is mainly
performed for kidney transplants and some liver transplants. Demand for organs exceeds the
number of organs available. In 2018, over
150 000 patients in Europe were registered on organ
waiting lists. Organ donation rates for both deceased and living donation vary widely across the EU.
In 2018, the number of actual deceased donors
1
ranged from 48.3 per million people in Spain, 40.2
per million in Croatia and 33.4 per million in Portugal, to 0.5 per million in Romania (see Figure 1).
Living organ donation practices vary, too. In a 2013 online survey
, large discrepancies were found
between geographical regions of Europe (eastern, Mediterranean and north-western).

EPRS | European Parliamentary Research Service
4
Figure 1 – Actual deceased organ donors 2018 (annual rate per million population)
Data source: Newsletter Transplant, EDQM, Council of Europe. Graphic by Samy Chahri, EPRS.
Consent systems: Opting in versus opting out
EU Member States have differing national (and sometimes regional) systems enabling people to
consent to donating organs after death. Under the 'opt-in' system (also called 'explicit consent' or
'informed consent' system), consent has to be given explicitly. The 'opt-out' system endorses the
principle of 'presumed consent' (silence being tantamount to consent) unless a specific request for
non-removal of organs for donation is made before death. There are also mixed systems. Some
countries have developed donor and/or non-donor registries where citizens can record their wishes
in this regard (see Table 2). In practice, operational variations
exist, as the family of the deceased still
plays a prominent role in the decision-making. The opt-out system is often considered to be a
contributing factor to higher donation rates. Increasing organ donation by adopting an opt-out
system is widely debated among the public and politicians. In this context, a recent
study comparing
opt-in and opt-out systems in 35 similar countries registered with the Organisation for Economic
Co-operation and Development (OECD) found no significant difference in deceased-donor rates; a
reduction in living-donor numbers in the opt-out countries was nevertheless observed. The authors
suggest that 'other barriers to organ donation must be addressed, even in settings where consent
for donation is presumed', and conclude that 'greater emphasis on education and informing the
general population about the benefits of transplantation is the preferred way to achieve an increase
in organ donation'. In this context, a 2016
commentary looks at whether the concept of 'nudging'
deceased donation through an opt-out system constitutes a libertarian approach or manipulation.
Organ donation and transplantation
5
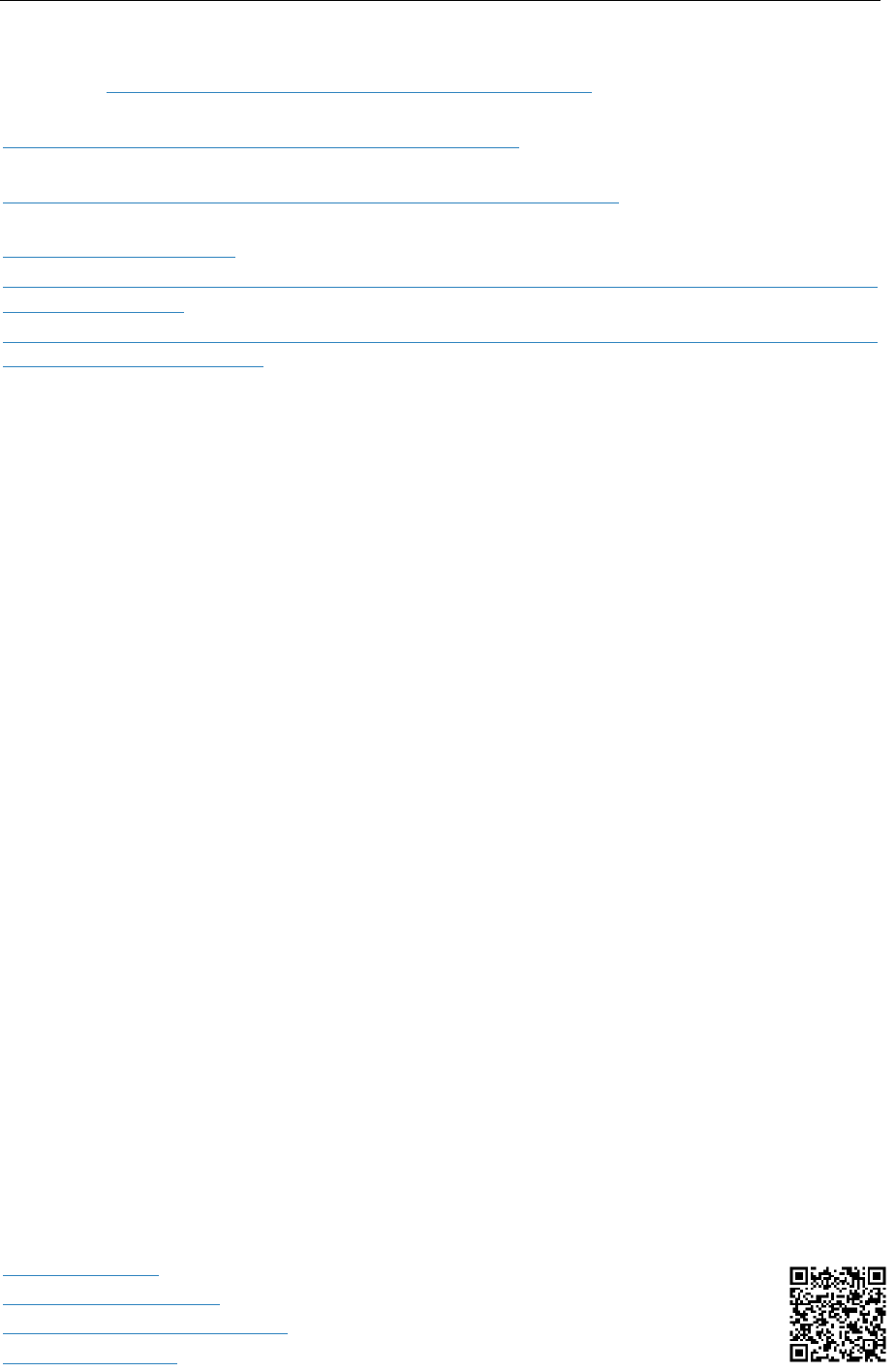
Table 2 – Opting in versus opting out: organ donation from deceased persons in the EU
Country
Consent system
Donor registry
Non-donor registry
Austria
opt-out
x
Belgium
opt-out
*
x
Bulgaria
opt-out
x
Croatia
opt-out
x
Cyprus
opt-in
x
Czechia
opt-out
x
Denmark
opt-in
x
x
Estonia
opt-out
x*
x*
Finland
opt-out
n/a
n/a
France
opt-out
x
Germany
opt-in
Greece
opt-out
x
Hungary
opt-out
x
Ireland
opt-in
n/a
n/a
Italy
opt-out
x
x
Latvia
opt-out
x
x
Lithuania
opt-in
x
*
Luxembourg
opt-out
n/a
n/a
Malta
opt-out
x
Netherlands
opt-in
x
x
Poland
opt-out
x
Portugal
opt-out
x
Romania
opt-in
x
Slovakia
opt-out
x
Slovenia
mixed system
x
x
Spain
opt-out
x
x
Sweden
opt-out
x
x
n/a: data not available.
Note: Spain has an advanced directives registry where persons can register their desire (or otherwise) to
become an organ donor after death.
* th
e data regarding the existence of (non-)donor registries taken from the data source for this table differ
from the results of a 2019 EDQM survey
.
Data source: Guide to the quality and safety of organs for transplantation, EDQM, Council of Europe, 2018 (as
adapted from the Commission's 2017 study on the uptake and impact of the EU action plan).

EPRS | European Parliamentary Research Service
6
EU public opinion on organ donation and transplantation
A 2009 Special Eurobarometer survey on behaviours and attitudes in relation to organ donation and
transplantation showed that the majority of EU citizens supported organ donation, with 55 %
expressing their willingness to donate their own organs after death, and 53 % willing to consent to
donate organs of deceased close family members. According to the survey
report, distrust of the
system (either the transplantation system, the consent system, and/or general social system) and
fear of manipulation of the human body were the main reasons for people not wanting to donate
their own organs or those of a deceased
close family member. More specifically, the
results showed that some 40 % of EU
citizens had talked about organ donation
and transplantation with their family (as
explained in the report, discussion of this
topic within families correlated positively
with support for organ donation). Support
levels for organ donation were generally
higher in the countries that joined the EU
before 2004 than in those that joined after
2004. Education level was also noted as a
key factor influencing support for organ donation. This factor interlinked with several others,
including the fact that certain age groups and regions of Europe that had more limited access to
higher education tended to have lower levels of discussion, awareness and support for organ
donation. Finally, financial hardship and self-described social position appeared to be a barrier to
support for organ donation. Respondents who reported having difficulty paying bills were less likely
to discuss organ donation with their families, or to give their consent to donation, compared to
those who hardly ever experienced this difficulty. Similarly, respondents who ranked themselves
lower on the social ladder were less likely to discuss this topic or to give their consent than those
who gave themselves a higher social ranking.
EU policy and action
The European Parliament has adopted own-initiative resolutions on various aspects of organ
donation and transplantation. In its 2008 resolution on policy actions at EU level, Parliament
considered that the main challenge facing EU Member States with regard to organ transplantation
was to reduce the organ and donor shortage. The resolution stressed that one highly effective way
to increase organ availability was to provide the public with more information. It proposed
establishing a 24-hour transplant hotline with a single telephone number managed by a national
transplantation organisation, to provide rapid, relevant and accurate information. It also called for
the introduction of a European donor card, complementary to existing national systems, and
recognised the need to reduce transplant risks. In its 2012 resolution on voluntary and unpaid
donation of tissues and cells, Parliament stressed, among other things, the importance of non-
remuneration, consent, and protection of living donors' health, underlining the need for anonymity,
traceability and transparency. It called on Member States to step up their information and
awareness-raising campaigns to promote the donation of tissue and cells, and to ensure the
provision of clear, fair and scientifically based medical information enabling the public to make
informed choices. It also asked for reinforced exchange of best practice and strengthened
cooperation. In its 2013 resolution on organ harvesting in China, Parliament expressed its concern
at reports of systematic, state-sanctioned organ harvesting from non-consenting prisoners of
conscience in the People's Republic, and called for the EU and its Member States to raise the issue
in China.
Denmark: from motivation to acceptability
A 2016 survey of public attitudes towards organ
donation in Denmark identified a shift over the
previous three decades from marked opposition to
organ transplantation to strong support for it. The
authors called for
comparative studies in other
countries to generate a better overall understanding of
the conditions of acceptability that needed to be in
place to ensure the long-term social robustness of
organ donation.

Organ donation and transplantation
7
The main responsibility for shaping health policies and organising and delivering care lies primarily
with the EU Member States. The EU has however addressed the issue of organ donation and
transplantation through legislation, an action plan and co-funded projects.
The EU can adopt measures setting high quality and safety standards for substances of human
origin, such as blood, organs, tissues and cells (Article 168
of the Treaty on the Functioning of the
EU). EU rules on organ donation and transplantation are set out in Directive 2010/45/EU (the
'European Organs Directive'). This directive lays down the quality and safety standards for organs
intended for transplantation, covering all stages of the process – from donation, procurement and
handling to transplantation.
Commission Directive 2012/25/EU regarding information procedures
for the cross-border exchange between Member States of human organs intended for
transplantation helps to implement the European Organs Directive. National
competent authorities
are responsible for implementing the requirements established by EU legislation. The European
Commission holds regular
meetings with these authorities to facilitate the exchange of best
practice. Moreover, the competent authorities occasionally adopt statements on topics of common
concern, such as the May 2018
statement on the proposed Global Kidney Exchange concept. As the
Commission has pointed out, experience shows that some organisational models perform better
than others. Identifying those elements that could be promoted at EU level would bring
European
added value, in particular for Member States with less developed organ donation and
transplantation systems. Patients that cannot be adequately treated in small Member States with a
limited donor pool could thereby benefit from EU action.
The EU action plan on organ donation and transplantation (2009-2015) was designed increase organ
availability; enhance the efficiency and accessibility of transplant systems, and improve the quality
and safety of procedures. The Commission's 2013
mid-term review of the action plan found that the
EU Member States had made good progress thus far. The main achievements related to the
increased number and improved training of
donor transplant coordinators, the
introduction or development of living
donation programmes in some Member
States, and improvements in organisational
models. According to the mid-term review,
in the remaining period efforts would be
focused on living donation programmes
and on the cross-border exchange of
organs.
The action plan's mid-term review reflected
the December 2012 Council conclusions
on
organ donation and transplantation:
recalling the main principles and objectives,
the Council acknowledged the Member
States' endeavours to meet the three
challenges set by the action plan. Among
other things, it welcomed the efforts made
to further develop living donation
programmes, the establishment of bilateral
and multilateral agreements between
countries, and the sharing of good practice.
The Council nevertheless saw room for
improvement. It underlined the importance
of transparent and comprehensive
communication to strengthen public trust in
the value of transplant systems, and of
Sharing best practice
Organ donation and transplant medicine is one of the
areas of work of the South-Eastern Europe Health
Network (SEEHN
), a multi-governmental forum for
regional collaboration on health, comprising Albania,
Bosnia and Herzegovina, Bulgaria, Croatia, Israel,
Moldova, Montenegro, North Macedonia, Romania
and Serbia. Within SEEHN, regional health
development centres (RHDC) transform regional
projects into long-term programmes. Headquartered
in Zagreb, Croatia, the
RHDC on organ donation and
transplantation supports cooperation within SEEHN
countries and facilitates the dissemination and
exchange of good practice.
National reform efforts in three leading countries for
organ donation reform – Spain, Croatia and Portugal –
are described in a 2013 paper on
international
approaches to organ donation reform. Also of note are
the individual papers on the development of donation
after circulatory death in Spain, and how Spain reached
40 deceased organ donors per million population; the
development of the Croatian model of organ donation
and transplantation; and organ donation: the reality of
an intensive care unit in Portugal.
Among the countries with the highest deceased donor
rates is also Belgium, where transplantation activities
were initiated in the early 1960s.

EPRS | European Parliamentary Research Service
8
encouraging people to become organ donors after death. It invited countries to share expertise on
several topics, such as expanded criteria for donors (for instance, older donors) so as to increase the
number of available organs.
The Commission's 2017 study on the uptake and impact of the EU action plan
found that the action
plan helped countries set a shared agenda in organ donation, facilitated EU-wide collaboration, and
was most effective for actions that were clearly defined and implied tangible changes in organ
donation. According to the study, many Member States expressed the view that the action plan
helped improve their policies on organ donation, and many considered there was a need for a new,
improved action plan (for more on this see '
Looking ahead' below).
In more concrete terms, the study found that the action plan resulted in a considerable increase in
organ donation and transplantation in the EU over its period of implementation. Between 2008 and
2015, the number of organ donors at EU level increased from 12 000 to nearly 15 000 (a 21 %
increase). This surge in donation rates
resulted in 4 600 additional transplant
operations (a 17 % increase). Kidney
transplants accounted for 60 % of the
increase, liver transplants for 24 %, and heart
transplants for 11 %. Significant variations
were nevertheless observed between
Member States, and rates even decreased in
some countries. The study also highlighted
that – despite the overall progress – by the
end of 2015, the demand for organs in the
EU continued to outstrip supply in all
countries, with thousands of people still
waiting for a transplant. Furthermore,
according to the study, the action plan also
showed that the cross-border exchange of
organs played an important role in
optimising the use of the limited number of
available organs. It found that, while the
majority of cross-border exchanges took
place within European organ exchange
organisations (see text box), many Member
States set up direct collaborations by means
of bilateral agreements
on organ exchange,
such as those between Italy and Malta,
2
and
Spain and Portugal.
3
Cross-border
agreements enabled some countries to
become more specialised in specific
transplantation procedures (for instance,
lung transplants for Austria and Belgium) –
an expertise from which other countries
could then benefit.
In the 2009 to 2015 period, several countries also started using a common organ exchange platform
developed in the course of the EU-funded joint action FOEDUS
(facilitating exchange of organs
donated in EU Member States, 2013-2016). The FOEDUS platform makes it possible for allocation
bodies to offer 'surplus organs' (organs that are difficult to match to recipients in their own country),
and inversely, to get access to offers from surplus organs donated in other countries. This often
concerns children.
As of February 2019, 13 countries had access to the exchange platform, and two
countries had applied to join. The most active EU countries in terms of offering organs through the
European organ exchange organisations
Eurotransplant is a non-
profit international
organisation that facilitates the allocation and cross-
border exchange of deceased donor organs. Eight
countries cooperate within Eurotransplant (Austria,
Belgium, Croatia, Germany, Hungary, Luxemburg,
Netherlands and Slovenia), covering a population of
roughly 137 million people. The organisation allocates
more than 7 000 organs per year, and there are about
14 000 patients on waiting lists for a donor organ. In
2019, the percentage of organs exchanged cross-
border was around
21.5 % of all organs transplanted
(see the statistics library for numbers per country).
Scandiatransplant is the organ exchange organisation
for Denmark, Finland, Iceland, Norway, Sweden and
Estonia (associate member). It is owned by the full
member hospitals performing organ transplantation in
these countries, and covers a population of
approximately 28.8 million. Approximately 2 000
patients are transplanted yearly within
Scandiatransplant (see also the transplantation and
waiting list
figures).
The South Alliance for Transplants (SAT) is trans-
national alliance of south-west European countries
aimed at strengthening and implementing
cooperation in the field of organ, tissue and cell
donation. It has five partner countries: France, Italy,
Portugal, Spain, Switzerland and Czechia (observer),
and covers a population of almost 202 million. SAT
accounts for more than half of all organ donors and
nearly half of all transplanted patients in the EU.

Organ donation and transplantation
9
portal are France, Spain and Italy, while the countries transplanting most organs are Italy, Czechia
and France. On average, 15 organs are offered and two transplanted every month.
The EU has provided funding for several other projects in the area of organ donation and
transplantation, both through the third EU health programme
(2014-2020) and its predecessors, and
through Horizon 2020 and previous EU research framework programmes. On the initiative of the
European Parliament, the EU also funded two pilot projects that ended in 2019: EDITH – focusing on
treatment modalities for end-stage kidney disease, along with different organ donation and
transplantation practices, and
EUDONORGAN – a service contract involving training and social
awareness for increasing organ donation in the EU and neighbouring countries. Other recent
examples include
ELAPHARMA, a novel approach to organ preservation before transplantation, and
NORMOPERF, the development of a portable device for the ex vivo preservation and viability
assessment of solid organs (kidney and liver) for transplantation based on a patented technology.
International and European organisations
World Health Organization
In the area of transplantation, the World Health Organization (WHO) works with member states to:
1 provide assistance to ensure effective national oversight of allogeneic and
xenogeneic transplantation activities. This would ensure accountability, traceability,
and appropriate surveillance of adverse events;
2 increase citizens' access to safe
and effective transplantation of
cells, tissues and organs, and
ensure ethical and technical
practices;
3 promote international
cooperation to encourage global
harmonisation of technical and
ethical practices in
transplantation; this would include
preventing the exploitation of the
disadvantaged through transplant
tourism and the sale of human
material for transplantation;
4 encourage donation of human
material for transplantation.
The WHO
explains that transplantation of
human cells, tissues or organs saves lives
and restores essential functions where no
alternatives of comparable effectiveness
exist. The WHO also notes the major
differences between countries in access to
suitable transplantation, and in the level of
safety, quality and efficacy of donation and
transplantation. It emphasises the ethical
aspects of transplantation, cautioning that
transplant shortages and patients' unmet
transplant needs tempt some into
trafficking human body components for
transplantation (see box).
Declaration of Istanbul
The 2008 Declaration of Istanbul on organ trafficking
and transplant tourism was drafted u
nder the
leadership of the Transplantation Society and the
International Society of Nephrology at the end of a
global summit, initiated by the World Health
Organization. It sets out definitions for unethical
practices, such as transplant tourism and organ
trafficking, and lays down
principles to guide
policymakers and health professionals working in the
field. The declaration was
updated in 2018, and now
includes a more succinctly worded set of principles. For
instance:
[…]
3. Trafficking in human organs and trafficking in
persons for the purpose of organ removal
should be prohibited and criminalised.
4. Organ donation should be a financially
neutral act. […]
7.
All residents of a country should have
equitable access to donation and transplant
services and to organs procured from
deceased donors. […]
11. Countries should strive to achieve self-
sufficiency in organ donation and
transplantation.

EPRS | European Parliamentary Research Service
10
The WHO Guiding Principles on Human Cell, Tissue and Organ Transplantation, first endorsed in
1991 and updated in 2010, urge member states, among other things, to:
promote the development of systems for the altruistic, voluntary, non-remunerated
donation of cells, tissues and organs as such from deceased and living donors, and
increase public awareness and understanding of the resulting benefits ;
oppose the seeking of financial gain or comparable advantage in transactions involving
human body parts, organ trafficking and transplant tourism;
promote a system of transparent, equitable allocation of organs, cells and tissues,
guided by clinical criteria and ethical norms, as well as equitable access to
transplantation services in accordance with national capacities;
strengthen national and multinational authorities to provide oversight, organisation
and coordination of donation and transplantation activities, with special attention to
maximising donation from deceased donors and to protecting the health and welfare
of living donors with appropriate healthcare services and long-term follow up.
The WHO operates the Global Knowledge Base on Transplantation
(GKT), a source of information on
organ, tissue and cell donation and transplantation for those involved in the field – from the lay
public, to health professionals and health authorities. The GKT is made up of four components that
are being progressively developed: activity and practices; legal framework and organisational
structure; vigilance, threats and responses; and xenotransplantation. The Spanish national
transplantation agency (Organización National de Trasplantes,
ONT) collaborates with the WHO on
GKT by maintaining a global database with information on organ donation and transplantation
activities derived from official sources, and on legal and organisational aspects. The database can
be accessed via the
Global Observatory on Donation and Transplantation (GODT) website.
Council of Europe
In addition to being an international human rights organisation, the Council of Europe is also a
leading standard-setting institution in the field of organ, tissue and cell transplantation. It has
adopted legally binding texts on the topic, such as the 1997
Oviedo Convention on Human Rights
and Biomedicine and the 2002 Additional Protocol on transplantation of organs and tissues of
human origin to the Oviedo Convention, as well as the 2015 Convention against Trafficking in
Human Organs. Its non-legally binding texts include recommendations– such as those on
xenotransplantation, organ donor registries, organ trafficking, and criteria for the authorisation of
organ transplantation facilities – and resolutions, for instance, on removal, grafting and
transplantation of human substances, and on establishing harmonised national living donor
registries with a view to facilitating international data sharing. Moreover, it issues reports and other
publications on the topic, such as Ethical eye: transplants.
The Council of Europe's work on organ transplantation is coordinated by the European Directorate
for the Quality of Medicines and Healthcare (EDQM
), whose mission is: to ensure human dignity;
maintain and fulfil human rights and fundamental freedoms; guarantee non-commercialisation of
substances of human origin; and protect
donors and recipients of organs, tissues and
cells. Within the EDQM, the European
Committee on Organ Transplantation,
composed of internationally recognised
experts, is in charge of: organ
transplantation activities that promote the
non-commercial donation of organs, tissue
and cells; the fight against organ trafficking;
and the development of ethical, quality and
safety standards in the field of organs,
tissues and cells. It provides
technical guides
European Day for Organ Donation and
Transplantation on 10 October
The Council of Europe's EDQM organises the European
Day for Organ Donation and Transplantation (EODD)
every year to raise awareness of organ, tissue and cell
donation as a way to improve and save lives. The EODD
seeks to encourage public debate on the topic, and
invite health professionals and policy-makers across
Europe to reflect on the importance of this therapy.
The EODD event takes place in a different country
every year. In 2020, the host country is Poland.

Organ donation and transplantation
11
for professionals, including on the quality and safety of both organs for transplantation and tissues
and cells for human application.
4
The Newsletter Transplant, published yearly, contains figures for
organ donation and transplantation across Europe and internationally. The EDQM also issues
booklets for a wider audience, such as on
donation of oocytes (egg cells) or post-transplant health.
The EDQM's 2003 European consensus document 'Organ shortage: current status and strategies for
improvement of organ donation' provides a step-by-step guide to the procurement of high-quality
organs from cadaveric donors, based on scientific data and international experience. The specific
recommendations underline, among other things, the need for an appropriate legal framework for
donation and transplantation that adequately defines brain death, the type of consent or
authorisation required for organ retrieval, and the means of retrieval, ensuring traceability while
maintaining confidentiality and banning organ trafficking.
Stakeholders' views
In October 2019, a number of stakeholders from the organ donation and transplantation community
submitted a joint statement
(updated version – January 2020) on a shared vision for improving
organ donation and transplantation to the European Commission. The statement was the main
output of the 2019 thematic network on improving organ donation and transplantation, led by the
European Kidney Health Alliance (
EKHA). It was developed in conjunction with national competent
authorities for organ donation and transplantation, transplant organisations, medical professionals
and patient associations, and
endorsed by co-signing organisations and Members of the European
Parliament. The policy recommendations made include: i) mobilising political will to make organ
donation and transplantation a priority; ii) improving legal and institutional frameworks; iii)
streamlining organisation and investment in leadership at all levels; iv) allocating appropriate funds
for organ donation and transplantation programmes; v) promoting education and training among
all stakeholders; vi) eradicating inequities in organ donation and transplantation; vii) boosting
benchmarking; and viii) leveraging research.
Looking ahead
As noted in the Commission's 2017 study on the uptake and impact of the EU action plan, many
countries have agreed that future European cooperation is important to promote organ
transplantation, and that EU activities should be continued. The study identified the need for a new,
improved action plan to cover areas such as: communication; education of professionals;
exchange of experiences on minorities and new population groups; end-of-life care; and research.
Innovative products, such
organoids – artificially grown organs that mimic the properties of real
organs – could become a complement to current organ transplantation to restore liver function in
patients with metabolic liver disease. In the near future, organoids may even be transplanted into
people to replace diseased or failing natural organs. According to the European Parliament's Science
and Technology Options Assessment (STOA), producing reliable biological materials on demand
through 3D bio-printing is
an interesting future possibility that might reduce our reliance on organ
donors. In a possible future in which organs are 3D printed, several ethical issues surrounding organ
donation would be resolved: there would be no more dilemmas regarding organ allocation or
scandals due to non-transparent organ distribution by hospitals. The contested field of
xenotransplantation would become obsolete. The psychological problems of patients receiving, for
instance, a heart from a deceased person would no longer be an issue. Human organ smuggling
would become less economically rewarding. In more realistic terms, however, there may be waiting
lists for printed organs, due to limited production capacity and high costs. Moreover, one negative
outcome of the feasibility of organ printing may be that motivation to donate organs would
probably decline and lead to an overall worse situation in terms of
health inequalities for people in
need of an organ (with only those able to afford to pay for their own organs benefiting). Finally, as
the study notes, before bio-printing solid organs becomes routine medical practice, the issue of
whether 3D-printed organs will (or should) be patentable, and what this would mean for patients'
autonomy, needs to be addressed.
EPRS | European Parliamentary Research Service
12
MAIN REFERENCES
Boucher P., 3D bio-printing for medical and enhancement purposes, Scientific Foresight Unit (STOA),
European Parliament, 2018.
Guide to the quality and safety of organs for transplantation, 7th edition, European Directorate for the
Quality of Medicines and Healthcare (EDQM), Council of Europe, 2018.
Guide to the quality and safety of tissues and cells for human application, 4th edition, EDQM, Council of
Europe, 2019.
Newsletter Transplant 2019, Volume 24 (2018 data), EDQM, Council of Europe, 2019.
Organ shortage: current status and strategies for improvement of organ donation – A European
consensus document, EDQM, Council of Europe, 2003.
Study on the uptake and impact of the EU action plan on organ donation and transplantation (2009-
2015) in the EU Member States, European Commission, 2017.
ENDNOTES
1
'Actual deceased organ donors' are donors from whom at least one organ has been recovered for the purpose of
transplantation (in contrast to 'utilised donors', who are donors from whom at least one organ has been transplanted).
2
From 2008 to 2010, 20 organs from Malta were transplanted in Italy.
3
In 2009, 41 organs were offered to Spain from Portugal.
4
For the downloadable versions of both publications, see the 'Main references' section.
DISCLAIMER AND COPYRIGHT
This document is prepared for, and addressed to, the Members and staff of the European Parliament as
background material to assist them in their parliamentary work. The content of the document is the sole
responsibility of its author(s) and any opinions expressed herein should not be taken to represent an official
position of the Parliament.
Reproduction and translation for non
-commercial purposes are a
uthorised, provided the source is
acknowledged and the European Parliament is given prior notice and sent a copy.
© European Union, 2020
.
Photo credits: ©
Csaba Deli / Shutterstock.com.
[email protected]ropa.eu (contact)
www.eprs.ep.parl.union.eu
(intranet)
www.europarl.europa.eu/thinktank
(internet)
http://epthinktank.eu
(blog)
