
i
OCCUPATIONAL THERAPY PRACTICE USED FOR CHILDREN DIAGNOSED WITH
A DUAL DIAGNOSIS OF CEREBRAL PALSY AND VISUAL IMPAIRMENT IN SOUTH
AFRICA
Zonè Janse van Rensburg
A research report submitted to the Faculty of Health Sciences, University of the
Witwatersrand, Johannesburg, in partial fulfilment of the requirements for the degree
of
Master of Science in Occupational Therapy
Johannesburg, 2016
brought to you by COREView metadata, citation and similar papers at core.ac.uk
provided by Wits Institutional Repository on DSPACE

ii
DECLARATION
I, Zonè Janse van Rensburg, declare that this research report is my own work. It is being
resubmitted for the degree of Master of Science in Occupational Therapy at the University of the
Witwatersrand, Johannesburg. It has been submitted before for examination at this university
and has been revised as per the examinees requests and specifications.
15 of March, 2016
iii
ABSTRACT
Occupational therapy aims to assist children diagnosed with cerebral palsy (CP) to achieve
independence in their occupational performance areas. Treatment includes the use of sensory
stimulation but when a child’s vision is impaired the use of visual stimulation becomes difficult.
Research guiding occupational therapists on how to combine treatment methods successfully
when treating children with CP with a co-morbid diagnosis of visual impairment is limited
(15)(16)
.
This study aims to determine the occupational therapy practice used, including the therapists’
knowledge; skill and perceived confidence, for children with a dual diagnosis of CP and visual
impairment in South Africa.
It uses a descriptive, non-experimental, cross-sectional framework within a quantitative research
approach. Purposive sampling was used to select participants.
This study finds uniformity in the approaches occupational therapists use when managing these
children, but these approaches are not always based on best practice. Therapists use clinical
expertise and integrate evidence based practice rather than the other way around. This study
demonstrates a need for clear protocols on how to manage these children and more accessible
postgraduate training in the management of them.
iv
TABLE OF CONTENTS
DECLARATION .......................................................................................................................... ii
ABSTRACT ................................................................................................................................ iii
TABLE OF CONTENTS ............................................................................................................. iv
ABBREVIATIONS .................................................................................................................... viii
LIST OF OPERATIONAL DEFINITIONS .................................................................................... ix
LIST OF FIGURES ..................................................................................................................... x
LIST OF TABLES ....................................................................................................................... xi
1.0 Chapter 1: Introduction............................................................................................................1
1.1 Introduction ........................................................................................................................... 1
1.2 Problem statement ................................................................................................................ 3
1.3 Research question ................................................................................................................ 3
1.4 Aim of the study .................................................................................................................... 3
1.5 Objectives of the study .......................................................................................................... 3
1.6 Justification of the study ........................................................................................................ 4
1.7 Organisation of the report ...................................................................................................... 4
2.0 Chapter 2: Literature review....................................................................................................6
2.1 Cerebral palsy and impairments ............................................................................................ 6
2.2 Cerebral palsy and visual impairment .................................................................................... 7
2.3 Occupational therapy intervention ......................................................................................... 8
2.4 Occupational therapy intervention for children with visual impairments ................................. 9
2.5 Theories, frames of reference and modalities used by occupational therapists for children
diagnosed with cerebral palsy and visual impairment ................................................................ 12
2.5.1 Somatosensory development and approach ................................................................. 14
Rood techniques ................................................................................................................... 16
2.5.2 Sensory integration ....................................................................................................... 17
2.5.3 Neurophysiological approach (proprioceptive neuromuscular facilitation) ..................... 19
Constraint induced therapy .................................................................................................... 20
2.5.5 Dynamic systems theory ............................................................................................... 20
2.5.6 Neurodevelopmental therapy approach ........................................................................ 21
2.5.8 Family-centred approach .............................................................................................. 23
2.5.9 Multi-disciplinary team approach................................................................................... 24
v
2.5.10 Compensatory approach............................................................................................. 25
2.5.11 Other approaches: Cognitive approach and motor learning ........................................ 26
2.6 Evidence based practice ..................................................................................................... 27
2.7 Conclusion .......................................................................................................................... 29
3.0 Chapter 3: Research Methodology........................................................................................30
3.1 Study design ....................................................................................................................... 30
3.2 Population ........................................................................................................................... 30
3.3 Sampling ............................................................................................................................. 31
3.4 Development of the measurement tool ................................................................................ 31
3.4.1 Pilot testing ................................................................................................................... 32
3.5 Data collection .................................................................................................................... 34
3.6 Data management ............................................................................................................... 34
3.7 Ethical considerations ......................................................................................................... 35
4.0 Chapter 4: Results.................................................................................................................36
4.1 Demographics of the participants ........................................................................................ 36
4.1.1. Gender ........................................................................................................................ 36
4.1.2 Educational background of the participants .................................................................. 37
4.1.3 Participants’ report on further training in the rehabilitation of children diagnosed with
cerebral palsy ........................................................................................................................ 38
4.1.4 Participants’ work information ....................................................................................... 39
4.1.5 Participants’ reasons for attending post graduate training in the form of courses,
diplomas or degrees. ............................................................................................................. 41
4.1.6 Participants’ cerebral palsy caseload ............................................................................ 44
4.2 Participants’ treatment regimes for children with cerebral palsy and visual impairment ....... 45
4.3 Participants and different therapeutic interventions ............................................................. 47
4.3.1 Treatment interventions used by participants ................................................................ 47
4.3.2 Participants’ reasons for using the various approaches and treatments ........................ 49
4.3.3 Participant’s use of approaches and treatments in combination .................................... 51
4.4 Participants’ responses on their confidence and attitude towards their knowledge and
training ...................................................................................................................................... 52
4.4.1 Participants’ undergraduate training ............................................................................. 52
4.5 Participants' confidence in their knowledge of and skill in the approaches and treatments
used for children diagnosed with CP and visual impairment, and their view of the effectiveness
of these treatments ................................................................................................................... 53
vi
4.6 Information gathered in an open-ended format regarding participants’ treatment, training and
opinions .................................................................................................................................... 58
4.6.1 Summary of the most frequently reported outcomes regarding what the participants saw
as their three most functional short-term outcomes ............................................................... 59
4.6.2 Summary of the most frequently reported outcomes regarding what the participants saw
as their three most functional long-term outcomes:................................................................ 60
4.6.3 Participants’ report on the most important principles used when treating these children61
4.6.4 Summary of the participants’ report on their perceived success in reaching their
outcomes and the reasons for success or failure: .................................................................. 63
4.6.5 Summary of the participants’ report on how they change their treatment interventions
when children have a dual diagnosis of CP and visual impairment ........................................ 64
4.6.6 Summary of the participants’ report on the sufficiency of training in South Africa .......... 65
4.6.7 Summary of participants’ report whether their treatment should be scientifically proven
and evidence-based and their understanding of these terms ................................................ 67
4.7 Conclusion and summary of the main results ...................................................................... 67
5.0 Chapter 5: Discussion...........................................................................................................71
5.1 Introduction ......................................................................................................................... 71
5.2 Response rate to the survey ............................................................................................... 71
5.3 Demographic characteristics of the participants .................................................................. 72
5.4 Treatment interventions....................................................................................................... 75
5.4.1 Occupational therapists’ approach to their treatment regimes ....................................... 75
5.4.2 Occupational interventions used by therapists to guide their treatment for children
diagnosed with CP and visual impairment ............................................................................. 76
5.4.3 Reasons participants reported for using certain approaches when managing children
with CP and visual impairment .............................................................................................. 78
5.4.4 Therapists’ perceived confidence in their knowledge, skill and effectiveness in the
treatment of children with a dual diagnosis of CP and visual impairment ............................... 79
5.5 Participants’ undergraduate and postgraduate training ....................................................... 80
5.6 Interventions for children with a dual diagnosis of CP and visual impairment ...................... 81
5.6.1 Most commonly reported outcomes .............................................................................. 81
5.6.2 Changes to treatment interventions to accommodate children with a dual diagnosis of
CP and visual impairment ...................................................................................................... 83
5.6.3 Participants’ principles when treating children with a dual diagnosis of CP and visual
impairment ............................................................................................................................ 84
vii
5.6.4 Participants’ perceived success in the treatment of children with a dual diagnosis of CP
and visual impairment ............................................................................................................ 85
5.6.5 Participants’ perceived confidence in their treatment .................................................... 86
5.7 Participants’ perception of the training available in South Africa in the treatment of children
with a dual diagnosis of CP and visual impairment, and how they view evidence-based practice87
5.8 Implications for current practice ........................................................................................... 87
5.9 Conclusion .......................................................................................................................... 88
6.0 Chapter 6: Conclusion...........................................................................................................90
6.1 Suggested further research ................................................................................................. 92
6.2 Limitations to this study ....................................................................................................... 92
REFERENCES ......................................................................................................................... 93
Appendix A ............................................................................................................................. 100
Information letter ..................................................................................................................... 100
Appendix B ............................................................................................................................. 102
QUESTIONNAIRE .................................................................................................................. 102
SECTION A.1:......................................................................................................................... 102
Demographic information ........................................................................................................ 102
SECTION B.1:......................................................................................................................... 103
This section will gather information related to post graduate training in the form of courses,
diplomas or degrees................................................................................................................ 103
SECTION B.2:......................................................................................................................... 105
Treatment intervention including modalities and frames of references .................................... 105
SECTION C: ........................................................................................................................... 106
Personal knowledge, confidence and skill in treatment intervention ........................................ 106
Appendix C ............................................................................................................................. 111
Ethics Clearance Certificate .................................................................................................... 111
viii
ABBREVIATIONS
CP – Cerebral palsy
CVI – Cerebral Visual Impairment
ICF – International Classification of Functioning: Disability and Health
OTPF II – Occupational Therapy Practice Framework II
OTASA – Occupational Therapy Association of South Africa
SANDTA – South African Neurodevelopmental Therapy Association
AAC – Alternative and Augmentative Communication
NDT – Neurodevelopmental therapy
SOPT - Systematic Occupational Therapy Practice
ix
LIST OF OPERATIONAL DEFINITIONS
Cerebral palsy: Cerebral palsy (CP) is considered as a group of disorders affecting motor
development including posture and movement although the severity and type of symptoms vary
according to the lesion in the brain
(1)
. The lesion is a non-progressive insult to the developing
foetus or infant brain which is considered from birth usually up to the age of five
(1)
.
Cerebral vascular impairment (CVI): This is a visual impairment as a result of damage to the
retrogeniculate visual pathways
(10)
.
Frame of reference: A frame of reference provides the platform for therapists to organise their
knowledge enabling the planning of intervention. This helps to link the theory to applying
treatment. It consists of several components including a theoretical base, evaluation, a
function/dysfunction continuum and suggests change
(30)
.
Treatment approach: A treatment approach is the outline of a plan developed by the therapist
in collaboration with the client which will guide the treatment. It is based on the relevant
theories, frames of reference and available evidence and is either aimed to promote, restore,
modify or maintain health or prevent further regression
(9)
.
Treatment modality: The specific methods used by a therapist to address the particular
condition of a client
(2)
.
x
LIST OF FIGURES
4.1.5 (a) Reason for attending postgraduate training was to improve knowledge and skill .......41
4.1.5 (b) Reason for attending postgraduate training was to improve the management of
children with a dual diagnosis of CP and visual impairment ..............................................42
4.1.5 (c) Reason for attending postgraduate training was because of its affordability ...............42
4.1.5 (d) Reason for attending postgraduate training was because of its regularity ..................43
4.1.5 (e) Reason for attending postgraduate training was because it was scientifically proven
and evidence-based to improve outcomes in therapy ........................................................43
4.1.5 (f) A summary of the reasons for attending postgraduate training ....................................44
4.2 (a) Participants’ response to recognising visual impairments in children with CP ................46
4.2 (b) Participants’ response to using a multi-disciplinary team when treating children with CP
and visual impairments ......................................................................................................46
4.2 (c) Participants changed their treatment management when a child with CP has a visual
impairment .........................................................................................................................47
4.3.1 (a) Therapeutic interventions when managing children with CP and visual impairment ....48
4.3.1 (b) Therapeutic approaches from most popular to least popular .......................................49
4.3.2 Participants’ reasons for using various approaches and treatments .................................50
4.3.3 Reasons displayed as an average of participants’ use therapeutic approaches or
treatment interventions .......................................................................................................51
4.3.3 Participants’ response to whether different approaches or treatment interventions are best
used in combination ...........................................................................................................51
4.4.1 (a) Participants’ perceptions whether their undergraduate training was adequate for
managing children with CP ................................................................................................52
4.4.1 (b) Participants’ perception whether their undergraduate training was adequate to manage
children with a dual diagnosis of CP and visual impairment effectively ...............................53
4.5.1 Participants’ confidence in their knowledge ......................................................................54
4.5.2 Participants’ confidence of their skill .................................................................................55
4.5.3 (a) Comparison between four therapeutic approaches and the participants’ knowledge and
skill.....................................................................................................................................56
4.5.3 (b) Comparison between the remaining four therapeutic approaches and the participants’
knowledge and skill ............................................................................................................57
4.5.4 (a) Participants’ perceived effectiveness of their treatment to manage these children .....58
4.5.4 (b) Participants’ confidence in their treatment to manage these children .........................58
xi
4.6.1 Summary of the participants’ most functional short-term outcomes ..................................60
4.6.2 Participants’ report on the most functional long-term outcomes ........................................61
4.6.3 Most common principles used during treatment ...............................................................62
4.6.4 Participants’ perceived success in reaching their outcomes .............................................64
4.6.5 Participants’ change in treatment interventions to accommodate children with a dual
diagnosis of CP and visual impairment ..............................................................................65
4.6.6 Report on the sufficiency of training in South Africa .........................................................66
xii
LIST OF TABLES
Table
4.1.1 Gender distribution of the participants................................................................................37
4.1.2 Undergraduate training and year qualified.........................................................................37
4.1.3 Participants’ further training in the rehabilitation of children diagnosed with CP ...............39
4.1.4 Participants’ years of experience with CP, current field and area of work .........................40
4.1.6 Incidence of visual impairment in participants’ CP caseload and the different types ........46

1
Chapter 1: Introduction
1.1 Introduction
Cerebral palsy (CP) is considered as a group of disorders affecting motor development including
posture and movement although the severity and type of symptoms vary according to the lesion in
the brain
(1)
. The lesion is a non-progressive insult to the developing foetus or infant brain which is
usually considered from birth up to the age of five
(1)
.
Though the exact prevalence of CP in South Africa is not known, the World Health Organization
reported that 10% of children with disabilities in South Africa present that of neurogenic origin
(2)
. A
population study conducted in the United States reported that the incidence of CP ranges from 1.5
to 4 children out of 1000
(3)
. The study also reported that the incidence of CP in developed countries
or areas with sophisticated health care would be lower than in rural settings or developing
countries where health care is not as accessible
(3)
. Poor health care increases the risk of children
being born with CP because of delays in birth, higher risk of infection and premature births
(4)(5)
.
South Africa is considered a developing country with regards to health care, so for the purpose of
this study it may be assumed that the incidence for CP is higher than 1.5 to 4 children out of
1000
(3)(5)
. A study by Van Toorn; Laughton & Van Zyl (2007) conducted in the Western Cape
investigated the aetiology of CP and found that the prevalence for this condition is similar for
developing and developed countries
(6)
. They suggested the difference in the incidence between
these countries lies in the aetiology of CP. Their research suggested that the majority of CP in
developing countries occurs before birth, but for acquired CP the occurrence varies from 5% in the
most developed country to 60% in the least developed country
(6)
. The reason for the higher
occurrence of acquired CP is consistent with the US study that reported the high incidence of CP
in developing countries is largely owing to poor health care and other risk factors
(6)
.
CP always results in motor disturbances but depending on the site and size of the lesion in the
brain it is often accompanied with disturbances by sensation; cognition; behaviour and
perception
(1)(7)
. This affects all areas of a child’s ability to perform his/her daily activities. Not only
will their impaired motor function inhibit them from having functional and/or safe mobility but the
motor disturbances in addition to other disturbances affect vision; swallowing; playing and social
interaction; as well as cognitive functions such as memory; concentration and abstract reasoning
and the list can be endless
(8)
. All of these skills are essential for activities of daily life
(9)
.
2
Recent research that investigated neuro-ophthalmological disorders associated with CP in Italy
estimated that about 60% of children diagnosed with CP have visual impairments
(10)
. A reason
suggested for the high prevalence of neuro-ophthalmological disorders is extensive brain injury
that resulted in multi-system involvement, which implies many of the structures of the brain are
affected
(11)
. These visual impairments can be categorised either as peripheral problems or cerebral
visual impairments (CVI) and commonly present as strabismus, poor visual acuity; decreased
visual field, astigmatism, stereopsis and nystagmus
(4)(10)(12)
. Functionally the child’s visual
impairments will present as difficulty fixating on and following objects, poor visual processing and
understanding objects, poor figure ground and depth perception, spatial relational issues and
decreased visual field
(12)(13)
.
Visual impairments may present itself differently in each type of CP. For example it is more
common for a child diagnosed with spastic CP to present ocular abnormalities because of
extensive and diffuse lesions in the brain, as opposed to athetoid or ataxic children
(11)
. Dyskinetic
strabismus is commonly associated with the athetoid CP which might be a result of involvement of
the basal ganglia
(11)
.
Children with CP often experience a poorer quality of life because they are unable to participate in
age-appropriate occupational performance areas because of the many debilitating symptoms they
experience
(1)
. The ultimate aim of occupational therapy intervention should be to improve their
quality of life
(1).
Occupational therapy for children diagnosed with CP aims to facilitate normal
development by addressing the client factors and performance skills that limit their ability to
engage in independent and milestone-appropriate occupational performance
(9)(1)
.
Treatment includes addressing problems related to range of movement and posture, facilitating
movement, providing the child with CP with assistive devices to compensate for lack of mobility
and/or maintaining good posture and encouraging independence in performing activities of daily
living
(14)(15)
. For a child with CP and visual impairment the ultimate aim would be similar in
accordance with the ultimate aim of occupational therapy however the child would be more
severely affected and the treatment would therefore need to be adjusted to suit the child.
Considering the additional visual problems associated with CP, therapy would either aim to
improve or compensate for the visual impairment as well as take into account the other goals
already mentioned. Addressing the visual impairments could include addressing the visual
perceptual deficits or compensating for them
(4)(14)
. This would improve the child’s ability to engage
3
as independently as possible in age-appropriate occupational performance areas which would
ultimately improve their quality of life
(1)
.
1.2 Problem statement
Occupational therapy aims to assist children diagnosed with CP to achieve independence in
activities of daily living so as to achieve age-appropriate developmental milestones. This includes
but is not limited to self-care and grooming, mobility, education, play, motor skills and perceptual
skills. Occupational therapists treating children diagnosed with CP usually use tactile and visual
cues to elicit movement and encourage the child to explore. However, the use of visual cues is
difficult or even impossible to use when vision is impaired. This means that other modalities should
be added to treat children with CP and visual impairment.
Research guiding therapists on successfully combining treatment methods and techniques in
occupational therapy interventions for children with a dual diagnosis of CP and visual impairment is
limited and lacks in scientific proof
(15)(16)
which makes it especially difficult for newly qualified
therapists to plan effective interventions.
1.3 Research question
What is the current occupational therapy intervention for children diagnosed with a dual diagnosis
of CP and visual impairment in South Africa and what is the perceived confidence of occupational
therapists in their ability to treat these children?
1.4 Aim of the study
This study aims to determine the current occupational therapy practice used for children diagnosed
with CP and who are visual impaired in South Africa, and how confident occupational therapists
are in treating these children.
1.5 Objectives of the study
This study intends to:
1. determine the occupational therapy interventions used by therapists in South Africa to
guide their treatment, including the frames of reference and treatment modalities used for
children with a dual diagnosis of CP and visual impairment; and
2. determine occupational therapists perception of confidence in their knowledge, training and
skill to treat children with a dual diagnosis of CP and visual impairment.
4
1.6 Justification of the study
The lack of literature to guide therapists in planning and implementing interventions for children
with a dual diagnosis of CP and visual impairment indicates a need to investigate and report on
occupational therapy practice in this area. This study will provide information on occupational
therapy practice in South Africa for children diagnosed with CP and visual impairment, and
occupational therapists’ perceived confidence, knowledge and skill in their treatment, as well as if
they perceive this treatment to be effective. This is important as they can provide information on
the effectiveness of treatment from a clinical perspective. Occupational therapists can also provide
information on their knowledge of what options are available for optimal treatment which will help
to ensure occupational therapy in South Africa remains evidence based. This study could then
provide information that could be used to develop a guideline for occupational therapy
interventions for children with a dual diagnosis of CP and visual impairment.
1.7 Organisation of the report
This report comprises six chapters.
Chapter 1 provides background information on how a combination of CP and visual impairment
affects children and highlights the problem this creates for occupational therapists. It reflects on the
limited information available for occupational therapists to know how to plan and execute
interventions for children with a dual diagnosis of CP and visual impairment
Chapter 2 reviews literature on the complications present in children with CP and visual
impairment as well as occupational therapy interventions for these children. It also investigates the
treatment methodologies available for occupational therapy interventions for children with CP and
visual impairment.
Chapter 3 reports on the methodology followed in this report: a descriptive, non-experimental,
cross-sectional research design within a quantitative research approach. It discusses population
and sampling methods, and how the researcher designed a measurement tool used in the study. It
also reviews the collection of data.
Chapter 4 reports on the results obtained from the questionnaire that was developed for this study.
Chapter 5 reflects on how the results correlate with available research and literature. It discusses
the significance of the results in light of which interventions are recommended in the literature.
5
Chapter 6 provides a conclusion on the best occupational therapy practice for children with a dual
diagnosis of CP and visual impairment. It also provides recommendations for further studies that
may arise from this report, and considers limitations within the study.

6
Chapter 2: Literature review
2.1 Cerebral palsy and impairments
Children diagnosed with cerebral palsy (CP) can have a great number of co-morbid deficits, as
explained in the introduction and can thus be referred to as multi-disabled children
(11)
. These multi-
disabled children always have motor disturbances, with the main motor deficit related to muscle
tone changes which, in turn, could lead to other motor impairments such as decreased motor
control and motor planning, and impaired balance and coordination among others
(17)
. Co-
morbidities can include cognitive impairment, visual impairment, communication difficulties,
swallowing and feeding difficulties, sensory integration challenges, low endurance levels and
emotional/behavioural difficulties
(17).
These deficits contribute to the child experiencing difficulty
performing activities of daily living
(18)
. This affects all areas of occupational performance such as
personal management, survival skills, education or work, rest or sleep, play, and participation in
social and community events and activities
(9)
.
Children diagnosed with CP often experience a lower quality of life because they struggle to
participate in daily activities
(1)
. This is confirmed in a study by Tsoi, Zhang, Wang, Tsang & Lo
(2011) who investigated quality of life for children with CP. The authors reported that children with
CP, regardless of the severity of the lesion, commonly report or their families report that their
children with CP experience a lower quality of life
(1)
. The World Health Organisation sees quality of
life as a person’s own evaluation or opinion of their satisfaction across all domains in life. This
encompasses the person’s context of their culture and value systems in relation to their goals and
concerns for their life
(1).
Quality of life can then be divided into five domains including
physical/health, psychological, education and/or work, cognition and participation in society
(1)
. It is
important to note that quality of life does not only involve independence or physical health, it takes
into consideration the individual’s context and culture as well. Therefore interventions made by
occupational therapists should not only support the physical aspects of the person, they should be
culturally competent in order to treat the person holistically
(1)
. Occupational therapists should also
ensure that they take the person or the person’s family’s goals into consideration to ensure that
improvement of quality of life is satisfactory across all domains of life
(1)
. If children with CP
commonly experience a lower quality of life it can then be assumed that a child with a dual
7
diagnosis of CP and visual impairment would experience an even lower quality of life as these
children are often more severely affected
(11)(17)
.
2.2 Cerebral palsy and visual impairment
As previously mentioned 1.5 to 4 out of 1000 births result in CP and of those births around 60%
are visually impaired
(3)(10)
. No research has been done in South Africa to determine the exact
prevalence of children diagnosed with CP and visual impairment. The motor control deficits in
children with CP as discussed under 2.1 p. 6 can affect the functioning of almost the entire body as
it influences mobility and posture, dexterity, eye movement, speech and swallowing, gesturing and
facial expressions and the digestive system
(10)(7)(8)
. If deficiencies in motor control affect all of these
areas it is clear that these impairments make tasks such as personal grooming and self-care, care
of others, accessing education or work, playing and participating in community or social events
difficult
(17)
. These are all occupational performance areas in which a child would need to participate
to achieve independence at age appropriate milestones
(15)
.
Visual impairments found in children with CP can be categorised either as peripheral problems or
cerebral visual impairments (CVI)
(11)
. After investigating various ocular abnormalities in Kenya
Njambe, Kariuki & Masinde (2009) reported that even though it is common for children with
developmental disabilities to have visual abnormalities this is often overlooked or ignored
(11)
. This
oversight has had devastating consequences for the development of children with CP who are
visually impaired
(4)(10)(11)
as visual impairment affect various levels of childhood development in
terms of fixating on objects, following objects, developing visual perceptual skills among
others
(12)(13)
. The reason for visual impairments being overlooked or under managed during
assessment and treatment is that practitioners find it difficult to accurately assess children who
already have mental and/or physical disabilities
(11)
. Diagnosis also requires specialised tests known
as a Visual Evoked Potential where the brain is scanned to measure visual electrical signals
(19)
.
These tests are not always available in the South African public health system as equipment to
conduct them is expensive to acquire and run and often staff members are not trained to
administer them
(2)
.
The study by Njambe et al. (2009) further reported that rehabilitation therapists often feel that
interventions for visual impairment would not impact significantly on the child’s condition or change
the prognosis
(11)
. This is cause for concern as children with CVI struggle to focus on or recognise
objects, and experience visual field loss which impacts on their ability to learn as vision is an
important aspect to achieving visual perceptual skills and other learning tasks
(12)(13)
. Impaired vision
8
also negatively impacts the child’s ability to achieve independence in age appropriate
milestones
(12)(13)
. Another cause for concern is these children struggle to recognise familiar faces
and everyday objects which negatively impacts their participation in social relationships, the
execution of daily activities to the limitations of their physical abilities, and participation in education
– all aspects that will directly influence their quality of life
(10)(20)
.
2.3 Occupational therapy intervention
The treatment of children with CP, should aim to improve, manage or compensate for all
impairments or problems associated with the dysfunction found
(8)
. This includes visual impairments
found in many children with CP
(10)
such as the visual perceptual deficits and reduced visual field
that inhibit the child from taking part in activities of daily living
(12)(13)(21)
.
The duration of therapy requires intensity and repetition to have a meaningful impact on the
prognosis of a client and clients have a better prognosis if they are from enriched environments as
opposed to poor/deprived environments
(22)
. In South Africa these factors such as the intensity and
repetition of therapy as well as the clients’ backgrounds have major implications for rehabilitation
as many of our clients live in poverty, live far from rehabilitation units, have families with little or no
education and limited family support thus implementing assistive devices and home programs that
can promote quality of life and improve independence is often a challenge
(2)(23)
.
Therapeutic decisions are significantly influenced by factors such as the environment, education
levels, the intensity of training and the ability to repeat training. Decisions such as the different
frames of reference used; expectations placed on the family; type of assistive devices issued;
intensity of therapy and home programs would need to consider the environment and culture the
family will return to, to ensure continuity of therapy.
Tsoi et al. (2011) placed treatment for CP broadly into three categories: physical rehabilitation,
medical intervention and behavioural intervention
(1)
. They categorised physical rehabilitation into
either strength or exercise training and behavioural intervention into an educative approach and
adaptive assistive approach
(1)
. The behavioural approach includes providing assistive devices or
supportive aids to improve functioning
(1)
. Occupational therapists are directly involved in both
physical rehabilitation and behavioural intervention
(24)
.
By combining these two approaches of Tsoi et al. (2011) with the World Health Organisation’s five
domains of quality of life
(1)
physical rehabilitation will address the physical/health domain
(1)(16)
and
the educative approach as part of behavioural intervention will address the education and cognitive
9
domain as well as the physical domain of quality of life
(1)
. The educative approach would also
serve to educate the families of those diagnosed with CP as many times the child is unable to
implement goals of treatment as they are too severely affected
(1)(17)(24)
. Lastly the adaptive assistive
approach deals with the physical/health, educative, social participation and psychological domains
regarding quality of life. This ensures that the child would receive assistive devices; adaptive
techniques or alternative methods to participate in those domains of quality of life in relation to age
appropriate developmental milestones
(1)(15)
.
An additional symptom that needs to be considered during occupational intervention is cognitive
impairments. About 50% of children with CP have learning or intellectual disabilities
(14)
. This
impacts significantly on the manner in which treatment is administered during intervention making
it necessary for occupational therapists to understand the impact of cognitive deficit on children
diagnosed with CP and visual impairment
(3)(14)
. Children with learning or intellectual disabilities
often have difficulty with praxis (understanding instructions, processing information or executing
actions), sequencing, memory and attention
(14)
.
This is important when considering specific
interventions as it impacts on how children learns using assistive devices, how they perceive
intervention in mobility and in general how they would achieve developmental milestones
(3)(14)
thereby determining their overall quality of life.
2.4 Occupational therapy intervention for children with visual impairments
When exploring the various therapeutic approaches for children with a dual diagnosis of CP and
visual impairment the ultimate aim should be to improve quality of life and facilitate participation in
occupational performance areas
(1)(9)
. If quality of life, through the various interventions, is the
ultimate aim for intervention the physical and the behavioural rehabilitation would encompass
managing the child’s condition in its entirety. This includes but is not limited to, addressing the
child’s client factors and performance skills or their body function and structure which would be
limited by their physical disability among other disturbances
(9)(17)
. The ultimate aim then, should be
to improve overall quality of life which would also involve improving independence in all
occupational performance areas
(1)
.
According to the World Health Organisation (WHO) children require vision to reach their
developmental milestones
(25)
. If children have a visual impairment, they would require rehabilitation
to assist them in their development and achieving independence
(25)
. Considering visual impairment
as a single deficit, rehabilitation would include either developing existing visual ability or developing
and using other senses for example hearing, to elicit movement
(10)(12)
. Techniques used to
10
accommodate for visual impairment include simplifying the environment, using bright and colourful
objects to optimise visual focus and using movement, as this makes it simpler for the child with CVI
to locate objects, using contrasting colours, or using a multi-sensory stimuli approach such as
combining touch
(12)
. These methods are reported to facilitate voluntary movement, and could help
the child achieve developmental milestones and/or some independence
(12)
.
When treating a child with a visual impairment, certain techniques as discussed are used to elicit
movement. However many of these techniques cannot be used when children are diagnosed with
CP
(14)(4)
owing to other co-morbidities associated with CP such as epilepsy or sensory
disorganisation and overstimulation
(14)(17)
. This highlights the importance of understanding the
child’s condition and considering the various types of intervention when treating a child with a dual
diagnosis of CP and visual impairment. In addition, the role of the occupational therapist is to
provide assistive devices for mobility and learning
(26)
. These assistive devices are routinely used
for children with visual impairment to achieve relative independence in activities of daily living
(25)
. If
a child has additional mobility impairments, they would struggle to use these assistive
devices
(25)(26)
. Furthermore when supplying assistive devices to facilitate independence, the
question arises as to how the child with a dual diagnosis of CP and visual impairment would use
the device? This is another factor to consider when selecting treatment interventions.
The loss of mobility in children with CP makes it more difficult to compensate for their visual
impairments as one requires vision to be mobile and to reach independence at age appropriate
milestones
(25)(27)
. These children have greater difficulty in achieving any type of independence and
reaching their developmental milestones resulting in significant developmental delays
(27)
. Their
reduced ability to become mobile either by walking or using mobility devices, difficulties in self-care
and grooming and poor participation in play and educational activities occurs not only because of
their physical impairment but because they lack normal vision
(27)
.
It is clear that the treatment protocols for a child with a dual diagnosis of CP and visual
impairments cannot be similar to that of children diagnosed with either CP or visual impairment.
After thorough investigation this is now clear. It is also clear that there is a lack of research to
assist therapists with effectively treating children with neurological visual impairment as well as for
children with a dual diagnosis of CP and visual impairment
(28)(13)(27)
.
Therefore visual impairment cannot be overlooked during treatment. As professionals, there is a
necessity for occupational therapists to provide advice on the use of visual aids, refer to multi-
11
disciplinary team, make environmental adaptations to adjust for visual loss, and assist with family
and client needs to ensure quality of life
(19)
.
The treatment of CVI is not routinely taught at the undergraduate level in occupational therapy
although there is some training done in assisting people with low vision or blindness
(28)
. In South
Africa as in the United States (US), universities or training institutions can decide individually how
much time and credit is awarded to cover treatment for low vision and blindness at undergraduate
level
(28)
. This results in occupational therapists with varying degrees of knowledge and skills in the
treatment of people with visual impairments. There is no published information on how much
training is done at South African universities. A US study indicates that the training for visual
impairments is mainly directed at people with low vision or blindness who have no mobility
problems
(28)
. This highlights that there has been limited research done or training available to guide
therapists on how to assist children diagnoses visual impairment with an additional diagnosis of
CP.
Specific treatment interventions for children with visual impairment include but are not limited to
sensory integration approach, motor learning approach, visual perception model, biomechanical
frame of reference and the neurodevelopmental approach
(29)
. The sensory integration approach,
motor learning approach and neurodevelopmental approach will be discussed later in this chapter.
The biomechanical model can be used in the treatment of children with visual impairments. This
model is based on the principles of kinetics and kinematics which is the forces acting on the
human body during movement
(30)
. When applying this model during intervention the goal is either
to prevent deformity, restoring and or improving the person’s ability and capacity to move
(30)
. The
focus is to address basic client factors to improve occupational performance where ultimately the
goal is to engage the person in occupation
(30)
. To apply this for children with visual impairment the
therapist will try to improve the child’s mobility while providing appropriate assistive devices to
compensate for their lack of mobility due to their loss of vision. It is similar to the compensatory
approach however in the case of the compensatory approach the aim is not improving mobility but
rather compensating for the loss of mobility for this reason it would be quite difficult to use a pure
biomechanical model if the child with the visual impairment is diagnosed with CP as well as these
children have permanent loss of mobility which needs to be compensated for.
The visual perception model links closely with somatosensory stimulation and the sensory
integration approach and is aimed to enhance sensory processing through developmentally age-
appropriate activities. These activities must provide sensory stimuli that will promote the
12
development of client factors such as body concept, postural control, hand function amongst
others
(29)
. Treatment for children with a visual impairment would mean that vision is partially or
completely excluded so the child does not make use of this sense but rather learns to rely on other
senses
(29)
. Taking this into consideration this approach would be difficult to use for children with
visual impairments and then very difficult to use if the child has an additional diagnosis of CP as
there would be more client factors that would require compensation in order to reach
independence. It would be more beneficial to use a somatosensory approach and then to
compensate for the skills they lack in order to reach independence.
2.5 Theories, frames of reference and modalities used by occupational therapists for
children diagnosed with cerebral palsy and visual impairment
Occupational therapy intervention begin by determining a child’s physical, cognitive and
psychosocial performance and how this impacts on the child’s occupational performance or
activities of daily living
(31)
. The International Classification of Functioning: Disability and Health
(ICF) and the Occupational Therapy Practice Framework II (OTPF II) assist occupational therapists
in doing this
(31)(9)
. These frameworks focus on health and promoting the client’s strengths rather
than looking at their weaknesses, taking their activity limitations and restrictions into consideration,
to plan optimised treatment
(15)(9)
. The OTPF II uses the child’s occupational profile to determine
limitations in participation and outcomes which should be to make the child as independent as
possible
(31)(9)
.
The intervention process can then be guided by identifying the client factor and performance skill
deficits as defined by the OTPF II which is based on the ICF
(31)(9)
. Occupational therapists also
need to consider various frames of reference to guide them in planning appropriate intervention for
children with CP and visual impairment
(32)
. In the case of intervention for a child with a dual
diagnosis of CP and visual impairment, more than one frame of reference is often used during the
intervention process
(32)
.
According to a review of the practice area of children and youth by the American Occupational
Therapy Association (2011) the outcomes for intervention should cover the following four domains:
children should be able to participate in activities in a range of environments, interventions should
aim to prevent social isolation, interventions should encourage the child’s development of roles
and sense of competence and interventions should critically analyse transition periods and
facilitate or support moving through these transition periods
(33)
. This will ultimately help children
become active members of communities
(33)
. Interventions in line with the principles of the ICF and
13
the OTPF II will ensure that the child is evaluated and treated in their various environments, and
that their body function and structures are taken into consideration along with their personal
factors
(9)
. This is in line with previous discussions that interventions should aim to improve all five
domains of quality of life, as defined by the World Health Organisation, through addressing the
physical; educational and behavioural aspects of the child
(1)
. This will ensure that the child is
treated in the best way to encourage participation in activities of their choice, in line with their or
their families’ goals, and within age appropriate developmental stages
(33)
. Ultimately this will ensure
the child experiences quality of life
(1)
.
If occupational therapy interventions for children with a dual diagnosis of CP and visual impairment
are informed by the ICF and the OTPF II maximum participation within their strengths will be
ensured, while the influence of various frames of reference and approaches will be used to achieve
the child’s maximum potential
(33)
. It would furthermore indicate and augment the need for assistive
devices to enhance independence owing to adaptation to various environments being taking into
consideration
(26)(33)
.
Children diagnosed with CP always have motor impairments and thus experience loss of motor
control
(1)
. Interventions based on the ICF and OTPF II would then aim for holistic treatment
includes addressing the deficiencies in motor control
(9)(34)
. The basic unit of motor control is a
reflex. This can be controlled through the application of a sensory stimulus
(34)
. During treatment
this sensory stimulus can either facilitate or inhibit movement
(34)
. Reflexes assist with development
initially but they should integrate as the central nervous system matures
(34)
however when there is
damage or injury to the central nervous system reflexes cannot integrate and an individual might
struggle to gain control over these reflexes
(34)
. The damage inhibits the ability to process and
interpret the sensory stimulus resulting in impaired output which is then seen in the lack of motor
control
(35)
. This would then indicate the need for certain therapeutic approaches. When considering
a dual diagnosis of CP and visual impairment, the child would have even greater difficulty
interpreting the sensory stimulus. Therefore aligning interventions for a child with CP and visual
impairments with the ICF and the OTPF II would highlight appropriate measure that need to be
implemented in order to administer holistic treatment
(9)
.
Early theoretical approaches used for treating children with CP include Rood’s;
Neurodevelopmental and Somatosensory Developmental Approach. These approaches are all
based on the hierarchy and reflex principles and all are sensorimotor in nature
(34)
. Other
theoretical approaches and treatment interventions which will be described, include:
14
The somatosensory approach
(36)
and the Rood techniques
(34)
The sensory integration approach
(37)
The neurophysiological approach/Proprioceptive Neuromuscular Facilitation approach
(36)
including the constraint induced technique
(34)
The dynamic systems theory
(35)
The neurodevelopmental therapy approach
(38)
The Family centred approach
(20)
The multi-disciplinary team approach
(39)
The compensatory approach
(26)
Other approaches including cognitive approach and motor learning approach
(40)
After reviewing the literature it was clear that different literature use the words frames of references
and approaches interchangeable
(41)(42).
The list was compiled and reference made to either the
word approach or frame of reference as it was referenced in that specific reference site. The
definition for a frame of reference is to provide the platform for therapists to organise their
knowledge and enable the planning of intervention. This helps to link the theory to applying
treatment. It consists of several components including a theoretical base, evaluation, a
function/dysfunction continuum and suggests change
(30)
. The definition for a therapeutic approach
is the outline of a plan developed by the therapist in collaboration with the client to guide treatment
and is based on the relevant theories, frames of reference and available evidence. It is either
aimed to promote, restore, modify or maintain health or prevent further regression
(9)
. When
comparing these two definitions it is clear that they are similar in nature and both aim to combine
theory to knowledge and then enable the therapist to apply it in their treatment. Therefore for the
purpose of the report the therapist decided to use the word approach to prevent confusion and to
maintain continuity throughout the report.
2.5.1 Somatosensory development and approach
According to the literature reviewed, the somatosensory system refers to the interpretation of
sensory information in the brain that is received by sensory receptors located throughout the
body
(36)
. This enables a child to experience different sensations and so understand the position
and movement of the body. The somatosensory system along with vision, the vestibular system
and motor activity are seen as the regulatory mechanisms of postural control
(43)
. The visual system
is important for a child to develop cognitive and visual perceptual skills as vision provides the
15
necessary information to the brain of what is happening in the environment and also as to which
plane objects or the environment is being observed
(36)
.
The visual system also assists with balance and understanding the environment such as
determining the size of objects and spatial concepts
(36)
. Although the vestibular system can also
inform the brain of the posture and corrections needed for postural control the child would usually
also make use of vision to make postural changes to maintain balance and to understand the
environment
(36)
. In children with CP, poor postural control not only occurs as a result of muscle
weakness and poor biomechanical alignment but due to sensory disturbances as a result of injury
to the central nervous system
(43)
.
An occupational therapist may approach interventions for children with CP and visual impairment
through the development of the somatosensory system
(36)
. When making interventions to develop
the somatosensory system, the occupational therapist stimulates different senses to elicit specific
sensory responses
(36)
.
Applying specific and suitable sensory stimulation during therapy could enhance postural control
and improve the execution of functional activities and interactions with the environment
(43)
implying
that using this approach could be valuable in treating children with a dual diagnosis of CP and
visual impairment. Occupational therapists could use the visual and other sensory systems when
treating children with CP to facilitate motor responses and postural control
(36)(43)
. This is particularly
of value owing to the high possibility of damage to the proprioceptive system, causing a deficiency
in the supply of adequate information to the brain to improve balance and postural control due to
their complex brain injuries
(43)
. If the child has a visual impairment, it will be necessary for the
therapist to focus on stimulating the vestibular and other somatosensory systems during
therapy
(43)
. Stimulating the vestibular system would then provide feedback to the brain to make
postural changes and develop spatial concepts
(43)
. This approach could be used to manage
children with a dual diagnosis of CP and visual impairment, as it would consider visual impairment
while aiming to improve motor control.
In a study investigating the use of sensory information in the treatment of postural control in clients
with CP, Pavão, Dos Santos Silva, Savelsbergh & Ferreira Rocha (2014) suggests the problem
might be impairment to somatosensory systems
(43)
. This could be due to the multi-system
involvement, as previously explained
(11)
where there is impaired sensory processing due to a
decrease in white matter as a result of injury to the central nervous system
(43)(44).
This injury, in
turn, shows decreases cortical and thalamic regions, resulting in a decrease in projections to the
16
primary somatosensory cortex and thus less sensori-motor function
(43)(44)
. This could result in
sensory processing to be slow, misinterpreted or the sensory stimulation might not be processed at
all and thus unable to create the desired effect. This presents great difficulty when trying to use this
approach in the treatment of children with a dual diagnosis of CP and visual impairment
(13)(15)(8)
.
The use of different sensory stimulation should thus be approached with caution. A study by Valler
(1997) showed that using vestibular stimulation along with tactile and electric stimulation could
improve motor disorders and result in better movement however, in some instances it either had
no effect or worsened the condition
(44)
. The effect of the stimulation was also temporary
(44)
. Other
concerns raised with using sensory stimulation are that these children would have somatosensory
dysfunction leading to difficulty in interpreting and processing tactile and proprioceptive information
simultaneously. This results in impaired body awareness and poor exploration of the
environment
(45)
.
Nevertheless this approach can be of value and can assist during treatment interventions for
children with a dual diagnosis of CP and visual impairment although it must be used with caution
by an experienced therapist. It is also recommended to be used in conjunction with other
approaches in order to treat the child holistically as this approach neither takes the child’s family
into account nor the need for assistive devices
(43)(20)
. Therapists should also be aware of side
effects and, should they occur, therapists should be able to adjust therapy accordingly
(43)
.
Rood techniques
Margaret Rood developed sensory techniques based on the neurodevelopmental approach and
sensory motor development
(34)
. According to Rood, reflexes play an important role in the
development of motor control and these reflex patterns although unconsciously support the
voluntary control over movement
(34)(46)
. When there is neurological damage voluntary control is lost
and reflex patterns guide movement
(46)
. Rood believed that by applying different sensory stimuli to
a motor unit the therapist can either facilitate or inhibit muscle tone
(41)
.
Rood suggested that this technique can be applied as an adjunct to other approaches
(34)
. It should
also be done during the execution of a functional activity and repetition is needed for learning to
take place
(46)
. Considering these aspects this technique can assist in improving the effectiveness of
other approaches when making treatment interventions for children with CP in order to improve
movement and motor control
(41)
. As it would be applied in conjunction with other approaches, the
approach can be used when vision is impaired
(41)
.
17
Limitations in using this technique include the fact that it is impossible to consistently predict the
outcome of the sensory application as every person is unique and the effect of the technique only
lasts for the duration of the therapy hence there is no lasting effect
(34)
which emphasises the need
to use this technique only as an adjunct to other approaches
(34)
.
2.5.2 Sensory integration
Occupational therapists can use the sensory integration approach based on the work of Jean
Ayres which aims to organise sensory information for the brain to interpret, resulting in functional
behaviour
(47)
. Sensory integration is based on the neural plasticity and integrative function of the
brain
(37)(47)
and ultimately seeks to facilitate an adaptive response through applying enhanced
sensory input in a meaningful activity
(45)
. Taking this approach requires the provision of various
sensory opportunities with the “just right challenge” in order for the child to see it as a playful
experience where learning can take place through achieving success
(47)
.
The sensory integration approach was initially developed to assist children with learning
difficulties
(37)
but it was later found to be effective with treating children who are intellectually
challenged, children who had modulation dysfunctions such as hyperactivity, children who drooled,
and children who had seizures and praxis disorders
(47)(37)
. The approach was later applied
holistically when Ayres observed that children with sensory integration problems struggle with
learning as well as motor deficits
(45)
. Problems experienced with sensory integration are not as a
result of neurological damage but as a result of the brain being unable to organise sensory
information from the body or the environment
(45)
.
Researchers believed that by exposing a child to meaningful sensory experiences the brain will
develop and form new neural connections also known as neural plasticity and this will ultimately
allow for sensory reorganisation to occur
(45)
. Using the sensory integration approach, the
occupational therapist aims to assist the child in experiencing controlled sensory stimulation which
includes vestibular, tactile and proprioceptive input and apply it in meaningful activity
(47)
.
Sensory integration works from several assumptions
(45)(48)
: (i) The central nervous system is
plastic. Neural plasticity will aim for the restructuring of the brain as a result of continuous sensory
stimulation and sensory experience. (ii) The sequence of sensory integrative capacities, meaning
that sensory integration develops as the brain matures. The brain matures as it is exposed to
18
different sensory experiences. (iii) The brain functions as an integrated whole. The cortical and
sub-cortical areas functions as a unit and are interdependent. (iv) The brain functions as an open
system that allows for the brain organisation to result in adaptive behaviour and vice versa.
Sensory integration requires action from the individual (adaptive behaviour) in order to bring about
change in the central nervous system. (v) Every person is motivated to participate in everyday
activities. Every individual has an innate drive to develop through their sensori-motor functions.
The sensory integration has also embraced the fact that the brain functions as a whole. This
approach acknowledges the important connection between cortical and sub-cortical structures.
These assumptions are what distinguish sensory integration from sensory stimulation. Particularly
the fact that sensory integration aims for an adaptive response as oppose to sensory stimulation
which is more about the experience of the sensory stimuli
(37)
.
Children with CP are often referred to as multi-disabled, which imply extensive damage. Thus
there is a need to treat the brain as a whole and not only focus on individual brain structures
(17)
. By
critically analysing these assumptions separately, we can apply each of them when treating
children with CP. Using the principles of neural plasticity in the treatment of children with a dual
diagnosis of CP and visual impairment could apply as the aim would be to encourage myelinisation
and the formation of new neural connections
(49)(37)
. This could be of value as these children have
extensive brain injuries and new neural connections could result in establishing new motor
patterns
(49)(11)
. Occupational therapy aims to utilise various sensory experiences and carry out
activities that will encompass what motivates that person and encourages active participation in an
activity
(45)(37)
. These assumptions will again encourage neural plasticity and emphasize that
aspects of this approach can be used for children with a dual diagnosis of CP and visual
impairment
(45)(37)
. Furthermore, the use of this approach has shown success with children
diagnosed with CP, as shown after investigation by Berry and Ryan (2002
)
(32)
as well as in children
with dyspraxia, which is often seen in children with CP, and visual impairment
(50)
. Thus, it can be
concluded that aspects of this approach could be valuable in treating children with a dual diagnosis
of CP and visual impairment
(47)(51)
.
However contradicting findings by Parham and Mailloux (2010) and Van Jaarsveld (2005) have
expressed that the effectiveness of sensory integration in children with dyspraxia, which is a
problem often seen in children with CP as they struggle with motor impairments, is
inconsistent
(37)(47)
. Research remains limited and no studies were found on this approach
specifically in relation to children with a dual diagnosis of CP and visual impairment.
19
Important to note is that there are many neurophysiological considerations to take into account
when using this approach such as reception or the receptors that need to register the stimulus,
which is then placed in transduction and then encoded
(48)
and the process needs to be interpreted
at the level of the central nervous system and control needs to distributed
(48)
. These contradictions
can emphasise the need for therapists to have specialised training before attempting to apply the
sensory integration approach in treating a child with severe injury to the central nervous system.
2.5.3 Neurophysiological approach (proprioceptive neuromuscular facilitation)
The neurophysiological approach also referred to as the proprioceptive neuromuscular facilitation
approach in other literature is based on stimulating the somatosensory systems and makes use of
the somatosensory approach
(36)(44)
. The assumption in this approach is that learning takes place
through multi-sensory exposure, so by providing stimulation, the individual can learn movement
(46)
.
The neurophysiological approach aims to adapt the environment in such a way that movement is
made easier in order for the child to get sensory stimulation from the environment with each
movement
(36)
. This approach specifically emphasises the importance of postural stability for the
effective functioning of oculo-motor performance
(36)
.
Based on various aspects this approach can be positively applied in the treatment of children with
a dual diagnosis of CP and visual impairment. Techniques used in this approach include
strengthening stronger muscles, inhibiting reflexes, encouraging appropriate positioning and
making environmental adaptations and understanding and using influences from the environment
and the therapist
(46)
. By analysing these aspects many important therapeutic principles will be
addressed through intervention, including improvement of motor control, understanding and using
the child’s environment to their benefit, and making necessary environmental and positioning
adjustments
(8)(15)
. The approach is then applied in a functional activity to teach movement
(46)
which
is also very important to encourage neural plasticity
(49)
. Lastly if this approach focuses on postural
stability to encourage improved oculo-motor functioning the therapist can improve the child’s visual
skills and visual perceptual and visual receptive skills
(36)
. These aspects show the approach aims
to assist with independence in children with a dual diagnosis of CP and visual impairment and as
such can be appropriate to use for children with a dual diagnosis of CP and visual impairment
(41)
.
The challenges of using this approach, as mentioned in the literature were that the approach
becomes difficult to apply if movement and posture are greatly affected by tone
(36)
. After
investigating the use of this approach when treating children diagnosed with CP, Kielhofner (1997)
20
reported mixed and limited results
(46)
. There was also no literature that specifically made mention
of applying this approach specifically to children with a dual diagnosis of CP and visual impairment.
Constraint induced therapy
Constraint induced therapy is based on the clinical application of Edward Taub’s research on
improving upper limb function
(36)
. This technique is based on neurophysiology and requires the
occupational therapist to restrain the unaffected limb for at least six hours a day so that the client is
required to use the affected limbs
(36)
. It requires some motor control in the upper limb to elicit
movement and vision to plan and execute directed movement and is mainly used for hemiplegic
patients.
Many studies have reported this technique to be effective for children diagnosed with CP, with or
without visual impairment
(16)(36)(51)
. However in order to be functional and effective this technique
should be accompanied by other intervention approaches
(41)
.
It is difficult to implement this approach in treating children with a dual diagnosis of CP and visual
impairment as these children, most probably, have extensive brain injury
(11)(17)
.
This means they
would struggle to have some motor control in the upper limb and their vision would be affected and
for this reason the technique could be quite challenging to apply.
2.5.5 Dynamic systems theory
Dynamic systems theory was developed from the work of Nikolai Bernstein and aligns with
neurodevelopmental therapy which aims to learn new skills by way of experiencing movement and
how the environment contributes to the way we learn skills
(41)
. Dynamic systems theory suggests
that the individual, the task and the environment constantly affect each other
(35)
. This can either be
beneficial or detrimental to the client
(35)
. Intervention using this approach could be aimed at
affecting one or all three of these subsystems in order to bring about change and/or improve
independence. In order for the individual to interact with the task and the environment the task
needs to be fully explained. The individual encompasses the entire being of the person including
the cognition (the intent or motivation behind moving), perception (interpreting and processing
sensory input) and the action (implying the actual execution the movement)
(35)
.
Dynamic systems theory requires the child to actively participate in a realistic environment. It also
requires a therapeutic activity to be carried out in full
(35)
. The activity needs to comply with
21
principles of neural plasticity such as salience, intensity of training, transference, repetition and
active participation
(35)(49)
. Improvement is dependent on the level of the child’s engagement and if
the activity is matched at the level of the child’s skill, this would mean the child would be motivated
to actively participate
(35)
. The activity then needs to be transferred and generalised
(35)
, meaning the
skills acquired in one activity will need to be applied in other activities. Ketelaar (2010) suggested
that using a more functional approach rather than just looking at improving movement patterns
elicited better results
(41)
.
Secondly acknowledging neural plasticity principles when using this
approach would assist in establishing new neural connections, and as such, make the approach
valuable
(49)
.
Concerns raised with this approach are twofold: as taking this approach encompasses the child
being, the amount of variables need to be taken into consideration; and as this approach requires
great amounts of control, thus having the potential to inhibit development, the environment and the
activity need to be carefully considered
(41)
. Furthermore the dynamic systems theory undermines
the influence of the central nervous system
(35)
. This is especially of concern when trying use this
approach when treating children with a dual diagnosis of CP and visual impairment as they have
extensive brain damage
(41)
.
2.5.6 Neurodevelopmental therapy approach
The neurodevelopmental therapy approach is founded on the learning of new skills, movement and
ideas by experiencing movement. Neurodevelopmental therapy is based on the work of Karel and
Berta Bobath, and was developed along with the dynamic systems theory and motor learning
(38)
.
The main aim of this approach is to assist in the control of posture and motor coordination
(41)(51)
.
This is a hands-on approach to be used while the therapist tries to influence motor deficits by
correcting abnormal patterns of movement and posture and inhibiting the abnormal reflexes
(38)
.
The assumption underlying neurodevelopmental therapy is that impairment in the sensorimotor
systems affects the entire individual and thus requires therapists to apply hands-on sensorimotor
techniques to bring about change in the individual’s movement patterns
(41)
. The technique is based
on the quality of touch which includes preparation of the child then facilitating movement and
inhibiting abnormal patterns
(15)
. There is also a strong link between the use of this approach and
making use of adaptive equipment and optimal positioning
(38)
. Movement is linked to the sensory
input which develops first through feedback then progresses to feed forward learning and it
22
requires active participation from the client in a functional activity
(41)
. The ultimate aim of this
approach is to optimise functioning through encouraging optimal movement patterns
(38)
.
There are many factors that indicate the value of taking this approach when treating children with a
dual diagnosis of CP and visual impairment. Firstly it can assist with correcting the alignment of the
head and the eye muscles and thus improve eye movement and vision
(8)(15)
. Literature supports the
use of assistive devices in this approach which according to Schoonover, Argabrite Grove &
Swinth (2010) who investigated how assistive devices can influence participation, is invaluable in
assisting with achieving independence
(26)
. Another important factor contributing to the value of
taking this approach is that it includes many principles of neural plasticity: therapy must be
presented in a functional activity; therapy must encourage active participation of the child; therapy
must require intense training with repetition and transference of skills which encourages the
improvement of motor control
(41)(49)
. According to literature by O’Brian and Williams (2010) and a
study by Butler and Darrah (2001) who reviewed studies by Trahan and Malouin (1999); Bower
and McLellan (1994); Mayo (1991); Carlsen (1975) and Scherzer, Mike, & Ilson (1976) who
investigated the effectiveness of this approach in areas such as improving gross motor functioning
and acquisition of motor skills as well as parent satisfaction all reported results that have shown
success when using this approach
(41)(38)
.
Although therapists have had success, the approach, according to Sugden and Dunford (2007)
and Butler et al. (2001) still rendered inconsistent results
(51)(38)
. Some studies compared the
neurodevelopmental therapy approach with other approaches and found that participants had
better results with alternative treatment approaches as conducted by D’Avignon (1981) and
Palmer; Shapiro; Wachtel; Allen; Hiller & Harryman (1988). After reviewing other studies by Butler
et al. (2001) showed that the condition of the participants who were treated by means of the
neurodevelopemental therapy approach did not improve however, they were not harmed during
the treatment
(41)(38)
. Lastly Stanger and Oresic (2003) reported that there is still insufficient
evidence to support the effectiveness of this approach
(16)
.
Results are varied with regards to the success rate of taking this approach in the treatment of
children with a dual diagnosis of CP and visual impairment
(38)
. Reasons for these mixed results or
ineffectiveness include that this approach requires many specific principles that are not always
easy to uphold such as that therapist must be hands-on, and it requires very intense and specific
therapy, and if clients are inconsistent in their consultations it would affect the outcome
(41)
.
23
Literature reviewed also suggests that therapists’ knowledge sometime varies with the use of this
approach. This can result in inconsistencies regarding outcomes
(41)(38)
.
2.5.8 Family-centred approach
When adopting the family-centred approach the occupational therapist consults with the child’s
parents as experts of understanding the child wants and needs
(20)
. To apply this approach, the
family and the client must be involved in the rehabilitation process and their ideas must be
respected and considered during treatment
(20)
. This approach encourages the family to establish
realistic and relevant goals through identifying and prioritising their needs
(52)
. A study conducted by
Jeglinsky; Autti-Rämö & Brogren Carlberg (2010), which investigated the family-centeredness of
rehabilitation teams proved that once a family-centred approach is used, parents are more
satisfied with the rehabilitation process and are also more cooperative
(20)
. The family-centred
approach would then ensure greater compliance and receptiveness with information, education,
training and home programs given
(20)
. Oien, Fallang & Ostensjo (2009) also found that once family-
centred goals are established and functioning the families found it easier to use every day activities
as learning opportunities, which in turn could enhance the achievement of goals
(52)
.
There are four general domains to following a family-centred approach: showing interpersonal
sensitivity, providing specific information, providing general information and treating others with
respect
(20)
. Jeglinsky et al. (2010) proved that when professionals work in a multi-disciplinary team
the family-centred approach and these four domains are adhered to and enhanced
(20)
. This is
because the entire team provides education, training and information implying all of the needs of
the family are addressed. Jeglinsky et al. (2010) also stated that medical practitioners with more
experience in the field of rehabilitation seem to be better at providing the service guided by a
family-centred approach, thus improving satisfaction as well as compliance of the clients
(20)
.
In this sense, aspects such as implementing various home programs, providing assistive devices,
and ensuring training to continue at home would be implemented easier and be more sustainable.
The reason for this is that the family would be more involved in therapy and as their needs are
supported they would be more willing to continue with the process at home
(20)
. Another study by
Law, Darrah, Pollock, Wilson, Russel, Walter, Rosenbaum & Galuppi (2011) has proven that when
therapists adopt a family centred approach it does not matter if context-focus therapy or child-focus
therapy is used, as the outcomes do not change much owing to the family’s goals being reached
24
and they are more satisfied with therapy and more compliant with home programs and
exercises
(53)
.
This would be especially beneficial for children with a dual diagnosis of CP and visual impairment
as often these children are multi-disabled and it is very difficult to determine goals for the child. By
making use of a family-centred approach, the therapist ensures that the goals they are working
towards are attained and that therapy continues at home, which would improve outcomes and
enable an improvement in quality of life. This approach would be beneficial to adopt when treating
children with a dual diagnosis of CP and visual impairment in conjunction with a motor control
approach
(53)(41)
.
Although the disadvantages of adopting this approach are negligible, using this approach should
form part of a holistic treatment process, especially for children with a dual diagnosis of CP and
visual impairment. This approach on its own will not necessarily improve the child’s functioning so
it must be emphasised the family-centred approach be used in conjunction with other approaches
aimed at improving or maintaining the impairments found in these children to improve
independence.
2.5.9 Multi-disciplinary team approach
A multi-disciplinary team comprises specialists from different areas in health care who have expert
knowledge and skills in their field of practice
(39)
. These team members collaborate to ensure that
they provide the best care for each patient
(39)
. When considering the multi-system involvement and
extensive injuries a child with a dual diagnosis of CP and visual impairment has, it is of utmost
importance that they be treated by a multi-disciplinary team
(11)
.
A study in Kenya conducted by Njambe et al. (2009) found value in occupational therapists
working with ophthalmologists
(11)
. Visual abnormalities are very common in children with CP and if
occupational therapists can identify the visual impairment and liaise with ophthalmologists these
impairments can be addressed and the children often show improvement especially if this is done
in conjunction with visual and physical rehabilitation
(11)
. Visual rehabilitation includes using bright
colours and lights while addressing physical concerns
(11)
.
As discussed earlier in this chapter, intervention regarding the domain of physical rehabilitation
involves strength training
(27)
. This is an area in which physiotherapists are very much involved
25
highlighting once again the importance of a multi-disciplinary team when ensuring that best
practice is followed
(15)
.
Jeglinsky et al. (2010) proved that when therapists work in a multi-disciplinary team, the family-
centred approach is enhanced and goals are attained more effectively
(20)
.
Critically reviewing the use of a multi-disciplinary team would ensure that clients and their families
would be treated and managed holistically, and thus best care would be provided.
2.5.10 Compensatory approach
The compensatory approach is used to enable a child’s functionality towards becoming more
independent in the presence of severe cognitive or physical limitations. This approach is adopted
by means using adaptive equipment and/or assistive technology
(26)
. It differs from the
biomechanical model in that it is rehabilitative in nature and compensates for the lack of ability
rather than improve ability as in the biomechanical model. The compensatory approach aims to
use the client’s current abilities and couple it with adaptive equipment and/or assistive technology
to achieve occupational performance
(42)
. It is commonly used in combination with other therapeutic
approaches as it is only used as a means to accomplish the final outcome if all other approaches
have failed, either in specific outcomes or as an adjunct to assist in reaching goals with the use of
other approaches
(32)
.
The compensatory approach makes use of splints, orthotic devices or
assistive technology
(26)
. Splints and orthotic devices aim to ensure maintenance of joint range, joint
protection and/or improvement of function
(16)
. These splints or devices are custom-made and
should always be accompanied with a wearing schedule to ensure that the primary goal is reached
and also to ensure correct usage and maintenance of the device
(16)
.
Assistive devices have similarities in their aims, however the primary goal is to improve postural
control or support and increase participation in the community or school
(26)
. Assistive devices are
defined as any item, piece of equipment or product system that can be acquired commercially or
are custom-made, however, modifications are often necessary to fit the individual’s specific
need
(16)(26)
. In order for a therapist to make these modifications specialized training and education
is often required
(16)
. This includes knowledge of equipment and insight in ordering, fitting and
matching the equipment to the client’s specific needs
(16)
. Assistive technology is typically divided
into five categories including postural support or seating systems, wheeled mobility, augmentative
26
and alternative communication, computer access and electronic aids to assist with activities of
daily living
(16)(26)
.
A major problem faced when adopting this approach in South Africa is that assistive devices are
often expensive and not readily available to the majority of the population
(2)
. This highlights the
importance of a family-centred approach, as the team would then know what devices the family
would use and can afford
(20)(26)
. The combination of these approaches could thus be utilised when
treating children with a dual diagnosis of CP and visual impairment
(16)(20)
.
Advantages of this approach include: children with CP often require seating devices or
splints/orthotic devices to improve mobility or maintain function
(16)
, and children with visual
impairments often require assistive devices to accommodate for their lack of vision including
spectacles and other electronic aids to compensate for lack of vision such as computers
(16)
. Thus,
with the help of the family-centred outcomes assistive devices could be customised to optimise the
quality of life for these children
(20)
. This would also address the challenge faced by children with a
dual diagnosis of CP and visual impairment, where they struggle to use their assistive devices, as
their families would assist them in using these devices or continue teaching them to use the
devices at home
(20)
.
Schoonover et al. (2010) reported that the use of assistive devices ultimately assists therapists to
ensure maximum independence is reached
(26)
. Thus, if applied correctly, using assistive devices
will ultimately ensure that these children experience quality of life and reach maximum
independence in the achievement of age appropriate milestones
(1)(26)
.
2.5.11 Other approaches: Cognitive approach and motor learning
Other approaches mentioned in research are not supported for the majority of children with a dual
diagnosis of CP and visual impairment.
The cognitive approach developed from the theory of Albert Bandura is a top-down, occupation-
based approach
(40)
in which the child is expected to develop cognitive strategies while participating
in task-specific activities. The therapist only guides the experience while the child explores various
strategies. These strategies are then generalised for application in more complex situations
(40)
. The
concern with this approach is that it is not suitable for children younger than five years. Even
though the approach has been adopted for children with CP, there is no research to support its use
27
for children with a dual diagnosis of CP and visual impairment
(40)
. As this approach also requires
the child to develop complex cognitive strategies, it is highly unlikely that it would be appropriate
for the majority of children with a dual diagnosis of CP and visual impairment. Reasons for this
include that these children generally have severe brain damage, thus could have cognitive
impairment, making it impossible to develop complex cognitive strategies
(17)(4)
.
The motor learning and skill acquisitions approach is strongly influenced by the dynamic systems
theory and other motor control theories
(36)
. It differs from other motor control theories in that it
places specific emphasis on the stage of learning. It also does not focus on motor control
difficulties as a result of a lesion but more on the systems that can be altered to change
movement
(36)
. Even though it focuses on the child being an active learner and the therapist as a
guide and facilitator, research is limited to show success with this approach
(36)
. No evidence exists
to confirm that this approach could be valuable when treating children with a dual diagnosis of CP
and visual impairment. Also considering that they might be multi-disabled with severe motor
impairments it would be very difficult for them to move through the stages of motor control
(36)
.
Although notable, the cognitive approach and the motor learning and skills acquisition approach
are not suitable for the treatment of children with a dual diagnosis of CP and visual impairment.
There was no evidence found in the literature to support these two approaches for these children.
2.6 Evidence based practice
In exploring the most suitable therapeutic approaches and investigating what is best to apply for
children with a dual diagnosis of CP and visual impairment it remains important to understand how
this is defined. Sacket’s (1996) definition is the most common used when describing evidence
based practice
(54)
in which evidence-based practice is regarded as the usage of unambiguous,
clear and up-to-date information that is thoroughly researched and judged, then applied specifically
when making decisions in the care of each individual client
(54)
. Part of this meticulous process
involves integrating that information with own clinical expertise
(54)
. Bennet and Bennet (2010)
expanded this definition further stating that research should strengthen, not replace, a therapist’s
clinical expertise
(55)
.
This raises the question as to the nature of clinical expertise which is described as a combination
of education; work experience and clinical training
(54)
. This implies that once research is done, in
28
order for the acquired knowledge to be applied, therapists need to make their own judgements
based on their clinical expertise. This would ensure client’s own values, concerns, goals and
culture are taken into consideration and best practice is followed
(54)
. Bennet et al. (2000) describe
best practice as the integration of research with clinical expertise as well as client’s expectations;
values and ideas
(55)
.
Another link to clinical expertise is the therapist’s perceived competence. Perceived competence
refers to how a person values his/her own skills and talents and the ability to control their
surroundings
(56).
This informs the manner in which the person perceives their skills in a particular
situation
(56)
. This process is important as it ensures that the clients receive the best care possible,
that available research and current practice is integrated and applied and that the client is
respected and his/her needs are appropriately cared for
(55)
.
In occupational therapy one of the models that have been described to assist therapists in applying
and using evidence-based approaches is named Systematic Occupational Therapy Practice model
or SOTP. It serves as a means for therapists to follow sound practice
(57)
. This model guides
therapists to integrate scientific thinking with action in all domains of practice in other words it is the
organised process where research is applied to the process and outcome of intervention
(57)
. It will
provide therapists with the opportunity to determine which intervention strategies will achieve the
desired outcome and what new knowledge needs to develop
(57)
. The reason why this model is so
effective is because it addresses the three critical areas from external demands. Firstly location
and time of service delivery which has been described as a problem in the South African context
thus needs to be considered during the intervention process. Secondly the process provides
therapists with the opportunity to provide sound scientific practice to consumers, insurers, policy
makers and other professionals. Thirdly it enables inter-disciplinary communication as it shares
language and theory with other disciplines
(57)
.
The SOTP consists of five steps including
(57)
: 1. To identify and clarify the problem. 2.
Understanding the needs to enable solutions to the problem. 3. Goal setting to address the need.
4. Reflecting during intervention to ensure goals are reached. 5. Outcome assessment. These
steps are advised to follow to ensure best practice is rendered to clients at all times.
Reasons for why therapists do not always follow models such as the SOTP to ensure best practice
was described by Benevides, Vause-Earland & Walsh (2015) and included: limited time, a lack of
29
resources for relevant literature, poor support from their respective organisations, lack of skills in
interpreting the research and data and decrease competence in applying new knowledge
(58)
.
Benevides et al. (2015) found that even though therapists reported a lack of organisational support
all therapists had a positive attitude towards evidence-based practice and felt it was necessary to
align their intervention with it
(58)
. The differences between therapists who had support and those
who did not have organisational support as reported by Benevides et al. (2015) was in the
therapists’ understanding of research concepts and their application of new knowledge and skill of
evidence-based practice
(58)
. This implied that even though therapists felt that all intervention
approaches should be aligned with best-practice, therapists were not always able to apply their
research done in a specific field practically. There were no specific studies linking the process of
evidence based practice specifically to the treatment of CP and visual impairment however each
approach was discussed in light of the best practice for these children.
2.7 Conclusion
A literature search on the combined topics “occupational therapy, CP and visual impairment”
rendered no articles. A search for the combined topic “CP and visual impairment” rendered 50
articles, of which seven were clinical trials, and three were randomised control trials, published in
the last five years. None of these articles are specifically based in the field of occupational therapy.
A search for “occupational therapy and CP” rendered more than 200 articles published in the last
10 years. However this includes all types of occupational therapy interventions such as splinting
etc. with just 36 articles based on randomised control trials. A search for the terms “visual
impairment and occupational therapy” rendered 255 articles but “visual impairment” is not specific
to children diagnosed with CP, so a search for “occupational therapy” along with “neurological
visual impairments” rendered just 15 articles highlighting that there is limited published research on
the combined treatment of children diagnosis with CP and visual impairment
(13)(15)(8)
.
This lack of scientific evidence confirmed earlier in this chapter during the discussions on each
therapeutic intervention, as very few of these approaches provided clear evidence on whether they
would be effective in the treating children with a dual diagnosis of CP and visual impairment. What
became clear, however, is that these interventions are best used in combination and through
thorough investigation there are approaches that have shown more success than others. This can
only be clear to therapists if they follow the procedures of evidence-based best practice and
integrate it with their clinical experience.

30
Chapter 3: Research methodology
3.1 Study design
A descriptive, non-experimental, cross-sectional research design within a quantitative research
approach was selected for this study
(59)
. The data was not manipulated in any way, and was used
only to describe the population and their work experience
(59)
. A cross-sectional design was used as
the respondents were from different genders, had varying educational qualifications, and various
numbers of years of experience. The data was collected in a set time period while adhering to a
deadline, and all data was presented numerically, therefore a quantitative approach was used.
Data was analysed statistically
(59)
and so the research design chosen was the best option for this
study.
As there was limited literature available to describe the combination of interventions for children
with a dual diagnosis of cerebral palsy (CP) and visual impairment, this research was conducted to
describe occupational therapy interventions. A phenomenon must be described for it to be
measured and describing and measuring the phenomenon was the aim of this study. The study
used a uniquely designed questionnaire to obtain information and presented this information
analytically.
3.2 Population
The study population consisted of all occupational therapists in South Africa registered with the
Occupational Therapy Association of South Africa (OTASA) and the Eastern Cape Occupational
Therapy Forum, the provincial body for occupational therapists working in the public sector in the
Eastern Cape.
The population included all therapists registered with OTASA estimated at about 1 700.
Additionally, those who attended the Eastern Cape Occupational Therapy Forum (about 120
therapists) were added to the mailing list. There might have been duplication in the lists as some of
the therapists might have belonged to both OTASA and the Eastern Cape Occupational Therapy
Forum.
31
3.3 Sampling
The study used purposive sampling
(59)
. Only those who met the inclusion criteria were asked to
participate
(59)
. These criteria were:
Inclusion criteria:
Occupational therapists with a minimum of six months working experience with children
with a dual diagnosis of CP and visual impairment.
Occupational therapists working in either the public or the private sector, or both.
Exclusion criteria:
Occupational therapy students.
The five occupational therapists used in the pilot study.
The questionnaire was not sent to specific occupational therapists. By using these national and
provincial bodies the researcher made use of their system-generated email process and emails
were automatically sent to all the members of these respective bodies. This made the total sample
size about 1 820, but only clinicians who met the inclusion criteria were asked to participate in the
study. All the completed questionnaires were used for data collection
(59)
. The respective bodies do
not keep record of how many of their members specialise in certain fields such as cerebral palsy
and so it was impossible to determine the sample size as there is no way of knowing how many
occupational therapists work in this specific field. As a result all completed questionnaires were
analysed.
3.4 Development of the measurement tool
The researcher had to design a measurement tool based on relevant literature, discussed in the
literature review, as there were no measurement tools available to assist clinicians working with
children with a dual diagnosis of CP and visual impairment. The questionnaire was divided into
three sections. It was electronic and designed on Survey Monkey ®. (See Addendum B) Survey
Monkey ® is an electronic based website where anyone can design and post their own survey and
allows access to anyone who receives the link to the survey
(60)
.
To ensure all participants had a good understanding of what was meant by visual impairment, a
brief summary was included with definitions from literature explaining the visual impairments seen
in children with CP.
32
The survey questionnaire consisted of three sections. These included:
Section A: Demographic information and work information: This section consisted of five
closed-ended questions and five open-ended questions on the sample population’s background;
work environment and caseload of children with CP and visual impairment.
Section B: Current practice including the theories and approaches of current occupational
therapy practice: This section contained two subdivisions. Section B.1 comprised six questions
on therapists’ undergraduate and postgraduate training for managing children diagnosed with CP
and visual impairment. Section B.2 comprised five questions on the treatment methods used when
managing children with a dual diagnosis of CP and visual impairment. This section used closed-
ended questions based on the literature discussed in Chapter 2. The majority of the closed-ended
questions used a Likert scale to derive answers. The Likert scale was taken from literature and is a
five-point scale to indicate various choices
(61)
. The participants had to choose the most appropriate
answer for agreement (strongly agree, agree, neutral, disagree or strongly disagree) and
frequency (always, very often, sometimes, rarely or never). For other closed-ended questions
participants were asked to mark the most appropriate responses. Parts of certain questions were
written in capital letters to highlight nuance and subtle differences.
Section C: Participants’ perceptions on their knowledge and skill: This section was also
divided into two subsections. The first contained two closed-ended questions on the participants’
perceptions of their undergraduate training for the management of children with a dual diagnosis of
CP and visual impairment and used the Likert scale for agreement. The second subsection
contained 10 questions, four of which were closed-ended questions using the Likert scale for
agreement and for quality (very good, good, barely acceptable, poor or very poor) on how the
participants rated their skill/knowledge and six open-ended questions to ascertain the therapists’
knowledge, skill and perceived confidence. It included questions on participant’s outcomes which
links to how participants use their knowledge and skill of the different theories and approaches to
plan treatment. This section also contained a question to determine the participants understanding
of evidence-based practice. These questions were based on the literature reviewed.
3.4.1 Pilot testing
A pilot study was conducted to test the validity and reliability of the questionnaire’s content to
assess whether the questions were clear and specific enough for participants to follow
(59)
. It further
helped to assess whether the questionnaire served its purpose to obtain information to describe
33
occupational therapy practice for children diagnosed with CP and visual impairment. The
questionnaire was sent to five therapists that met to the inclusion criteria. These occupational
therapists have various levels of experience in this particular field. Convenient sampling was used
to select participants for the pilot study
(59)
. This group was selected from a group of therapists who
worked with the researcher and the researcher was familiar with their levels of experience.
Pilot study participants included:
an occupational therapist with experience working at the Cerebral Palsy Association in the
Eastern Cape;
two occupational therapists from the Port Elizabeth Hospital Complex: one of whom had at
least three years, and one less than one year’s working experience; and
two therapists from the immediate district.
The participants for the pilot study were approached by the researcher with the information letter
and study objectives, and asked to complete the questionnaire. They were asked not to participate
in the main study. Feedback was given verbally with each individual participant to determine
whether the questions were clear, unbiased, and if the pilot participants had any difficulties
answering the questions. To establish content validity for this questionnaire the pilot group was
asked to indicate clarity, simplicity and ambiguity of each of the questions on a scale of 1 – 4
according to a validity measurement scale
(62)
. The scale was labelled: 1. Not relevant/clear/simple
or doubtful; 2. Question needs some revision; 3. Relevant/clear/simple or no doubt but needs
minor revision; and 4. Very relevant/clear/simple or meaning is clear
(62)
. They were given the
opportunity to make suggestions for additional changes to the questions. Completing the pilot
study and making the necessary amendments after interpreting the pilot group’s feedback it
improved the study’s validity. The final questionnaire was then sent out.
Feedback received from the pilot study group was examined. An issue raised was that some
questions appeared similar, which is why the researcher chose to write certain parts of the
question in capital letters for emphasis. The pilot study participants suggested that the researcher
should define the different visual impairments as participants might not be familiar with a certain
visual impairment or can interpret it incorrectly. The pilot study participants indicated in Section C
that the treatment of these children should be evidence-based, however, some of the members of
the sample population said they were unclear about what evidence-based treatment mean so a
question was added to determine what participants understood by evidence-based and
34
scientifically proven treatment. Lastly, the pilot study participants indicated that the question in
Section C about therapeutic outcomes was unclear. This question was then broken down into
three questions: the immediate functional aims of each session; the long term outcomes; and the
principles they followed during treatment. The amended questionnaire was resent to all five
participants. They found the changes to be acceptable and concluded that the questionnaire was
ready to be sent out for data gathering.
3.5 Data collection
Data was collected through an electronic uniquely designed questionnaire designed using Survey
Monkey® and the link was sent out via emails to the therapists through the OTASA website and
the Eastern Cape Occupational Therapy Forum.
The email contained an information letter about the study, and prospective participants were
asked to complete the survey by following a link sent to them via the emails. No consent form was
necessary as participation was seen as consent. Participants clicked on the appropriate answers
in the survey and submitted them on the Survey Monkey® site where the researcher had access
to the results. The survey took less than 20 minutes to complete.
Participants were asked to try to answer all the questions although they were allowed to refrain
from answering questions if they chose to do so. All participants were kept anonymous except for
the link to their IP addresses. They were not required to provide their name or contact details.
Bias was minimised through the use of an information letter that requested participants to refrain
from speaking to one another about the questionnaire to prevent duplication of answers and/or
influencing other participants. The information letter requested that participants complete the
questionnaire only once to ensure that there was no duplication between the questionnaires
particularly by therapists belonging to both OTASA and the Eastern Cape Occupational Therapy
Forum.
3.6 Data management
Responses were stored on the Survey Monkey® database and exported into Microsoft Excel
spreadsheets and Microsoft Power Point to create graphs and tables for data analysis. The
researcher had access to all completed questionnaires and was able to double check that data
compiled in Microsoft Power Point corresponded with data on Microsoft Excel spreadsheets.
Survey Monkey® automatically exports all graphs to Microsoft Power Point and even though all

35
graphs were created by the researcher in Microsoft Excel it was useful to compare data and
graphs with those automatically created in Power Point. New graphs were created in Microsoft
Excel as the researcher were not able to make any changes to the graphs in Power Point and as
such if the researcher wanted to present data differently graphs needed to be available in
Microsoft Excel.
3.7 Ethical considerations
The study commenced only after ethical clearance (Ethical Clearance Number M130936) was
given by the University of the Witwatersrand’s Human Research Ethics Committee (See Appendix
C). The questionnaire was supported by an information letter. (See appendix A) The information
letter emailed to prospective participants informed them of the purpose of the study, the population
criteria and about their right to withdraw from the research at any time.
The completion and return of the questionnaire served as consent to participate. The questionnaire
was completed in the occupational therapists’ own capacity and not through their department thus
it was not necessary to get departmental permission or permission from the Department of Health.
All participants were kept anonymous to protect their professional integrity. This was done through
Survey Monkey® as well as by refraining from using confidential information in the questionnaire.
After completing the survey the only link to the participants was an IP address, which ensured the
researcher could not obtain any personal information.

36
Chapter 4: Results
This chapter reports on the data collected and presents the results of the study in a structured and
logical manner. The data reported on includes the participants’ background information, their
knowledge, skill and perceived confidence in the different treatment approaches when managing
children with a dual diagnosis of cerebral palsy (CP) and visual impairment. It will also reflect on
the participants’ short- and long term outcomes and principles in treatment when managing
children with a dual diagnosis of CP and visual impairment and lastly what participants’ opinions
are on their education and what they perceive as evidence based practice.
Descriptive statistics were used with quantitative aspects
(59)
. Using the Likert scale enabled the
researcher to present data in numerical scales using graphs and tables to display cross-
tabulations. It showed the mean and confidence intervals of the data the open-ended questions
were analysed and interpreted by looking for similarities and frequency in the answers.
Data was transferred from existing Microsoft Excel spreadsheets and Microsoft Power Point slides
to new spreadsheets in which the researcher grouped data into specific categories determined by
the questions. The researcher displayed the data according to the number of participants and
percentiles for all closed-ended questions. As participants were given the option not to answer
questions the total participants for each question was not always the same.
Open-ended questions were interpreted through analysing similarities and the frequency of words
used, and were then transferred and displayed graphically.
4.1 Demographics of the participants
The response rate to the survey was 3.4% of the 1820 occupational therapists to whom the survey
was emailed. Of the 62 occupational therapists who completed the survey, only 47 provided
complete responses to all the questions. The survey was posted for an extended period to
maximise participation and emails were sent to various bodies to encourage and remind possible
participants to complete the questionnaire.
4.1.1. Gender
One man and 61 women participated in the survey.
37
Table 4.1.1 Gender distribution of the participants (n=62)
Participants
Percentage (%)
n = 62
Male
1
1.6
Female
61
98.4
4.1.2 Educational background of the participants
The section focussed on the participants’ undergraduate training and experience. Participants from
various universities across South Africa took part in the study. The majority were from the
University of Cape Town (19.4%), followed by the University of the Free State (17.7%), and the
University of the Witwatersrand (16.1%). At the other end of the scale, one participant studied at
the Pretoria College of Occupational Therapy, one at Brunel University, London, and one at the
University of Edinburgh, Scotland.
The majority of the participants (58.0%) had qualified in the past ten years indicating that many of
the participants had only ten years’ or less work experience, whereas 21.1% of the participants
had between 10 – 20 years’, and 20.9% had 23 years’ or more.
Table 4.1.2 Undergraduate training and year qualified (n=62)
Qualifications
Participants
Percentage
Undergraduate training
n = 62
University of Cape Town
12
19.6%
University of Free State
11
17.7%
University of Stellenbosch
9
14.5%
University of Limpopo
6
9.7%
University of Witwatersrand
10
16.1%
University of Kwa-Zulu Natal
4
6.5%
University of Pretoria
7
11.3%
Other universities
3
4.9%
Year qualified
1966 – 1977
2
3.2%
1978 – 1989
11
17.7%
1990 – 2001
13
21.1%
2002 – 2012
36
58.0%
38
4.1.3 Participants’ report on further training in the rehabilitation of children diagnosed with
cerebral palsy
In this section participants had to report on additional courses they had attended or training they
had received that focused on the rehabilitation of children diagnosed with CP. Participants could
indicate all courses they attended and for this reason courses attended does not add up to the
number of participants with further training. This implied that some participants attended more than
one course. The majority of participants (74.2%) indicated they had received further training on the
treatment of children with CP. None of the participants, however, had received a diploma or
masters degree specifically applied to the treatment of CP. The most common course attended by
48% of the participants was the South African Neurodevelopmental Therapy Association’s
(SANDTA) eight week basic paediatric neurodevelopmental therapy (NDT) course. The second
most common course attended by 28% of the participants was the association’s one week
introductory course to the management of CP.
Other courses included Hambisela training and the Buggy seating course. Hambisela training is a
course to provide therapists with the knowledge and equipment to implement training workshops
for the caregivers of children with CP. The Buggy seating course is a wheelchair seating course to
educate therapists on the proper seating of children with CP and other neurological disabilities.
39
Table 4.1.3 Participants’ further training in the rehabilitation of children diagnosed with CP
(n=62)
Participants with further
training in rehabilitation of
children diagnosed with CP
Participants
(n=62)
Percentage
Total participants with further
training
46
74.19%
Total participants without further
training
16
25.81%
Training included:
8 week basic paediatric NDT
course
22
48%
One week introductory CP
course
13
28%
Buggy seating course
4
9%
Other workshops and training
related to CP
4
9%
Other SANDTA course
3
7%
Sensory integration training
2
4%
3 week Adult NDT course
1
2%
Hambisela training
1
2%
4.1.4 Participants’ work information
This section gathered information on the participants’ experience in working with and managing
children with CP, as well as their work setting. The experience of the participants working with
children with CP ranged from 22 (35.5%) participants with more than 10 years’ experience to three
participants (4.8%) who had less than one year of experience.
More than half of the participants (54.8%) worked in the public sector. The majority reported that
they worked in hospitals (43.6%) while 35.4% worked in private practice. Community work was the
area least represented, by only 6.5% of participants.

40
Table 4.1.4 Participants’ years of experience with CP, current field and area of work (n=62)
Work experience
Years of experience with CP
Participants
(n=62)
Percentage (%)
0 - 1
3
4.8
1 – 2
10
16.1
2 – 5
15
24.2
5 – 10
12
19.4
More than 10 years
22
35.5
Field of work
Participants
(n=62)
Percentage (%)
Public
34
54.8
Private
18
29.0
Both
10
16.1
Area of work
Participants
(n=62)
Percentage (%)
Hospital
27
43.6
Clinic
5
8.1
Community
4
6.5
School
12
19.4
Private practice
22
35.4
NGO
7
11.3

41
4.1.5 Participants’ reasons for attending post graduate training in the form of courses,
diplomas or degrees.
This section gathered information on reasons for attending further training in the rehabilitation of
children with CP. The tables presented number of participants.
In the first section participants were asked whether they had attended training to improve their
skill and knowledge. More than half (32 participants which is 52.5%) agreed and 16 (26.2%)
strongly agreed, while a minority group of two (3.3%) participants disagreed and four (5.3%)
strongly disagreed.
Figure 4.1.5 (a) Reason for attending postgraduate training was to improve knowledge
and skill (n=61)
The second section gathered information on whether the participants’ reason for attending
courses was to improve their management of children with CP and visual impairment. Here, 33
participants (54.1%) agreed with this statement and 15 (24.6%) strongly agreed; none
disagreed, and only two (3.9%) strongly disagreed.
0
5
10
15
20
25
30
35
Strongly agree Agree Neutral Disagree Strongly
disagree
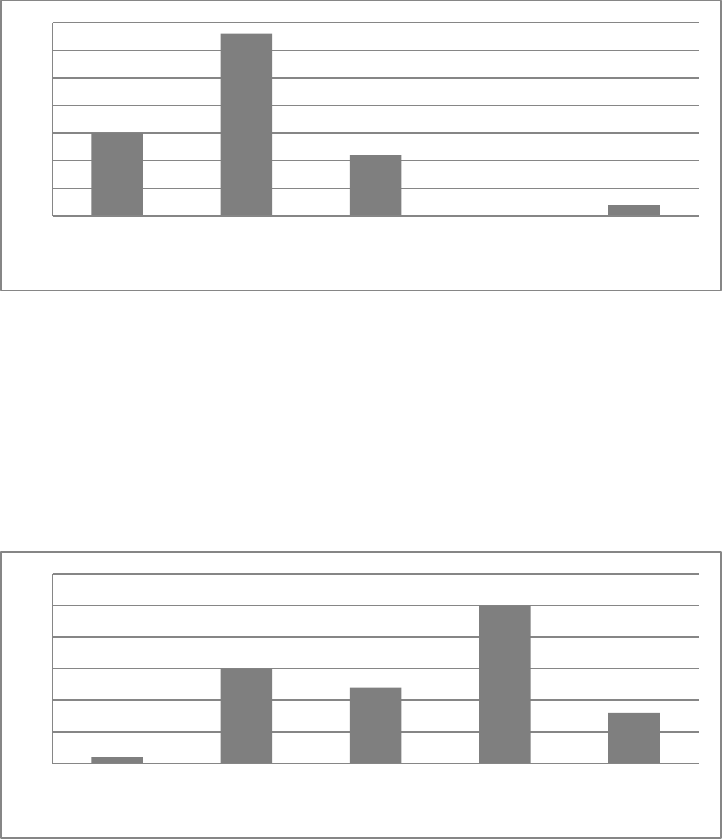
42
Figure 4.1.5 (b) Reason for attending postgraduate training was to improve the
management of children with a dual diagnosis of CP and visual impairment (n=61)
The third section gathered information on whether participants had attended courses because of
their affordability. Some participants (19.7%) felt neutral, and 25 (41.0%) disagreed that courses
are accessible because they are affordable. Only 15 participants (24.6%) agreed that courses
are affordable.
Figure 4.1.5 (c) Reason for attending postgraduate training was because of its
affordability (n=61)
The fourth section gathered information whether participants had attended courses because of
their regularity. More than half (54.19%) disagreed or strongly disagreed (18.03%) with this
rationale, although five participants (8.2%) agreed and two (3.28%) strongly agreed.
0
5
10
15
20
25
30
35
Strongly agree Agree Neutral Disagree Strongly
disagree
0
5
10
15
20
25
30
Strongly agree Agree Neutral Disagree Strongly
disagree

43
Figure 4.1.5 (d) Reason for attending postgraduate training was because of its regularity
(n=61)
The last section gathered data on whether participants had attended courses because they were
scientifically proven and evidence-based to improve therapeutic outcomes. Twenty-six
participants (42.6%) felt neutral about this statement, and 24 participants (39.3%) agreed.
Figure 4.1.5 (e) Reason for attending postgraduate training was because it was
scientifically proven and evidence-based to improve outcomes in therapy (n=61)
The figure below is a summary of the graphs above to show the reasons why participants
attended postgraduate training.
0
5
10
15
20
25
30
35
Strongly agree Agree Neutral Disagree Strongly
disagree
0
5
10
15
20
25
30
Strongly agree Agree Neutral Disagree Strongly
disagree
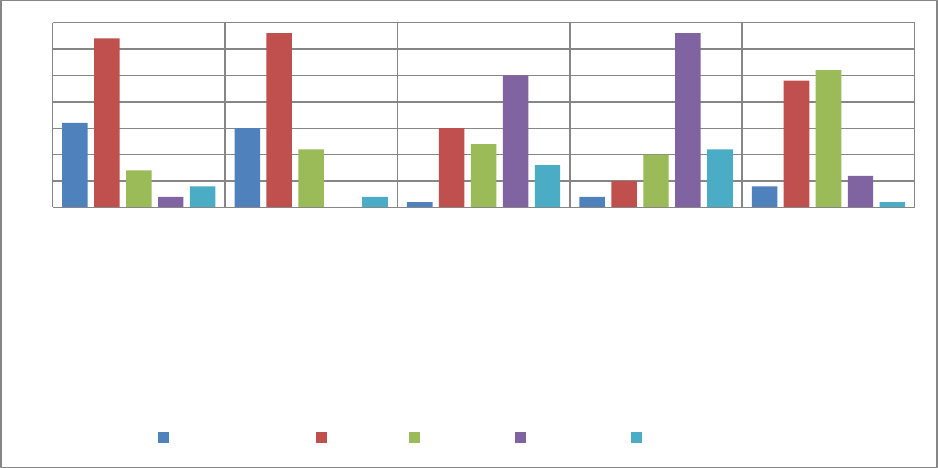
44
Figure 4.1.5 (f) A summary of the reasons for attending postgraduate training (n=61)
4.1.6 Participants’ cerebral palsy caseload
This section gathered information on the participants’ CP caseload. Participants were able to
indicate at both of these questions in groups of tens what percentages of their caseloads’ were
comprised of CP and what percentage had visual impairments. Then the information was grouped
together in the most logical way without making too many categories and in order to display the
trend of the caseloads.
Thirty-five participants (56.5%) reported to have a CP caseload of up to 30% and 18 participants
(29.0%) reported their CP caseload to be between 31% and 50%.
Of this CP caseload 20 participants (32.3%) reported that less than 10 % have visual impairments
and 14 participants (22.6%) reported that up to 20% of their CP caseload suffer from visual
impairments. Only 10 participants (16.1%) reported that more than 60% of their CP caseload have
visual impairments.
The most common visual impairment was low vision/poor visual acuity which was reported by 54
participants (87.1%). Strabismus, blindness and nystagmus were also common in the CP
population with the visual impairment with the lowest score (12.9%) being astigmatism.
0
5
10
15
20
25
30
35
Participants attended
courses to improve
their knowledge and
skill
Participants attended
courses to improve
their management of
children with CP and
visual impairment
Participants attend
courses as courses are
accessible due to its’
affordability
Participants attend
courses as it is
accessible because
courses are presented
regularly
Participants attend
courses as they are
proven to improve
outcomes in therapy
Strongly agree Agree Neutral Disagree Strongly disagree

45
Table 4.1.6 Incidence of visual impairment in participants’ CP caseload and the different
types (n=62)
Cerebral palsy caseload
Participants
(n=62)
Percentage (%)
Percentage of the participants’ caseload comprising CP children
0 – 30 %
35
56.5
31 – 50 %
18
29.0
51 – 70 %
4
6.5
71 – 100 %
5
8.1
Percentage of the participants’ CP caseload with some form of visual impairment
<10
20
32.3
10 – 20
14
22.6
20 – 30
4
6.5
30 – 40
5
8.1
40 – 50
4
6.5
50 – 60
5
8.1
>60
10
16.1
Types of visual impairments
from most seen to least seen
by participants in their
practices
Participants
Percentage seen
(%)
Low vision/poor visual acuity
54
87.1
Strabismus
40
64.5
Blindness
37
59.7
Nystagmus
35
56.5
Stereopsis
10
16.1
Astigmatism
8
12.9
4.2 Participants’ treatment regimes for children with cerebral palsy and visual
impairment
This section gathered information on whether the participants are aware when children with CP are
visually impaired, whether they make use of a multi-disciplinary team and if they change their
treatment once they become aware that a child with CP has a visual impairment.
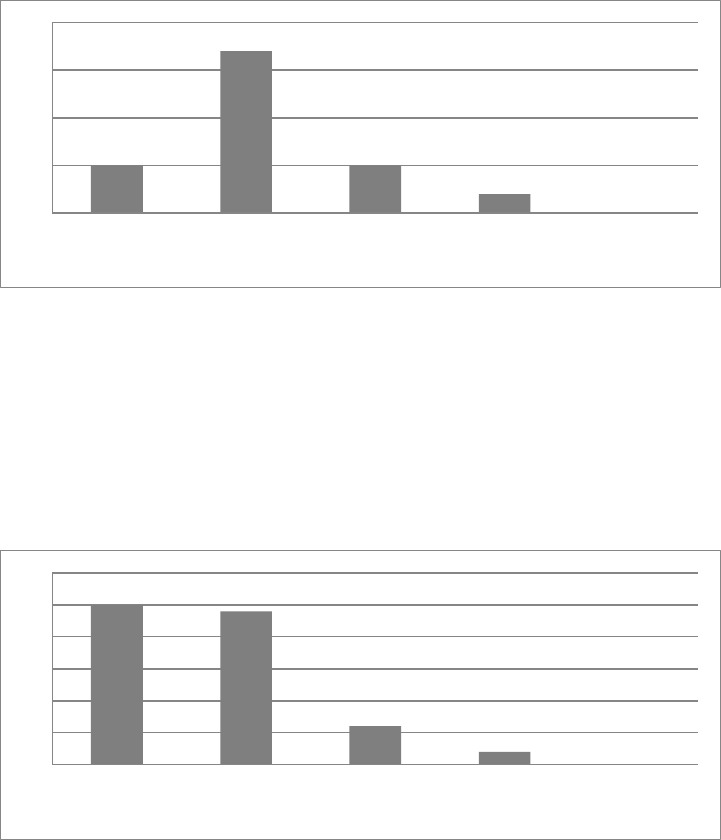
46
More than half (32) of the participants (57.1%) agreed and 10 participants (17.9%) strongly agreed
that they are aware when children with CP are visually impaired. Ten of the participants (17.9%)
felt neutral about this statement. Not one participant strongly disagreed with this statement.
Figure 4.2 (a) Participants’ response to recognising visual impairments in children with CP
(n=56)
Most of the participants (86%) reported that they use a multi-disciplinary team to manage children
with CP and visual impairments. Twenty-four participants (42.1%) agreed with this statement and
25 (43.9%) strongly agreed.
Figure 4.2 (b) Participants’ response to using a multi-disciplinary team when treating
children with CP and visual impairments (n=57)
Once participants become aware that a child with CP has a visual impairment, 29 (50.9%) agreed
and 18 (31.6%) strongly agreed that they would change their treatment approach. Only five
participants (8.8%) reported that they do not change their treatment approach once they become
aware that a child with CP has a visual impairment.
0
10
20
30
40
Strongly agree Agree Neutral Disagree Strongly
disagree
0
5
10
15
20
25
30
Strongly agree Agree Neutral Disagree Strongly
disagree
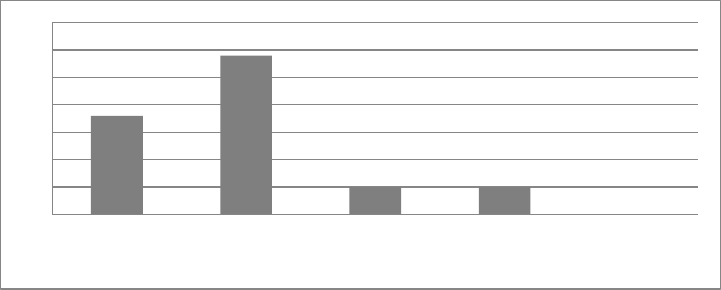
47
Figure 4.2 (c) Participants changed their treatment management when a child with CP has a
visual impairment (n=57)
4.3 Participants and different therapeutic interventions
4.3.1 Treatment interventions used by participants
This section gathered information on the different approaches the participants used. They were
asked to choose between the neurophysiological approach; neurodevelopmental therapy
approach; Rood Techniques; neurodevelopmental techniques (when qualified in NDT after
completing a Bobath course); somatosensory approach; sensory integration approach; sensory
integration approach (when qualified in sensory integration after completing the course to train
therapist in the specialised field of sensory integration) and the constraint-induced therapy
technique.
The most common treatment approach as indicated by 30 participants (53.6%), was the
neurodevelopmental therapy approach, with the second most common approach being the
somatosensory approach, with 29 participants (51.2%). The least common approaches used were
the sensory integration approach, which 22 participants (39.3%) reported never to use (when
qualified in sensory integration after completing the course) and the constraint-induced therapy
technique, which 20 participants (35.7%) reported never to use. It was interesting to note that 20
participants (35.7%) indicated that although they commonly use the principles of the sensory
integration approach, those with the sensory integration course qualification do not apply the
approach to children with a dual diagnosis of CP and visual impairment.
0
5
10
15
20
25
30
35
Strongly agree Agree Neutral Disagree Strongly
disagree

48
Figure 4.3.1 (a) Therapeutic interventions when managing children with CP and visual
impairment
The figure below represents the different therapeutic interventions from most popular to least
popular as reported by the participants. This was determined as follow: The participants were able
to indicate choices 1 – 5, 1 being never used and 5 being always used. Then to determine
popularity, the rating was calculated by Microsoft Excel to see which approach scored the highest
which indicated that this approach was most often used and thus the most popular. The rating
score refers to the popularity of an approach 1 being least popular and 5 being the most popular.”
0
5
10
15
20
25
30
35
Neurophysiological
frame of reference (n =
49)
Neurodevelopmental
frame of reference (n =
56)
Rood techniques (n =
47)
Neurodevelopmental
frame of reference
(Qualified in NDT) (n =
49)
Somatosensory
approach (using
children's sensory
systems) (n = 54)
Sensory Integration
Approach (n = 53)
Sensory Integration
Approach (Qualified in
SI) (n = 38)
Constraint-Induced
Therapy (n = 51)
Never Seldom Sometimes Very often Always

49
Figure 4.3.1 (b) Therapeutic approaches from most popular to least popular
4.3.2 Participants’ reasons for using the various approaches and treatments
This section gathered information about the participants’ reasons for using the different treatment
interventions. They were asked to justify their reasons for using a particular approach as illustrated
in figure 4.3.2, which also shows the reasons according to popularity of why the participants make
use of certain approaches and treatment modalities.
The participants were able to indicate all areas that were applicable to them. The most common
reason given for using a therapeutic intervention was because of work experience which 39
participants (69.6%) indicated for their use of the neurodevelopmental therapy approach. Thirty-six
participants (64.3%) gave the same reason for their use of the somatosensory approach, and 35
participants (62.5%) for their use of the principles of the sensory integration approach.
The second most common reason for using a particular therapeutic intervention was because of
evidence as indicated by 21 participants (37.5%) for both the neurodevelopmental therapy
approach and the neurodevelopmental technique (in which therapists’ had to receive further
training).
0.00
0.50
1.00
1.50
2.00
2.50
3.00
3.50
4.00
4.50
5.00
Neurodevelopmental frame of
reference
Somatosensory approach (using
children's sensory systems)
Sensory Integration Approach
Neurodevelopmental frame of
reference (Qualified in NDT)
Neurophysiological frame of
reference
Sensory Integration Approach
(Qualified in SI)
Rood techniques
Constraint-Induced Therapy
Rating score
Average rating
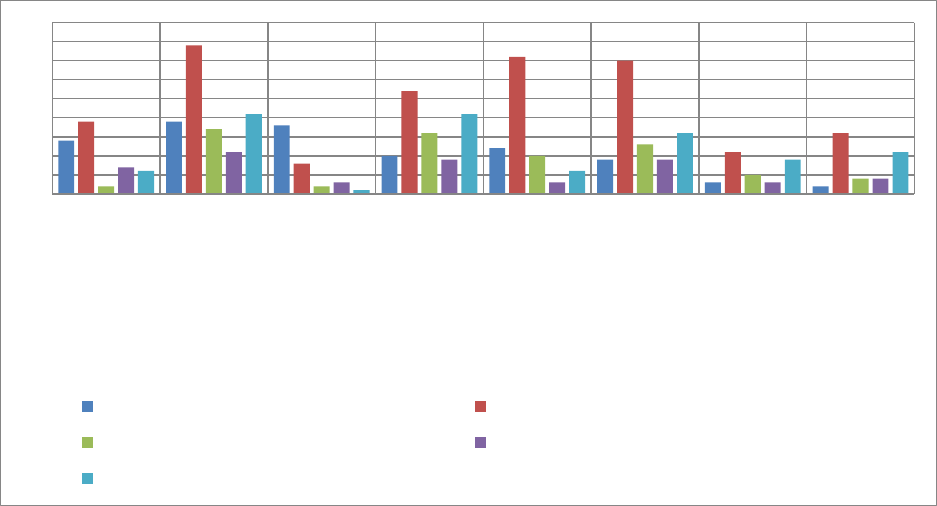
50
Figure 4.3.2 Participants’ reasons for using various approaches and treatments
The figure below displays the reasons, according to popularity, participants use various
approaches and treatments. The most common reason for using a particular approach or
treatment was because of work experience as reported by an average of 24 participants. The
least common reason for using an approach or treatment was because it is scientifically proven,
as reported by only an average of six participants.
0
5
10
15
20
25
30
35
40
45
Neurophysiological
frame of reference
(n = 37)
Neurodevelopmenta
l frame of reference
(n = 52)
Rood techniques (n
= 23)
Neurodevelopmenta
l frame of reference
(Qualified in NDT) (n
= 42)
Somatosensory
approach (using
children's sensory
systems) (n = 46)
Sensory Integration
Approach (n = 49)
Sensory Integration
Approach (Qualified
in SI) (n = 20)
Constraint-Induced
Therapy (n = 28)
Due to my undergraduate training experience Due to my work experience in the field
Because it is used at my workplace Because it is scientifically proven
Because it is evidence based
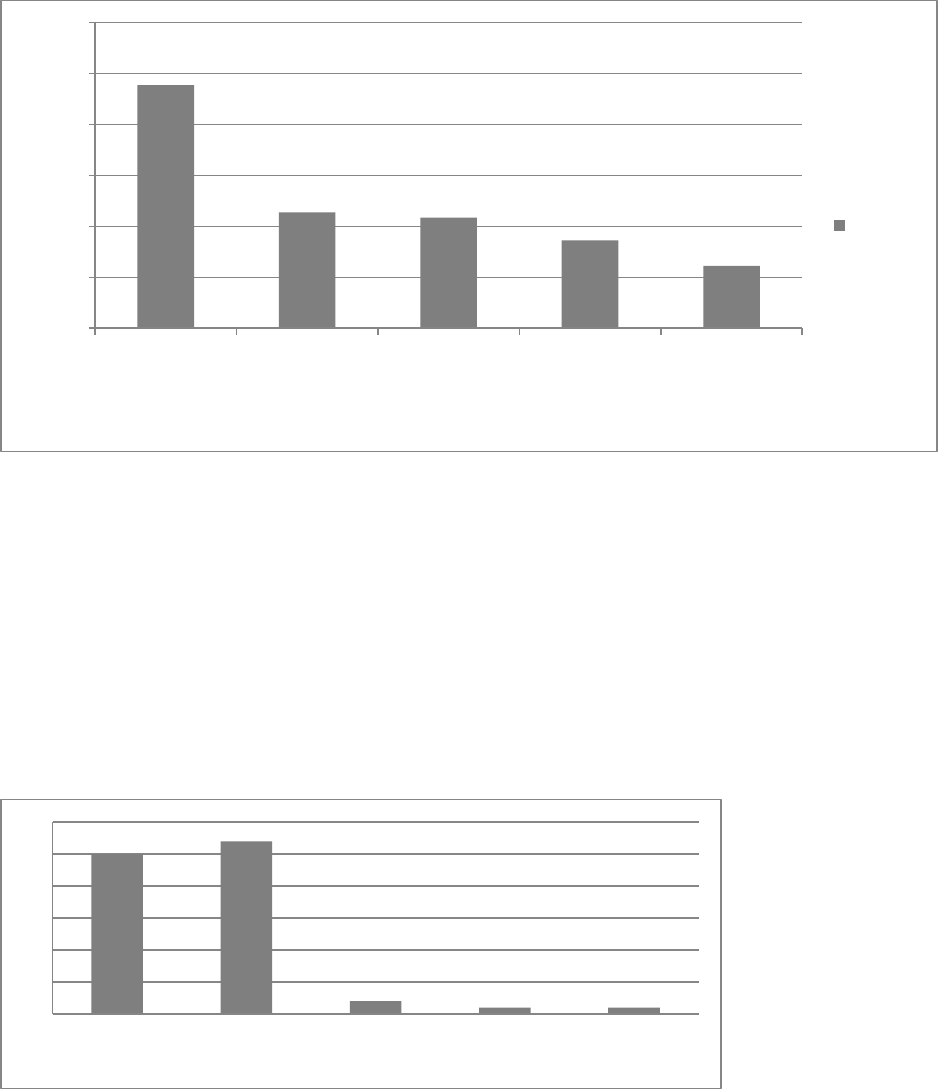
51
Figure 4.3.3 Reasons displayed as an average of participants’ use therapeutic approaches
or treatment interventions
4.3.3 Participant’s use of approaches and treatments in combination
This section gathered information on whether participants felt these approaches or treatment
interventions where best used in combination and the majority of participants (93%) felt they were.
Twenty-five participants (44.6%) strongly agreed and 27 (48.2%) agreed that approaches or
treatment interventions should be used in combination. Only two participants (3.6%) disagreed
with this statement.
Figure 4.3.3 Participants’ response to whether different approaches or treatment
interventions are best used in combination (n=56)
23.88
11.38
10.88
8.63
6.12
0
5
10
15
20
25
30
Due to my work
experience in the
field
Because it is
evidence based
Due to my
undergraduate
training
experience
Because it is
used at my
workplace
Because it is
scientifically
proven
Number of participants
Average
0
5
10
15
20
25
30
Strongly agree Agree Neutral Disagree Strongly
disagree

52
4.4 Participants’ responses on their confidence and attitude towards their
knowledge and training
4.4.1 Participants’ undergraduate training
This section gathered information on the participants’ view of the effectiveness of their
undergraduate training for managing children with CP. More than half of the participants disagreed
that their undergraduate training was adequate for managing children with CP. Twenty three
participants (41.1%) disagreed and seven (12.5%) strongly disagreed with the statement.
Figure 4.4.1 (a) Participants’ perceptions whether their undergraduate training was
adequate for managing children with CP (n=56)
The number of participants who disagreed with this statement increased significantly when asked
whether their undergraduate training was adequate for managing children with a dual diagnosis of
CP and visual impairment. The number of participants who disagreed remained 23 (41.1%), but 20
participants (35.7%) strongly disagreed with this statement.
0
5
10
15
20
25
Strongly agree Agree Neutral Disagree Strongly
disagree
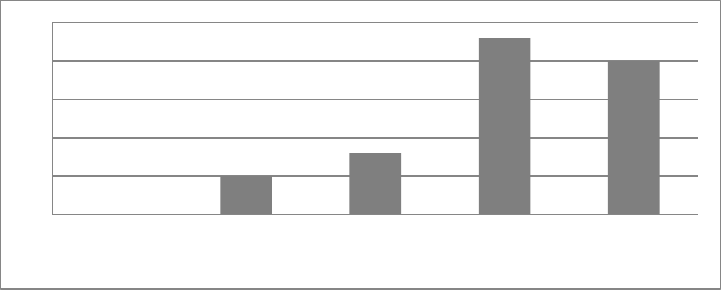
53
Figure 4.4.1 (b) Participants’ perception whether their undergraduate training was adequate
to manage children with a dual diagnosis of CP and visual impairment effectively (n=56)
4.5 Participants' confidence in their knowledge of and skill in the approaches and
treatments used for children diagnosed with CP and visual impairment, and their
view of the effectiveness of these treatments
This section gathered information on the participants’ knowledge of and skill in the use of the
various approaches and treatments. Participants regarded their knowledge about the approaches
and treatment modalities and their skill when applying this knowledge in treatment as good. There
was very little difference between how participants perceived their knowledge and skill.
The participants felt most confident in their knowledge of the approaches and treatment
interventions they used most often. The most common approach used was the
neurodevelopmental therapy approach, which 31 participants (67.4%) felt they knew well followed
closely by the somatosensory approach, which 27 participants (48.2%) felt comfortable with.
The participants said they rarely used the Rood techniques, which was the treatment intervention
most participants felt least confident with as reported by eight of them (17.4%). This was followed
by the sensory integration approach (when qualified in sensory integration), as reported by seven
participants (15.2%), and the constraint-induced therapy approach, as reported by five participants
(10.9%).
0
5
10
15
20
25
Strongly agree Agree Neutral Disagree Strongly
disagree

54
Figure 4.5.1 Participants’ confidence in their knowledge
As mentioned previously participants’ confidence levels were almost the same for their skill levels
as their knowledge. They felt most confident in the neurodevelopmental therapy approach as
reported by 31 participants (67.4%), followed by the somatosensory approach, as reported by 24
participants (52.1%) and the neurophysiological approach, as reported by 20 participants (43.5%).
The participants felt the least confident in using the Rood techniques, as with nine participants
(19.6%) admitting to having very poor knowledge of them.
0
5
10
15
20
25
30
35
Neurophysiological frame
of reference (n = 41)
Neurodevelopmental
frame of reference (n = 45)
Rood techniques (n = 35)
Neurodevelopmental
frame of reference
(Qualified in NDT) (n = 36)
Somatosensory approach
(using children's sensory
systems) (n = 43)
Sensory Integration
Approach (n = 43)
Sensory Integration
Approach (Qualified in SI)
(n = 23)
Constraint-Induced
Therapy (n = 35)
Very Good Good Barely Acceptible Poor Very Poor

55
Figure 4.5.2 Participants’ confidence of their skill
The figures 4.5.3 (a and b) on pages 56 and 57 illustrate how closely related the participants’
confidence in their skill in and knowledge of the approaches and treatment modalities were. The
researcher has divided this data into two graphs.
0
5
10
15
20
25
30
35
Neurophysiological
frame of reference
(n = 37)
Neurodevelopment
al frame of
reference (n = 45)
Rood techniques (n
= 34)
Neurodevelopment
al frame of
reference
(Qualified in NDT)…
Somatosensory
approach (using
children's sensory
systems) (n = 43)
Sensory Integration
Approach (n = 41)
Sensory Integration
Approach
(Qualified in SI) (n =
20)
Constraint-Induced
Therapy (n = 33)
Very Good Good Barely Acceptible Poor Very Poor

56
Figure 4.5.3 (a) Comparison between four therapeutic approaches and the participants’
knowledge and skill
0
5
10
15
20
25
30
35
Neurophysiological frame of
reference - Skill
Neurophysiological frame of
reference - Knowledge
Neurodevelopmental frame of
reference - Skill
Neurodevelopmental frame of
reference - Knowledge
Rood techniques - Skill
Rood techniques - Knowledge
Neurodevelopmental frame of
reference (Qualified in NDT) - Skill
Neurodevelopmental frame of
reference (Qualified in NDT) -
Knowledge
Axis Title
Very Good
Good
Barely Acceptible
Poor
Very Poor

57
Figure 4.5.3 (b) Comparison between the remaining four therapeutic approaches and the
participants’ knowledge and skill
This section gathered information on whether participants felt their treatment was effective and
whether they felt confident managing children with a dual diagnosis of CP and visual impairment.
Although most participants felt their treatment was effective, their confidence varied.
The majority of the participants (75.2%) considered their treatment when managing these children
to be effective while only eight participants (17.4%) disagreed. None of the participants strongly
disagreed with this statement.
0
5
10
15
20
25
30
Somatosensory approach (using
children's sensory systems) - Skill
Somatosensory approach (using
children's sensory systems) -
Knowledge
Sensory Integration Approach -
Skill
Sensory Integration Approach -
Knowledge
Sensory Integration Approach
(Qualified in SI) - Skill
Sensory Integration Approach
(Qualified in SI) - Knowledge
Constraint-Induced Therapy - Skill
Constraint-Induced Therapy -
Knowledge
Axis Title
Very Good
Good
Barely Acceptible
Poor
Very Poor
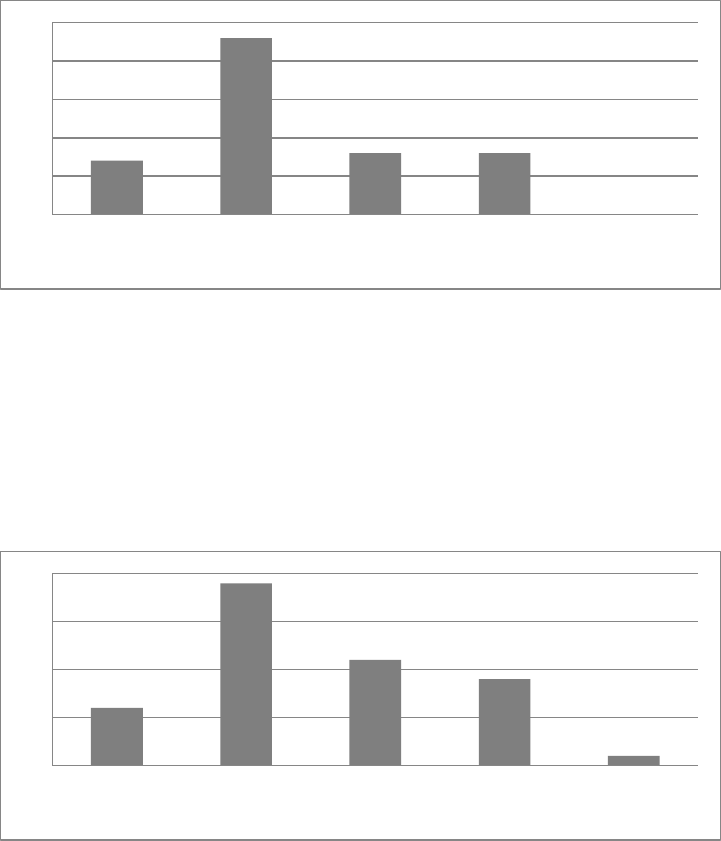
58
Figure 4.5.4 (a) Participants’ perceived effectiveness of their treatment to manage these
children (n=46)
Eleven participants (24.0%) felt neutral about their confidence in the effectiveness of their
treatment, whereas 19 (41.3%) felt confident about their treatment, nine (19.6%) did not feel
confident and one (2.2%) strongly disagreed about feeling confident in his/her treatment.
Figure 4.5.4 (b) Participants’ confidence in their treatment to manage these children (n=46)
4.6 Information gathered in an open-ended format regarding participants’ treatment,
training and opinions
This section gathered information on the participants’ treatment, including their short-term
outcomes, long-term outcomes and treatment principles. It also looked at how they viewed the
success of their treatment, and whether and how they change their treatment once a child with CP
is diagnosed with a visual impairment. Other aspects reported on included how they viewed the
level of training in South Africa and what they see as evidence-based and scientifically proven
treatment.
0
5
10
15
20
25
Strongly agree Agree Neutral Disagree Strongly
disagree
0
5
10
15
20
Strongly agree Agree Neutral Disagree Strongly
disagree
59
These questions were open-ended which allowed participants to write and formulate their answers
in any way they felt comfortable. The questions were then interpreted by looking at word
frequencies to group answers.
4.6.1 Summary of the most frequently reported outcomes regarding what the participants
saw as their three most functional short-term outcomes
(The graph below is not displaying the number of participants but rather representing how many
times an outcome was mentioned by the various participants.)
Sixteen participants (37.2%) reported that they focus on improving visual function such as
eye-hand coordination, visual tracking, object recognition, and maintaining gaze.
Sixteen participants (37.2%) reported that they focus on improving the execution of
occupational performance areas and independence including play, feeding, functional
mobility and social participation.
Fourteen participants (32.6%) reported that they make use of multi-sensory stimulation to
improve children’s interaction and participation in activities.
Thirteen participants (30.2%) reported that they aim to improve or stimulate normal motor
responses.
Eight participants (18.6%) reported that they focus on improving hand function, including
grasps and the manipulation of objects.
Seven participants (16.3%) reported that they focus on correct positioning.
Six participants (14%) reported that family training is one of the most important outcomes.
Four participants (9.3%) reported that they focus on improving postural and head control.
Four participants (9.3%) reported that they compensate use assistive devices to improve
children’s independence or care.
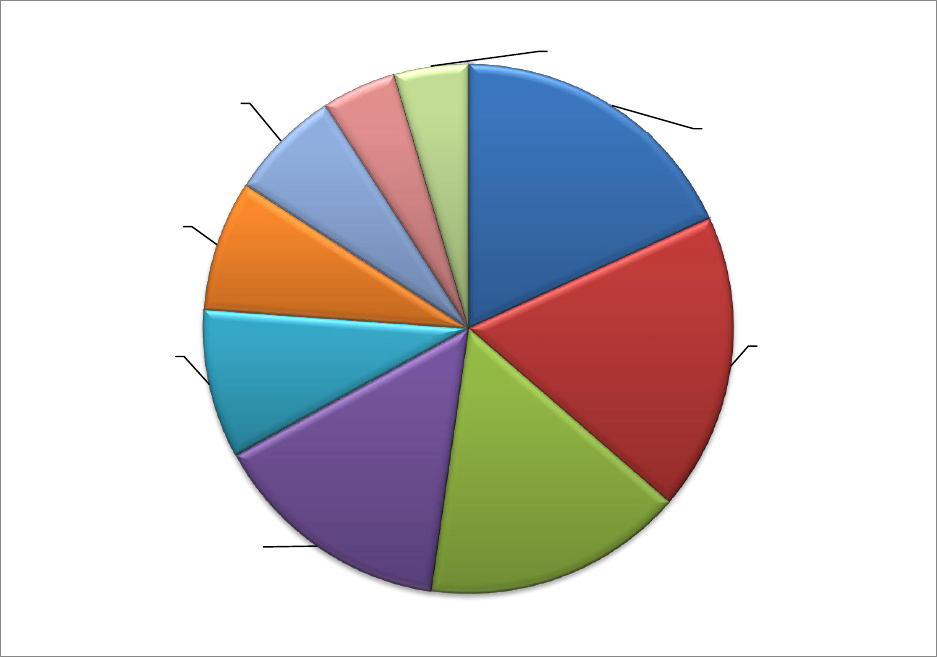
60
Figure 4.6.1 Summary of the participants’ most functional short-term outcomes (n=43)
4.6.2 Summary of the most frequently reported outcomes regarding what the participants
saw as their three most functional long-term outcomes:
Thirty-three participants (78.6%) reported that they would like these children to achieve
maximum independence in occupational performance areas such as play, self-care,
functional mobility, social participation, and community re-integration.
Eleven participants (26.2%) reported that they would like these children to be placed in a
special school.
Ten participants (23.9%) reported that family training and encouraging positive family
relationships is very important.
Eight participants (19.0%) reported that they would work on improving hand function, fine
motor skills, posture, and/or positioning.
Improving visual
function
16
Improvement of
OPA’s execution and
independence
16
Make use of multi-
sensory stimulation
to improve child’s
interaction and
participation in
activities
14
Improve or stimulate
normal motor
responses.
13
Improvement of
hand function
8
Focus on correct
positioning
7
Family training
6
Improving postural
control and head
control
4
Compensate and
make use of assistive
devices
4
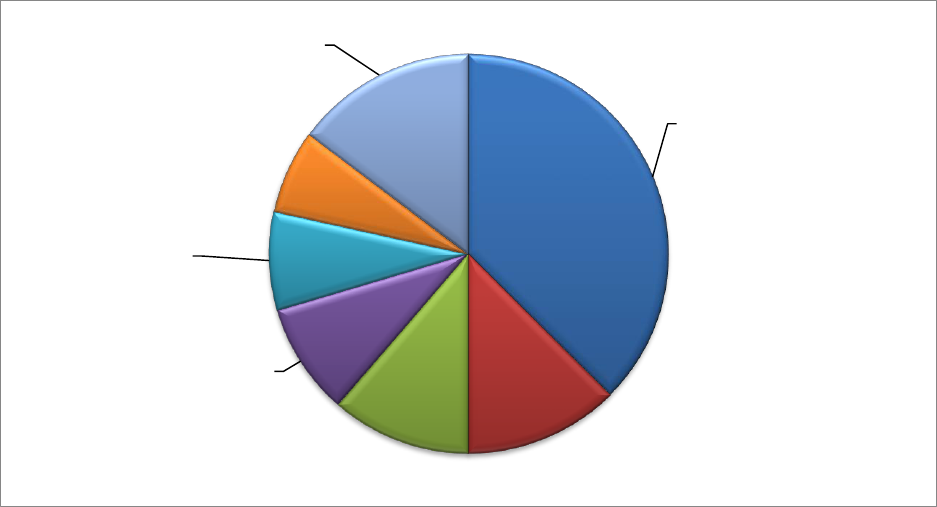
61
Seven participants (16.7%) reported that they would use assistive devices to compensate
for impairments. This includes training the family or child to use the device to achieve
maximum independence.
Six participants (14.3%) reported that improving communication would be very important
including making use of alternative and augmentative communication (AAC).
Other outcomes mentioned included improving quality of life, reaching maximum
independence, improving cognitive function, normalising tone, using a multi-disciplinary
team, improving interaction with the child’s immediate environment, and work placement.
Figure 4.6.2 Participants’ report on the most functional long-term outcomes (n=42)
4.6.3 Participants’ report on the most important principles used when treating these
children
The most common principles used comprised those in the family-centred approach and
somatosensory principles. Principles for the family-centred approach included family
training, education to manage the child and treatment interventions that take family goals
into consideration and ensure the family is involved in treatment. Principles for the
somatosensory approach included providing multi-sensory input, using other sensory
systems to compensate for lack of vision and stimulating one sensory modality at a time.
Fourteen participants (37.9%) reported they used the principles of both of these
Achieve maximum
independence in
OPA's
33
Special school
placement
11
Family Training
10
Improvement of
hand function; fine
motor skills; posture
and/or positioning
8
Use of assistive
devices and
compensate for
impairments
7
Improving
communication
including making use
of AAC
6
Other outcomes
13

62
approaches when treating these children. Out of the fourteen participants who reported that
they used the somatosensory approach two (5.4%) mentioned they would specifically
include sensory integration principles as well.
The most common principles for the neurodevelopmental therapy approach included
analysing movement, normalising tone, improving postural control to improve movement,
making use of repetition, observing and adapting according to neurological changes, and
ensuring a combination of principles to improve independence in occupational performance
areas. Thirteen participants (35.1%) supported the principles of this approach.
Eleven participants (29.8%) emphasised the need to accommodate, accurately assess and
manage and/or improve vision.
Nine participants (24.3%) supported a child-centred approach comprising principles such
as allowing the child to lead, using activities or objects that interest and motivates the child
during therapy and ensuring success.
Six participants (16.2%) supported the use of positioning principles such as use of assistive
devices to achieve optimal positioning.
Other principles mentioned included preventing further complications, ensuring child safety
and being aware of developmental stages during treatment.
Figure 4.6.3 Most common principles used during treatment (n=37)
Family-centred
approach and
somato-sensory
principles
14 each
NDT approach
13
Principles to manage
vision
11
A child-centred
approach
9
Use of assistive
devices
6
Other principles
63
4.6.4 Summary of the participants’ report on their perceived success in reaching their
outcomes and the reasons for success or failure:
Twenty-three participants (62.2%) reported they experienced success in reaching their
outcomes, five (13.6%) reported they did not experience success and nine (24.3%)
reported they experienced success occasionally.
Fifteen participants (40.5%) reported family compliance as the most important key to
reaching outcomes. The participants felt children whose families were compliant and
ensured ongoing therapy at home were more successful than children from families who
did not participate in and continue with therapy at home.
Other factors that were reported to influence success in outcomes included:
intensity of training which includes increasing the time and frequency of training
resulted in higher levels of success, as reported by six participants (16.2%);
realistic goal setting as reported by three participants (8.1%);
co-morbidities such as low cognition and poor sensory integration as reported by 2
participants (5.4%) result in lower success rates;
limited training and knowledge as reported by one participant (2.7%) lead to lower
success rates; and
the use of multi-disciplinary teams; well-developed ongoing assessment tools and
AAC as reported by three different participants (8.1%) to lead to higher success
rates.
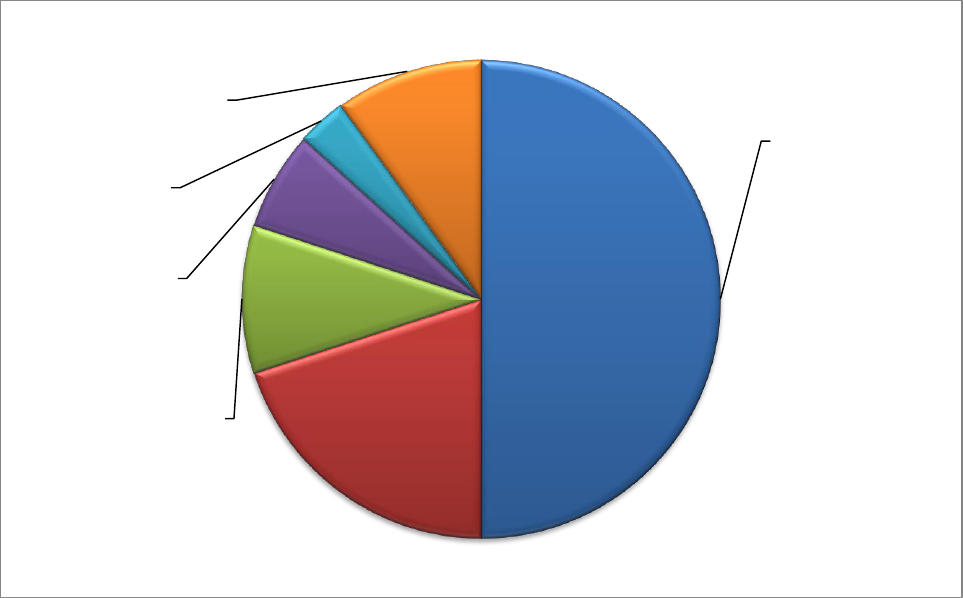
64
Figure 4.6.4 Participants’ perceived success in reaching their outcomes (n=37)
4.6.5 Summary of the participants’ report on how they change their treatment interventions
when children have a dual diagnosis of CP and visual impairment
Eleven participants (28.9%) used a multi-sensory approach as opposed to a pure motor
approach when children are diagnosed with a dual diagnosis of CP and visual impairment.
Six participants (15.8%) reported that it was important to adopt a sensory approach with a
focus on visual training when treating children with a dual diagnosis of CP and visual
impairment.
The participants were divided over their preferred approach with some opting for the
sensory approach including sensory integration, and others for the neuro-developmental
approach including neurodevelopmental therapy techniques. Three participants (7.9%)
reported they preferred to use a sensory approach as oppose to an NDT approach when
children have a dual diagnosis, whereas two participants (5.3%) reported the opposite, and
two others (5.3%) reported they preferred to combine these two approaches.
Other changes (23.7%) mentioned once or twice included the importance of having a multi-
disciplinary team, using verbal and manual guidance during treatment, compensating and
Family compliance
15
Intensity of training
ie. increase in time
and repetition
6
Realistic goal setting
3
No co-morbidities
2
Lack of training
1
Use a multi-
disciplinary team;
well-developed
ongoing assessment
tools and AAC
3

65
making adjustments to the environment to ensure active participation from the child, and
increasing the use of caregivers during treatment.
Figure 4.6.5 Participants’ change in treatment interventions to accommodate children with a
dual diagnosis of CP and visual impairment (n=38)
4.6.6 Summary of the participants’ report on the sufficiency of training in South Africa
Twelve participants (29.3%) regarded undergraduate training as insufficient, with reasons
varying from inexperienced lecturers, limited time during undergraduate training to focus on
a speciality such as children with diagnosis of CP and visual impairment and limited time to
practice knowledge gained.
According to 26 participants (63.4%) the training in South Africa is not sufficient and the
reasons for this are multiple. Some participants reported that although there are quality
courses available specifically from SANDTA, this is not enough. Reasons included:
courses being unaffordable or difficult to access because they are not presented in
other provinces other than Gauteng province or not regularly presented in all other
provinces;
participation in courses requiring significant time off work;
· A multi-
sensory approach
as opposed to a
pure motor
approach
11
Greater focus on a
sensory approach
6
Use sensory
approach rather
than NDT
3
Use NDT rather
than sensory
approach
2
Combining NDT
and SI
2
Other changes
9

66
limited focus being given to combine these two diagnoses’ or that more time is
spent on treating primary diagnosis of CP and little time is spent on the visual
impairment; and
lack of courses that focus on a combination of treatments for children with CP and
visual impairment.
Five participants (12.2%) reported that because they had received insufficient training, they
felt they lacked the experience and knowledge to manage these children. This led to either
not treating these children or lacking confidence when managing them.
Five participants (12.2%) referred to Christa Scholtz as an expert on children with a dual
diagnosis of CP and visual impairment whose efforts through training have been valuable in
addressing the lack in this area in South Africa.
Figure 4.6.6 Report on the sufficiency of training in South Africa (n=41)
Undergraduate
training was
insufficient
12
General training in
South Africa is
insufficient
26
Insufficient training
leads to lack of
knowledge and
confidence
5
Christa Scholtz’s
presents quality
training
5
67
4.6.7 Summary of participants’ report whether their treatment should be scientifically
proven and evidence-based and their understanding of these terms (n=40)
Participants noted evidence-based practice as most relevant and up-to-date treatment as it
is supported by research. Treatment and techniques emanating from it have been proved
to be effective by data that was objectively measured, and include case studies performed
and data captured from them. As the efficacy of this treatment can be measured it is
considered the best practice to follow as it leads to increased confidence levels and
improved management of children with a dual diagnosis of CP and visual impairment.
Participants described scientific proof as carrying out research to prove a hypothesis to be
either correct or incorrect through empirical testing. It results in statistics to support or to
reject a certain treatment or technique. Participants reported that case studies are more
freely available for them to refer to than scientific data.
Even though the question stated that participants should report on their understanding of
these terms only 23 (57.5%) of the participants gave an explanation of their understanding.
Of the 23 (57.5%) participants only 13 (32.5%) of the participants seemed to have a good
understanding of the term as compared to the definitions discussed in chapter 2 section
2.6. The other ten (25%) participants only mentioned aspects of what evidence based
practice or scientifically proven data means.
Even though all participants stated that occupational therapists should follow only treatment
that are scientifically proven and evidence-based, nine (22.5%) felt that treatment does not
always adhere to these terms especially when treating children with a dual diagnosis of CP
and visual impairment. These nine participants (22.5%) felt more research should be
conducted.
4.7 Conclusion and summary of the main results
There were 62 participants, which one of whom was male. Universities across South Africa were
represented, the top two being the University of Cape Town and the University of the Free State.
The majority of the participants (58.0%) had graduated in the past ten years. Of all the participants
20.9% had 23 or more years’ experience working with children with CP. Just more than half of the
participants (54.8%) work in the public sector.
More than half of the participants (56.5%) reported to have a caseload of up to 50 % of children
diagnosed with CP. Of the participants’ CP caseload, 16.1% reported that 60% or more of their CP
68
children have a visual impairment. The most common visual impairment was low vision as reported
by 87.1% of the participants.
The majority of the participants (74.2%) reported they had attended further training in the
management of children with CP and visual impairment. The most common course reported was
the eight-week neurodevelopmental therapy technique workshop held by SANDTA.
Just more than half (52.5%) of the participants agreed that they attended courses to improve their
knowledge and skill, with 54.1% citing that courses and training improved their management of
children with CP. Only 24.6% felt courses were affordable and only 8.2% felt that courses were
presented regularly. Less than half (39.3%) reported that they attend courses as it is scientifically
proven and evidence-based to improve outcomes of therapy.
The majority of participants (75%) agreed or strongly agreed that they were able to tell when a
child with CP had a visual impairment. Once the participants become aware a child is visually
impaired 89.5% participants reported to change their treatment and 86% reported that they always
make use of a multi-disciplinary team to manage these children.
The most common approach used for the management of children with CP and visual impairment
was the neurodevelopmental therapy approach (53.6%) followed closely by the somatosensory
approach (51.2%). The least popular approach was the sensory integration approach (after
completion of the sensory integration courses) which 39.3% of the participants reported never to
use. The majority of the participants (92.9%) reported that approaches or treatment interventions
are best used in combination.
Work experience was cited as the main reason for using a particular treatment approach, as 69.6%
of participants reported for the neurodevelopmental approach and 64.3% for the somatosensory
approach. The second most common reason as reported by 37.5% of participants was that the
neurodevelopmental approach is evidence-based.
More than half of the participants (53.6%) reported that their undergraduate training was
insufficient to educate them how to manage children with CP, and this increased to 76.8% when
having to manage children with CP and a visual impairment.
Many of the participants felt assured about their knowledge of the approaches and treatment
interventions they use, as 67.4% reported to have good knowledge of the neurodevelopmental
69
therapy approach and 48.3% of the somatosensory approach. Knowledge on the Rood techniques
received the lowest rating as reported by 17.4%.
Similar to the perception of their knowledge, the participants reported to feel good about their skill,
as 67.4% felt assured about their skill regarding the neurodevelopmental therapy approach and
52.5% for the somatosensory approach. Again similar to their perception of their knowledge 19.5%
of the participants felt they were poorly skilled regarding the Rood techniques.
The majority of the participants (75.2%) saw their treatment as effective although only 41.3% felt
confident in their management of children with CP and visual impairment.
The two most common short-term outcomes, according to 37.2% of the participants, were
improving visual function, including focus on eye-hand coordination, and improving independence
in occupational performance areas. Improving the child’s interaction through the use of multi-
sensory stimulation was reported by 32.6% of the participants. The most common long-term
outcomes were improving and reaching maximum independence in occupational performance
areas, as reported by 78.6% of the participants, and placing these children in special schooling
systems, as reported by 26.2%.
The most common therapeutic principles followed by participants were those of the family-centred
approach and the somatosensory approach, as reported by 37.9% of participants, followed closely
by the principles of the Neurodevelopmental therapy approach, as reported by 35.1% of the
participants.
Almost two-thirds of the participants (62.2%) perceived to reach their outcomes successfully and
15 participants (40.5%) felt that family compliance is the most important factor contributing to
reaching successful outcomes.
Participants reported to change their treatment intervention when a child with CP has a visual
impairment. Once the participants discover a visual impairment, 28.4% of them make use of a
multi-sensory approach rather than a pure motor approach and 15.8% participants make use of a
sensory approach with special focus on visual stimulation.
Undergraduate training in South Africa was thought to be insufficient by 29.3% of the participants,
and general training for the management of children with CP and visual impairment was
considered insufficient by 63.4%. Reasons included from courses being inaccessible, time
consuming and unaffordable.

70
All the participants supported that therapy should be evidence-based and scientifically proven but,
22.5% reported that the current treatment for children with a dual diagnosis of CP and visual
impairment does not always adhere to those terms.

71
Chapter 5: Discussion of results
5.1 Introduction
This chapter will focus on the interpretation of the data and reflect on the significance of the results
of the study. It will reflect on the objectives of the study and investigate any limitations the study
might have had. Lastly, it will compare results of the results of the study with other studies and
literature.
5.2 Response rate to the survey
The survey was completed by 62 occupational therapists, and had a response rate of 3.4% as the
questionnaire was sent to a population of 1820 occupational therapists. The various professional
bodies – including Occupational Therapy Association for South Africa (OTASA); South African
Neurodevelopmental Association (SANDTA) and Eastern Cape Occupational Therapy Forum sent
out the emails but were not able to identify the occupational therapists’ field of practice so it was
impossible to email only occupational therapists who treated children with cerebral palsy (CP). It
was therefore not possible to determine how many of the occupational therapists who received the
survey met the inclusion criteria, and thus a sample size could not be calculated. The
questionnaire was available for completion for a period of four months, and emails were sent to
remind prospective participants to complete the survey. This still resulted in a small sample which
influenced the results as this study aimed to describe occupational therapy interventions for
children with a dual diagnosis of CP and visual impairment in South Africa. The small number of
participants cannot be representative of all occupational therapists in South Africa treating children
with a dual diagnosis of CP and visual impairment even though, as previously discussed, the
researcher was not able to determine the exact population size. Extensive steps were taken to
gather as many participants as possible so the information generated from this study can be used
as a foundation for occupational therapy intervention for children with a dual diagnosis of CP and
visual impairment.
According to international research, the average response rate for email surveys is 24.8%
(63)
.
Although there were no statistics available on survey response rates for South Africa, the
extremely low response rate raises a number of concerns. The topic for this study was very
specific and only those who adhered to the inclusion criteria were asked to participate, but the
72
email requesting participation was sent to a general population which could have impacted the
response rate. Secondly the researcher was not able to identify the number of participants who
wanted to complete the survey but did not meet the inclusion criteria. When taking this into
consideration, the response rate still remains low and should be considered as a limitation to the
study. As this is such a specialised field, the information gathered can still be seen as sufficient to
provide at least a background to occupational therapy practice in South Africa for children with CP
and visual impairment.
5.3 Demographic characteristics of the participants
Only one male participated in the study. If you look at the gender statistics for occupational
therapists, as supplied by the Health Profession Council of South Africa, there are currently 4557
occupational therapists registered in South Africa of which only 222 are male, making male
therapists representative of less than 5 % of the occupational therapy population in South Africa.
This implies that the one male who participated can be representative of the occupational therapy
population in South Africa. It is also unclear why so few males participated in the study and
literature does not provide any clarity on this.
Undergraduate training from the majority of universities in South Africa was well represented in the
study. The majority of participants came from the University of Cape Town and the University of
the Free State. Even though the participants were trained differently at their respective universities,
institutions across South Africa were represented, so data obtained through this study could be
generalised to undergraduate training in South Africa. This is significant as universities differ
according to the time and credits devoted to a specific field
(28)
. Although the knowledge therapists
gained during their undergraduate training might vary, the study gathered and integrated
information from different South African universities.
The average experience of the participants working in the field of occupational therapy was almost
equally distributed between those with ten years’ experience or less, and ten years’ experience or
more. This indicated that about half of the participants (42.0%) showed extensive work experience
in the field. Considering the definition of clinical expertise, which forms part of evidence-based
practice and encompasses work experience
(54)
, the fact that half of the participants had extensive
work experience indicates that those participants are able to make effective clinical decisions.
Their clinical reasoning can therefore add significant value to the information obtained in this study,
which aimed to determine which interventions occupational therapists use to treat children with a
dual diagnosis of CP and visual impairment, as these participants are more likely to make better
73
decisions based on their clinical expertise. Although it is also important to note that more than half
of the participants had ten years’ experience or less (58.0%) which could have negatively impacted
the results of this study when clinical expertise is taken into consideration. However work
experience is not the only aspect that adds value to clinical expertise as it also regards aspects
such as education and clinical training which are not related to work experience. This would mean
that even though these participants had limited years of work experience their knowledge and skill
would still be valuable in the results of the study.
More than half of the participants (54.8%) represented the public health setting. However
participants came from a variety of settings including hospitals both private and public, schools and
private practice. All of which was well represented in this study. This allowed the study to gain
information from occupational therapists in various areas of work.
No participants had postgraduate degrees, however 46 (72.2%) had completed postgraduate
courses. The neurodevelopmental course hosted by SANDTA was a very popular choice for
participants working in the field of CP. This could imply that participants felt that completing
courses as opposed to postgraduate degrees is sufficient when managing children with CP. Other
reasons could be that completing courses is cheaper and less time consuming than postgraduate
degrees or that courses are geared toward clinical application and skills and not only knowledge.
This aligns well with clinical expertise as it is described as a combination of education; work
experience and clinical training and thus integrates the knowledge with clinical training and
application
(54)
. That the participants completed courses is in line with evidence-based practice and
clinical expertise stating that practitioners should aim to obtain knowledge and skill geared to
improve their practice, which they are likely to obtain through postgraduate courses
(54)
. This is
further emphasised by participants indicating that they felt these courses improved their
knowledge, skill, and management of children with CP and visual impairment. Participants also
indicated that they were aware these courses aimed to improve outcomes in therapy and that they
would keep their clinical expertise current, which strongly aligns with evidence-based practice
(54)
.
But participants also strongly felt courses were costly and not presented regularly enough. This
could be why 16 (25.8%) of the participants had not undergone further training in the form of
postgraduate courses or why only 22 (35.5%) of the participants have managed to complete a
course specifically aimed at assisting with the management of more complicated CP children as
opposed to only introductory courses. The concern is that, according to literature describing
evidence-based practice, it is very important to attend courses and keep up to date with new
74
occupational therapy research, and if this is not done, practitioners can no longer depend on their
own clinical expertise to make the best-evidence based decisions in their practice
(54)
.
Participants particularly complained about the accessibility of courses. They considered courses to
be time consuming and complained that they are not presented across South Africa, so
participants from remote areas find it difficult to access these courses. This resulted in participants
not receiving further specialised training while working in a speciality field which can significantly
influence clinical expertise when managing clients
(54)
.
The participants CP caseload was mostly up to 50 %, with 35 participants (56.5%) having a CP
caseload of up to 30% and 18 participants (29.0%) having a CP caseload of between 31% – 50 %.
The high number of CP clients in their caseload was to be expected as this study aimed to reach
participants who regularly manage children with CP. The World Health Organisation also reported
that 10% of children with disabilities in South Africa present with disability that is of neurogenic
origin
(2)
, so children with CP are to be expected.
More than half of the participants reported that 30 % or less of their CP caseload has visual
impairment, and only 10 (16.1%) reported that more than 60% of their CP caseload has some form
of visual impairment. This contradicts a study done by Fazzi, Signorini, La Piana, Bertone,
Misefari, Galli, Balottin & Bianchi (2012), who investigated the visual dysfunctions in children with
CP and reported that about 60% of children with CP have some form of visual impairment
(10)
. A
reason for the discrepancy in numbers between what the participants reported and what Fazzi et
al. (2012) suggest can be explained through a study done in Kenya by Njambi, Kariuki & Masinde
(2009)
(10)(11)
. Njambe et al. (2009) investigated visual dysfunctions in children with CP and stated
that professionals struggle to consistently identify visual impairments in children with CP because
of multi-system involvement
(11)
. This implies that a reason for the lower rates of visual impairment
in the participants’ CP caseload could be that they under-diagnose the visual impairments in these
children. This could imply that participants are not adjusting their treatment when children with CP
have a visual impairment as they are unaware of the visual impairment. This would mean that
these children are not being treated according to the correct treatment regimes as prescribed by
the relevant literature
(14)(4)(43)
.
The different types of visual impairments seen by the participants were consistent with visual
impairments seen in children with CP according to the study by Fazzi et al. (2012)
(10)
.
75
5.4 Treatment interventions
5.4.1 Occupational therapists’ approach to their treatment regimes
The majority of the participants (75.1%) reported becoming aware when a child with CP has a
visual impairment. It would appear that participants are confident in diagnosing visual impairment
in children with CP. This could positively indicate that the majority of the children are treated
correctly, and can also be linked to the previous discussion of participants’ CP caseload. What is
interesting to note is that if the majority of participants are aware when a child with CP has a visual
impairment, that more than half of them reported that only 30% or less of their CP caseload is
visually impaired. A possible reason could be that even though participants think they are aware of
visual impairments in CP children, they are still under diagnosing these impairments because of
the difficulties in diagnosing them, according to the study by Njambe et al. (2009)
(11)
. Another
explanation could be that the prevalence of visual impairment in the participant’s CP caseload
could be lower than the literature suggests or participants could be working with higher-functioning
CP children who do not have visual impairments.
Most of the participants (86%) reported using a multi-disciplinary team to manage children with CP
and visual impairments. This is consistent with literature which states that a multi-disciplinary team
is needed during the treatment
(11)(20)
. The Australian health department stated that therapists who
use multi-disciplinary teams would ensure the client is treated holistically, ensuring higher success
rates in treatment
(39)
. This can link to why participants also reported that they perceived their
treatment as successful. The studies by Njambe et al. (2009) and Jeglinsky, Autti-Rämö & Brogren
Carlberg (2010) suggest the lack of a multi-disciplinary team could be a reason for therapists not
being able to identify visual impairments or feeling confident during treatment
(11)(20)
. These two
aspects were observed in this study. It appears that even though participants used multi-
disciplinary teams, they were still not aware of visual impairments and reported a lack of
confidence in their treatment.
The majority of the participants indicated that children with a dual diagnosis of CP and visual
impairment require a multi-disciplinary team. This is very positive as literature suggests that using
a multi-disciplinary team ensures that outcomes are reached
(20)(11)
. What was disappointing,
however is that even though participants indicated that these children require a multi-disciplinary
team approach very few indicated the need for a multi-disciplinary team as part of their principles
during treatment or, as an essential component to ensure outcomes are reached.
76
The majority of the participants felt treatment regimes need to be adapted once they discover a
child with CP has a visual impairment. This aligns well with literature stating that therapy for a child
with CP and a visual impairment cannot be the same as for a child with CP
(4)(14)
.
5.4.2 Occupational interventions used by therapists to guide their treatment for children
diagnosed with CP and visual impairment
The most popular treatment intervention, as indicated by 30 participants (53.4%), was the
neurodevelopmental therapy approach. The use of this approach is in line with literature such as
the study by Butler and Darrah (2001) who investigated its effectiveness and indicated various
studies that proved that this treatment can be effective when managing children with a dual
diagnosis of CP and visual impairment
(16)(38)
. This approach is commonly taught at undergraduate
level, but not in depth. A preference for this approach is also in line with the most popular choice of
postgraduate courses attended the eight-week SANDTA course, as described earlier. This could
also explain why the neurodevelopmental therapy approach was the most popular treatment
intervention used by participants as they were qualified to use it. However, this approach is not
always described as successful to treat these children as literature suggests that sometimes other
approaches show better success, or that there is often no difference achieved through the use of
this approach as opposed to other approaches
(51)(16)(38)
. These other approaches include those that
has been thoroughly discussed in chapter 2 however literature does not show specific
combinations of approaches rather it suggests that therapists should be able to evaluate which
combination works best for a specific client. This can be only happen successfully if therapists
show good clinical expertise and knowledge of best practice
(55)
. Additionally, a study by Owen,
Adams & Franzsen (2014) that investigated practice models used in South Africa found that
preference for a particular model used depend on, among other things, the models used by others
in the clinician’s work environment
(64)
. This could be another reason this approach was preferred
by the participants who also agreed they make use of certain treatment interventions because they
are used at their workplace.
The somatosensory approach was the second most popular approach as indicated by 29
participants (51.2%). According to literature by O’Brian (2015) and Pavão, Dos Santos Silva,
Savelsbergh & Ferreira Rocha (2014) the somatosensory approach can be a useful approach,
although it should be used with caution and in combination with other treatment interventions such
as the neurodevelopmental therapy approach, among others
(32)(36)(43)
. Reasons being that
outcomes through the use of this approach, are still mixed when managing children with CP and
visual impairment
(13)(44)
. Other reasons include the multi-system involvement in the brain which
77
leads to impaired sensory processing. This can in turn lead to sensory stimulation being
misinterpreted, slower processing and thus therapists can easily over-stimulate the child as the
child takes longer to respond and thus approach should be used with caution
(36) (43)
. The fact that
literature and studies suggests that treatment interventions should be used in combination aligns
positively with this study as 93% of the participants agreed that treatment interventions are best
used in combination. Literature reviewed, such as O’Brian (2015) and other studies, stated that
combining treatment interventions was to ensure the best outcomes for these children
(36)
.
Although the participants commonly used the principles of the sensory integration approach once
they were qualified in sensory integration 22 participants (39.3%) reported they never use this
approach in the management of children with CP and visual impairment. This contradicts relevant
literature, as although the results are still inconsistent, the sensory integration approach has shown
success in managing children with CP and visual impairment
(32)(47)(50)
. Participants should not only
be using the principles which are aspects or guidelines of the approach, but the entire approach
(as defined on p.14), according to Berry and Ryan (2002) who investigated various approaches in
the management of children with CP and visual impairment
(32)(47)(51)
.
Most of the participants reported to feel neutral towards the use of the neurophysiological
approach. Participants reported having limited knowledge of this approach which could be a
reason they are not using it. Another reason for not using the approach could be explained through
a study by Owen et al. (2014) who stated, clinicians use models that are known to their
environment and used by their colleagues, and the neurophysiological approach was used least at
their work places
(64)
. Kielhofner (1997) and O’Brian (2015) studied motor control, and indicated that
this approach can be helpful in managing these children as it addresses visual functioning as well
as the motor control during functional activity
(36)(46)
. However Kielhofner (1997) states these results
are inconsistent, and by comparing this study to other ones, it is evident that the relevant literature
is still limited and does not specifically address children with a dual diagnosis of CP and visual
impairment
(46)(41)
.
The constraint-induced approach was the second least common approach as reported by 20
participants (35.7%). Literature reviewing the technique developed by Taub suggests constraint-
induced therapy can be used adjunct to therapy approaches
(36)(51)
, although it requires some visual
control and thus would not be consistently effective during treatment, particularly if the child is
severely affected
(41)
. This could be why participants do not use this approach when managing their

78
clients. They also reported to feel less confident in their knowledge of and skill in this approach,
which might imply that they don’t know it can be helpful.
Rood techniques were also reported to be uncommon in treatment of children with a dual
diagnosis of CP and visual impairment as 15 participants (26.8%) reported never to use this
technique. Participants indicated that they mainly use it due to their undergraduate experience.
The reason for this was that they felt least confident in this technique as reported by eight
participants (17.4%) and nine participants (19.6%) indicated to have very poor knowledge of this
technique. This is contradictory to literature as reviewed by O'Brian & Williams (2010) as well as
literature by Schultz-Krohn, Royeen, Mccormack, Pope-Davis & Jourdan (2010) who suggested
this technique can be valuable as an adjunct to therapy
(41)(34)
.
All participants strongly felt that approaches are always best used in combination. It is important
that they agree with this statement to ensure the optimal management of children with CP and
visual impairment, and is in line with literature describing therapeutic interventions for motor control
(36)
. As discussed in the literature review, the majority of the approaches that can be useful in the
management of children with CP and visual impairment do not produce consistently successful
results, which suggests that approaches should be used in combination
(41)(32)(16)
. The literature
does not necessarily suggest which approaches should be combined, but that the therapist should
be able to apply combinations of different therapeutic interventions that best suit the client.
5.4.3 Reasons participants reported for using certain approaches when managing children
with CP and visual impairment
The most common reason for using a particular treatment intervention was because of their work
experience. As 50% of the participants had been working for five years or more, it is significant that
this was the most common reason as it implies that participants value the experience they gain
from work and what they have seen results in, and use this to guide their treatment choices. This
suggests that clinical expertise, which includes work experience, is used as the principle reason to
follow a particular treatment intervention
(54)
. According to Bennet et al. (2000) this is valuable as
clinical expertise are supposed to support evidence-based practice
(55)
. Another reason for this
being the most common reason for using a particular treatment intervention could furthermore be
explained through the study by Owen et al. (2014). They stated that therapists are likely to choose
a specific approach or treatment intervention if it is commonly used in the clinician’s work
environment which could imply that therapists are likely to use an approach if others use it in their
immediate work environment
(64)
.

79
The second most common reason for using one treatment intervention over another was because
of it being evidence-based. If this is compared to the definition of evidence-based practice, as
defined by Sacket (1996) both these reasons are supported
(54)
. However clinical expertise should
be secondary and integrated to evidence-based practice, and not the other way around, as
suggested by the results of this study
(54)
.
The least popular reason for using a certain approach is because it is scientifically proven, as
reported by only an average of 6 participants. This is interesting, as a study by Owen et al. (2014)
reported that if professionals were taught about certain therapeutic interventions at undergraduate
level they were likely to use that intervention
(64)
. Participants reported that they felt occupational
therapy interventions are not always scientific, but rely more on case studies. They also reported a
lack scientific of evidence to support occupational therapy interventions.
5.4.4 Therapists’ perceived confidence in their knowledge, skill and effectiveness in the
treatment of children with a dual diagnosis of CP and visual impairment
The confidence participants had in their knowledge and skill was similar. Most of the participants
who use a certain treatment intervention were confident in their knowledge of and skill of it. The
participants also felt most confident in their knowledge of and skill in the approaches they most
commonly use, which in most cases was the neurodevelopmental therapy approach. The second-
most commonly used approach, as reported by 24 participants (52.1%), was the somatosensory
approach. The participants felt least confident in their knowledge and skill of the Rood techniques,
and second least in constraint-induced therapy. This is in line with the treatment interventions the
participants used least often, aside from the sensory integration approach. If participants were to
compare the use of the Rood techniques and constraint-induced therapy to literature such as that
of Schultz-Krohn, Royeen, Mccormack, Pope-Davis & Jourdan, (2006) who explored traditional
sensori-motor interventions they would have known it can be useful during therapy adjunct to other
approaches such as the neurodevelopmental therapy or somatosensory approach
(41)(34)(51)
. The
Rood techniques can achieve a desired motor response to assist in therapy
(41)(34)
, so it could be
reasoned that if the participants were up to date with occupational therapy literature on motor
control, they would know the value of the Rood techniques and the constraint-induced therapy and
be able to apply these approaches to their clients in the correct situation.
Interesting differences found between the knowledge and skill of participants was regarding the
neurophysiological and sensory integration approaches. Even though 24 participants reported to
have confidence in their knowledge of and skill in using the neurophysiological approach they still
80
did not apply it. This contradicts research done by Valler (1997), who investigated somatosensory
processing and Kielhofner (1997), who investigated motor control along with the use of the
neurophysiological approach
(44)(46)
. These researchers suggested that this approach can produce
positive outcomes in the treatment of these children, although not consistently as it focuses on
visual and postural aspects
(44)(46)
. This implies that participants could use the approach to test
whether it produces positive results
(44)(46)
. Secondly those qualified in sensory integration did not
feel confident in their knowledge of and skill in this approach when managing children with CP and
visual impairment. The fact that they reported not using it, was contradictory to research by
Glomstad (2004) and other literature investigating the sensory integration approach that supports
its use in the management of these children when participants are qualified
(48)(45)
. Reasons for this
could be that the sensory integration approach was initially and still is more commonly used for
children with learning difficulties, modulation dysfunction and dyspraxia
(47)
. This could be why
participants still prefer to use the approach for those types of difficulties as opposed to children
with a dual diagnosis of CP and visual impairment. Another reason could be that the results of
studies on the use of this approach with these children are still mixed
(37)
.
5.5 Participants’ undergraduate and postgraduate training
The majority of participants (53.6%) reported that their undergraduate training was not sufficient to
manage children with CP. Similarly, 76.8% of participants felt their undergraduate training was
insufficient to manage children with a dual diagnosis of CP and visual impairment. The reason for
this could be that credits differ from university to university which could result in varying knowledge
when occupational therapists complete their undergraduate training
(28)
. Another reason could be
that this is a specialised area in which further training is required to manage these children
effectively
(4)
.
It is interesting to note that even though so many of the participants reported their undergraduate
training to be insufficient to manage these children, 25 participants reported that they have not
attended further training. This is of concern as these participants manage children with a dual
diagnosis of CP and visual impairment even though they believe the only training they have
received is insufficient. This suggests participants are not keeping up to date with current research
and literature, and thus their ability to discern best practices and integrate those with clinical
expertise is below standard, as attending training would ensure participants keep up to date with
best practice and delivering effective management
(54)
.
81
Training at postgraduate level was also reported to be insufficient by 26 participants who reported
that there is insufficient focus on the management of children with a dual diagnosis of CP and
visual impairment. Another reason given for participants not attending postgraduate training was
that courses are inaccessible because they are time consuming, costly, not presented regularly
enough, and have very little focus on the combination of this dual diagnosis. This could also
explain why so few participants had attended further training. Participants not attending courses
results in less clinical expertise as participants are unable to further their clinical training and keep
up with evidence-based practice
(54)
.
This could also suggest that participants value their clinical experience, which includes work
experience, over evidence-based practice. This could further explain why the most common
reason for participants making use of certain therapeutic approaches was because of their work
experience, and not because of research or evidence-based practice. However participants still
indicated that training is important and agreed that training should improve therapeutic outcomes
despite preferring to prize their own experience over available literature, current research and
evidence-based practice to evaluate and direct their treatment. This contradicts evidence-based
practice as it supports using own expertise in the light of and not without the use of new up-to-date
research
(54)
. However, it could also be argued that participants valued their own experience more
than evidence-based practice as they have found that the courses presented are so inaccessible.
Participants also reported that training on the management of children with a dual diagnosis of CP
and visual impairment is limited which could also be a reason participants let their work experience
direct treatment interventions as they feel training to guide them is limited.
5.6 Interventions for children with a dual diagnosis of CP and visual impairment
5.6.1 Most commonly reported outcomes
The two most common short-term outcomes for children with a dual diagnosis, as reported by
37.2% of the participants, were improving visual functioning and improving the execution of and
independence in occupational performance areas. The least common outcomes included family
training, and improving postural and head control. Taking relevant literature into consideration,
outcomes would include improving or compensating for visual impairments, and improving in the
execution of and independence in occupational performance areas
(8)(9)
. However, literature
contradicts the participants’ lack of focus on family training. Tsoi et al. (2011) report that family
training is of utmost importance to implement and sustain the physical and behavioural intervention
strategies recommended for children with CP and visual impairment
(1)
. Also, if participants want to
82
achieve the outcome of improving independence in the execution of daily activities they would
probably have to make use of assistive devices, which, according to Schoonover et al. (2010) and
Tsoi et al. (2011) would be impossible or difficult to implement without family training and
support
(26)(1)
. Relevant literature also contradicts the participants’ lack of focus to compensate for or
accommodate improving postural and head control
(14)(27)
. Therapists should either compensate for
or accommodate these two aspects if they cannot be improved
(14)(16)
.
The most common long-term outcomes for occupational therapy intervention for children with a
dual diagnosis, as reported by 78.6% of the participants, were to achieve maximum independence.
Only 23.9% of participants reported that family training would be very important and 16.7%
reported that they would implement the use of assistive devices. Only two participants (2.4%)
reported that they would focus on quality of life or make use of a multi-disciplinary team.
Improving occupational performance areas is very important, as this will improve quality of life,
which is the ultimate aim of occupational therapy
(9)(31)
. It should go without saying that this should
be the ultimate aim when managing children with CP and visual impairment
(9)(31)
. All participants
with this as the ultimate aim of occupational therapy, which is of particular importance as children
are still learning to be independent and achieving age appropriate developmental milestones, and
these children would struggle to achieve independence because of their many debilitating
impairments
(4)
. Although the majority of the participants deemed independence in the execution of
occupational performance areas very important in both short- and long-term outcomes only some
reported that they would make use of assistive devices. This contradicts research by Schoonover
et al. (2010) that assistive devices are generally prescribed to achieve maximum independence
(26)
,
and therapists need to consider that these children are severely disabled and would most probably
not be able to reach a form of independence without the use of assistive devices
(16)
.
Only 23.9% of the participants reported that family training is important and included it as part of
their long-term outcomes. This contradicts literature that emphasises the importance of family
training
(1)(20)
, such as studies by Tsoi et al. (2011) who investigated the aspects that improve
quality of life and Jeglinsky; Autti-Rämö & Brogren Carlberg (2010) who investigated the
importance of being family-centred during the rehabilitation of children with CP
(1)(20).
They noted
that these children require certain therapy principles including intensity of training, repetition of
interventions and specificity of training to reach positive outcomes, and improve independence and
quality of life, which is why the intervention process requires the family to continue with therapy at
home
(1)(20)
. Family training also ensures that goals are reached and that there is commitment to
83
therapy
(20)
. Without family training (including educating the family on how to manage the child
holistically) and family centeredness (including valuing the family’s goals as well), most of the
reported outcomes, such as achieving maximum independence in occupational performance
areas, would probably not be achieved without family training which the participants failed to report
on.
If we compare these short- and long-term outcomes to the outcomes as set out by the American
Occupational Therapy Association (2011) it should cover the following four domains: children
should be able to participate in activities in a range of environments, interventions should aim to
prevent social isolation, interventions should encourage the child’s development of roles and sense
of competence and interventions should critically analyse transition periods and facilitate or
support moving through these transition periods
(33)
. The two most common short-term outcomes
included that of improving visual functioning and improving the execution of and independence in
occupational performance areas and would then be in line with these four domains as it would
allow the child to participate in age appropriate activities; encourage the child’s development as
well as support moving through transition periods
(33)
. However the lack of focus on family training
would then again make achieving these outcomes difficult as family would be needed to ensure
these goals are reached as previously discussed. Similarly if we look at the long-term outcomes
the focus on achieving maximum independence aligns with the four domains as described by the
American Occupational Therapy Association however the lack of focus on family training and
implementing assistive devices would again impede on fully reaching these outcomes
(33)(20)(26)
.
5.6.2 Changes to treatment interventions to accommodate children with a dual diagnosis of
CP and visual impairment
All of the participants reported that they would change their approach when they discover a child
with CP has a visual impairment. However the reported changes were minimal. The most common
change, as reported by 28.9% of participants, was from a pure motor approach, to a multi-sensory
approach. Another change, as reported by 15.8% of participants was to use a sensory approach
with intense focus on visual training. These changes align with the treatments explored in this
study
(27)
. These children would not have only a motor disability, but as a result of extensive brain
injury there would be multi-system involvement, including the visual impairment, and all of these
would need to be addressed
(4)(8)
which would require a multi-sensory approach
(4)(14)
. A
contradiction emerged between what the participants reported and what literature suggests about
the use of the somatosensory approach over the neurodevelopmental therapy approach. The
84
concern is that literature supports the use of both of these approaches
(43)(38)
and suggests they are
best used in combination
(41)(32)
and not using one or the other as the participants reported.
A concern is that only nine participants (23.7%) reported they would use a multi-disciplinary team,
make environmental adjustments, and use assistive devices and caregivers during training. This
means very few participants supported these changes, which contradicts the literature. These are
all important principles and should be used during treatment, as explored through Schoonover et
al. (2010) who explored the importance of assistive devices for these complicated children,
Jeglinksy et al. (2010) who investigated the importance of multi-disciplinary teams in the
management of these children and Tsoi et al. (2011) who asserted that quality of life should always
be a primary outcome for therapy
(1)(26)(20)(52)
.
5.6.3 Participants’ principles when treating children with a dual diagnosis of CP and visual
impairment
The most common principles used, as discussed in results in 4.6.3, were those of a family-centred
approach and somatosensory approach. Fourteen participants (37.9%) reported to use the
principles of these two approaches to address children with a dual diagnosis of CP and visual
impairment whereas 13 participants (35.1%) used the principles of the neurodevelopmental
therapy approach. This included principles such as analysing movement, normalising tone,
improving postural control to improve movement, making use of repetition, observing and adapting
according to neurological changes and ensuring the use of a combination of principles to improve
independence in occupational performance areas. Only 16.2% of participants included the use of
assistive devices for optimal positioning.
It is positive that most participants reported to use principles that include the family-centred and
somatosensory approaches. Family training is deemed very important by various studies, including
those by Tsoi et al. (2011) and Jeglinsky et al. (2010) and it is encouraging that participants apply
these principles
(1)(20)
. What is of concern, however, is that this was not reflected as part of their
short- or long-term outcomes, or mentioned as part of how they would change their treatment. The
number of participants using of the principles of the somatosensory approach aligns with it being
reported as the second most common approach used. This is positive because, as discussed, this
approach and its principles would be of value when treating these children
(43)
.
The neurodevelopmental therapy approach is the most common approach used as reported by 30
participants (53.4%) but it is only the third-most popular when the principles of the approach are
used. The use of these principles is positive as this approach is considered to be valuable in
85
interventions for these children, and would include encouraging normal movement patterns,
improving postural control and encouraging optimal positioning
(38)(51)
. One concern was the
neurodevelopmental therapy approach no longer supports the idea of normalising tone as this is
not possible
(38)
even though it was one of the principles used, as reported by the participants. A
reason for this could be that participants learnt this from attending a course or from undergraduate
experience years ago and did not keep their knowledge updated. Another concern was that
although the neurodevelopmental therapy approach encourages optimal positioning with or without
the use of assistive devices
(38)
the participants did not give sufficient focus to this.
The participants’ open-ended responses also made scant mention of the value of using multi-
disciplinary teams, which, as reported by Jeglinsky et al. (2010) ensures that goals are reached
and as reported by Njambe et al.(2009) ensures that visual impairments are not overlooked
(20)(11)
.
Schoonover et al. (2010) suggest independence can be achieved through the use of adaptive
equipment, and thus it is concerning that so few participants reported to make use of these in their
principles
(26)
especially because these children would be severely affected and would need
assistive devices to be able to live a quality life
(1)(26)
.
5.6.4 Participants’ perceived success in the treatment of children with a dual diagnosis of
CP and visual impairment
More than half of the participants (62.2%) reported that they experience success in reaching their
outcomes. The most important factor to reach outcomes successfully, as reported by 15
participants (40.5%), was family compliance. As 40.5% of the participants reported that family
compliance is an important factor that contributes to reaching outcomes, it aligns well with the 14
participants (37.5%) who reported to use principles of the family-centred approach. This suggests
that participants who use a family-centred approach have realised the value of it in reaching
success in their treatment
(52)
.
Other factors that played a role in reaching outcomes, as reported by some participants included
the intensity of training, the presence of co-morbidities, the use of multi-disciplinary teams and the
postgraduate training of professionals. This can be linked to participants undervaluing the use of
multi-disciplinary teams. This, as discussed above and described in the literature review is of
utmost importance to ensure best practice. If participants were aware of this, they would have
reported to make use of multi-disciplinary teams. Another concern was that so few participants
reported the value of postgraduate training, which, as discussed in section 5.5, would ensure best
evidence based practice and thus successful outcomes
(54)
.
86
Although the participants felt confident in their treatment only 23 (62.2%) reported to perceive their
treatment to be successful. Reasons could include a lack focus on the use of multi-disciplinary
teams, family training, postgraduate training and adaptive equipment which, as discussed, is
considered very important in ensuring effective intervention for children with a dual diagnosis of CP
and visual impairment
(1)(26)(20)(54)
. Furthermore the reasons for success or failure as reported by
therapists was not the type of outcomes chosen but factors such as family compliance, co-
morbidities in the child etc. For this reason it can hypothesised that participants did not feel that the
type of outcome determined success or failure but rather other factors such as the existence of co-
morbidities, family compliance and other reasons as reported on p. 63 section 4.6.4.
5.6.5 Participants’ perceived confidence in their treatment
The study investigated how the participants viewed their management of children with a dual
diagnosis of CP and visual impairment in terms of the effectiveness of and perceived confidence in
their treatment. The majority of participants (75.2%) considered their treatment as effective,
although only 41.3% felt confident about the effectiveness of their treatment which suggests that
because clinical expertise is based on evidence-based practice and requires ongoing training, a
lack of training can result in less confidence in the management of clients
(54)
.
Participants generally reported that treatment is effective when it is evidence-based which should
ensure best practice. However if the participants practiced evidence-based treatment, it would
result in increased confidence levels and improved management of children with a dual diagnosis
of CP and visual impairment participants. Also, if this statement is considered in the context that
only half of the participants have attended further training it is understandable that their perceived
confidence in their treatment is low, and explains why they did not always support the correct
outcomes and principles according to previous research and existing literature.
Another reason for the discrepancy between the effectiveness of treatment and confidence levels
might be explained by the five participants (12.2%) who felt inexperienced and lacked the
knowledge to manage these children because they had received insufficient training. This led to
either avoiding treating these children or lacking confidence when managing them.
87
5.7 Participants’ perception of the training available in South Africa in the treatment
of children with a dual diagnosis of CP and visual impairment, and how they view
evidence-based practice
As discussed in section 5.5 participants viewed their undergraduate training as insufficient. When
participants had the opportunity to substantiate why they felt this way, responses included there
being limited time available to gain practical knowledge during undergraduate training, lecturers
being inexperienced and there being insufficient time during undergraduate training to focus on
such a speciality. This can be linked again to discrepancies in university syllabuses regarding how
much time and credits are devoted to specific aspects, which results in therapists varying in
knowledge once they qualify
(28)
.
According to 26 participants (63.4%) postgraduate training in South Africa is insufficient, and the
reasons for this are multiple. Some participants reported that although quality courses are
available, specifically from SANDTA this is not enough. The reasons for this have been discussed
in section 5.3. Five participants (12.2%) reported they felt inexperienced and lacked the knowledge
to manage these children which led to either avoiding treating them or lacking confidence when
managing them. This illustrates why evidence-practice first taking into account the most up-to-date
research should be paramount followed by clinical expertise and not the other way around
(54)
.
5.8 Implications for current practice
When comparing assertions made in the literature review to current occupational therapy practice
for children with a dual diagnosis of CP and visual impairment, it is clear that therapists showed a
lack of knowledge of the different types of treatment interventions available. They also did not
always follow best practice. This shows that there is a need for guidance on available treatments. It
is also important to note that this study investigated which treatment interventions the occupational
therapists use, as well as their perceived confidence in knowledge of and skill in their treatment.
This was important as it provided information on the effectiveness of current treatment from a
clinical perspective. Although therapists reported to feel confident in their skill in and knowledge of
the treatment regimes they use there are other treatment regimes available that therapists were
not aware of and/or not using that are supported by research and literature. Furthermore, although
the participants had confidence in their treatment, they were not confident in the success of it. This
means that even though the participants believed they were using treatment that should be
effective, they were not sure of its effectiveness. This might affect their clinical expertise and result
in ineffective treatment.
88
This study highlights the importance of evidence-based practice. This would ensure that therapists
first make decisions based on current, thoroughly researched data before they make use of their
own clinical expertise where it appears most therapists’ first look towards their clinical expertise
before taking the most up-to-date research into account. This links with the objective of the
research to determine and ensure therapists still make use of evidence-based practice.
As it is difficult to say absolutely what the best approach should be for children with a dual
diagnosis of CP and visual impairment there are a few guidelines every therapist should follow. It is
important to make use of a multi-disciplinary team and include a family-centred approach, as this
ensures that therapeutic goals are reached.
When taking all of this into consideration useful approaches for therapists to consider when
managing children with a dual diagnosis of CP and visual impairment include the
neurodevelopmental therapy approach, neurophysiological approach, somatosensory approach,
sensory integration approach, family-centred approach, compensatory approach and the use of
multi-disciplinary teams. These approaches are best used in combination. Another important factor
to note is that therapists should allow evidence-based practice to guide their therapy and then
integrate their clinical expertise to ensure these children are treated in the best way possible.
If participants were aware of all possible treatment interventions, it would improve the outcomes
and principles they use during the management of these complicated children. This awareness, as
shown through this study, would then ensure treatment is more successful as outcomes would be
reached more effectively.
It is worth mentioning that the availability of postgraduate training should be addressed, as this
was a major problem for therapists, as noted by the participants, and results less prevalent
evidence-based practice and a decline in clinical expertise. A reason for this could be that
therapists are not always familiar with the concept of evidence-based practice, lack the skill to
apply it or lack organisational support as explained through the study of Benevides, Vause-Earland
& Walsh (2015) and for this reason do not know how to apply it
(58)
.
5.9 Conclusion
This study aimed to investigate occupational therapy interventions used by therapists in South
Africa to guide their treatment for children with a dual diagnosis of CP and visual impairment. It
also investigated their skill in and knowledge of their treatment interventions, as well as their
perceived confidence in their ability to manage these children.
89
Therapists use combinations of the different approaches and treatment modalities, such as the
neurodevelopmental therapy approach and somatosensory approach, which aligns with the
relevant literature. However, they lack knowledge of other treatment interventions such as
neurophysiological approach, compensatory approach, family centred approach, multi-disciplinary
team approach and Rood techniques. What was positive to note though, is that therapists’ reported
knowledge of certain treatment intervention and their perceived skill in applying this knowledge
was more or the less the same.
Also positive is that participants had good knowledge of and skill in these approaches and could
provide positive answers to the outcomes and principles used in their treatment. However, as they
lacked knowledge on various important approaches and treatment interventions, it was significant
to note the extent to which this negatively affected their outcomes and principles. It was clear that
their lack of knowledge on specific treatment interventions meant that participants lack certain
principles and outcomes that, according to literature, should be primary in the treatment of these
complicated children.
Therapists also reported to be aware when a child with CP has a visual impairment. Even though
through the data in this study, suggests participants often overlook visual impairments, they still
reported to be aware of them. Participants further reported to change their treatment once they
became aware a child with CP has a visual impairment. This is significant, as this study provided
critical arguments for why treatment interventions for children with CP alone cannot be the same
as those for children with CP and visual impairments.
Even though participants perceived their treatment as effective their perceived confidence levels
were low, which implies that even though they reported to have good knowledge of and skill in their
treatment, they do not feel confident about it.
The majority of the participants considered their undergraduate training to be insufficient. Most of
them agreed that any form of postgraduate training is important to ensure they provide best
practice and reach their outcomes although this is limited as many participants reported not to
have undergone any further or specialised training on the management of these children.
Participants gave various reasons for why courses were inaccessible. This requires further
investigation and possible intervention.

90
Chapter 6: Conclusion
To summarise, the objectives of the study was to determine the occupational therapy interventions
used to treat children with a dual diagnosis of CP and visual impairment; and determine
occupational therapists perception of confidence in their knowledge, training and skill to treat
children with a dual diagnosis of CP and visual impairment and this study has met its objectives.
After thorough investigation there are still no clear indication as to what is the best approach to use
when children have a dual diagnosis of CP and visual impairment as many of the treatment
interventions reviewed did not provide consistently successful results in the management of these
complicated clients. However, some approaches are better and were elucidated through this study
such as the family centred approach
(20)
, compensatory approach
(26),
neurodevelopmental therapy
approach
(38)
, neurophysiological approach
(41)
, somatosensory approach
(43)
, multi-disciplinary team
approach
(20)
and sensory integration
(48)
all of which were recommended by relevant literature and
studies that provided proof that these appraoches could be successfully applied. The literature also
suggested that approaches should be used in combination
(41)(8)
, and that they are best used when
therapists are trained and feel confident in them so that evidence-based practice can be integrated
with clinical expertise
(54)(55)
.
One of the objectives was to investigate the current practice for children with a dual diagnosis of
CP and visual impairment. There is some uniformity in the therapeutic approaches occupational
therapists use in South Africa the most common being the neurodevelopmental therapy approach
and the somatosensory approach. These align with literature as discussed
(38)(43)
, as discussed in
Chapter 2. The neurodevelopmental therapy approach is also the most common approach for
which participants received postgraduate training. The concern is that the participants lacked focus
on treatment interventions such as the family-centred approach, compensatory approach, multi-
disciplinary team approach, neurophysiological approach and sensory integration approaches. The
participants either reported not to make use of these treatment interventions or their principles or
very few participants reported on applying their principles to ensure success in outcomes. Another
concern was that some of the principles the participants used such as trying to normalise tone was
not supported by literature anymore
(38)
. Therapists also reported that the main reason for applying
a therapeutic intervention is because it is commonly used at their workplace and secondly because
the intervention was evidence-based, which indicates that they value their clinical expertise above
91
evidence-based practice. Although clinical expertise that results from work experience should be
integrated with evidence-based theory, it should not be the primary reason for applying a treatment
intervention. This suggests therapists do not always use the best evidence-based practice when
managing these complicated children. Participants also reported to feel confident in their skill and
knowledge of their treatment interventions and although they saw their treatment as effective they
did not feel confident in it. This again points to therapists prizing their clinical expertise above
evidence-based practice (which would ensure best care and build confidence) to guide their
treatment.
This study discovered that the majority of participants regarded their undergraduate training to be
insufficient in the management of these complicated clients. This emphasised the need to receive
further training to manage children with a dual diagnosis of CP and visual impairment effectively.
However, the participants gave various reasons for why postgraduate training is not easily
accessible, explaining why many of them had not attend any postgraduate training to improve their
knowledge and skill specifically related to this complicated disability which could be connected to
therapists’ lack of confidence in managing these complicated clients. This then indicates the need
and importance for therapists to undergo regular training to keep up to date with research and best
evidence-based practice to build their confidence. Ensuring therapists remain up to date with
current research would result in therapy guided primarily by evidence-based practice and
supported by clinical expertise
(55)(54)
.
This study argued that therapy for children with CP alone and those with CP and an additional
visual impairment cannot be the same. The reasons for this have been thoroughly explored in this
study among them that the World Health Organisation stated that vision is essential for
independence
(25)
and that some sort of vision is required to use most assistive devices
(26)
. This in
itself suggests that therapy would need to be adapted if a child with CP is discovered to have a
visual impairment. Another factor contributing to this complicated intervention process is that,
according to a study by Njambe et al. (2009) these visual impairments are often overlooked
(11)
.
Thus it was significant to note that participants reported to be aware when a child with CP has a
visual impairment, and recommended therapy should be adjusted if the child presented this
condition. Although this study suggests that therapists sometimes overlook these visual
impairments (as many participants reported that there are minimal visual impairments in their CP
caseload), it is still encouraging that they felt they were aware of the visual impairment and
recognised a need to change their treatment when confronted with this. It is concerning, however
that the changes the participants reported to apply were limited. Participants still lacked knowledge
92
of the application of the compensatory approach, the family-centred approach and the multi-
disciplinary approach which are all recommended specifically to address this change in treatment
and assist in reaching outcomes
(26)(20)(11)(39)
.
The participants’ responses revealed that their knowledge of relevant literature and research is
limited as is their access to courses. They were not aware of all the different treatment
interventions and reported not to use certain appropriate interventions or principles that could be of
value. Furthermore, they reported to still use principles that are no longer supported by research,
which should be addressed to give the participants the knowledge and skills they need when
managing these complicated children.
6.1 Suggested further research
As it is clear that there is limited research and courses available to guide therapists in managing
these clients, it is recommended that further research be done to set up a protocol for occupational
therapists to follow when treating a child with a dual diagnosis of CP and visual impairment. This
would allow for therapists to follow evidence-based practice and integrate it with clinical expertise.
6.2 Limitations to this study
Although extensive steps were taken the small number of participants cannot be representative of
all occupational therapists in South Africa treating children with a dual diagnosis of CP and visual
impairment. Other limitations that could have added value to the information obtained included:
firstly participants were not able to add their own approaches to the list of approaches provided
when indicating approaches they used for treatment and they were also not able to indicate which
approaches they combine during treatment. This could have added value to the discussion on
treatment interventions which were one of the objectives of this study. Secondly participants had to
indicate their years’ of experience according to predetermined category sizes which resulted in
uneven category sizes. This could have rather been presented in an open-ended question so that
once results were calculated the years of experience categories could be calculated in even sizes.
Lastly participants had to indicate where they worked but the category of clinic did not distinguish
whether it was a clinic in the hospital or clinic in the community.

93
REFERENCES
1.
Tsoi WSE, Zhang LA, Wang WY, Tsang KL, Lo SK. Improving quality of life of children with
cerebral palsy: a systematic review of clinical trials. Child: care, health and development. 2011
April; 38(1): p. 21-31.
2.
Organization WH. WHO. [Online].; 2008 [cited 2014 January 16. Available from:
www.who.int/enity/gho/publication.
3.
Kirby RS, Wingate MS, van Naarden Braun K, Doernberg NS, Arneson CL, Benedict RE,
Mulvihill B, Durkin MS, Fitzgerald RT, Maenner MJ, Patz JA, Yeargin-Allsopp M. Prevalence
and functioning of children with cerebral palsy in four areas of the United States in 2006: A
report from the Autism and Developmental Disabilities Monitoring Network. Research in
developmental disabilities. 2011 January; 32: p. 462–469.
4.
Rogers SL. Common conditions that influence children's participation. In Falk K, editor.
Occupational Therapy For Children. 6th ed. Maryland Heights: Mosby Elsevier; 2010. p. 146-
193.
5.
O'Shea TM. Diagnosis, treatment and prevention of Cerebral Palsy. Clinical Obstetrics and
Gynecology. 2008 December; 51(4): p. 816-822.
6.
van Toorn R, Laughton B, van Zyl N. Aetiology of cerebral palsy in children presenting at
Tygerberg Hospital. SA Journal of Child Health. 2007 July; 1(2): p. 74-77.
7.
LoWing K, Bexelius A, Carlberg EB. Goal-directed functional therapy: A longitudinal study on
gross motor function in children with cerebral palsy. Disability and Rehabilitation. 2010; 32(11):
p. 908-916.
8.
Steultjens EM, Dekker J, Bouter LM, van de Nes JC, van de Lambregts BL, Ende CH.
Occupational therapy for children with cerebral palsy: a systematic review. Clinical
Rehabilitation. 2003 July 20; 18(1): p. 1-14.
9.
Association AOT. Occupational therapy practice framework: Domain and process (3rd ed.).
American Journal of Occupational Therapy. 2014; 62(5): p. 625 - 683.
10
Fazzi E, Signorini SG, La Piana R, Bertone C, Misefari W, Galli J, Balottin U, Bianchi PE.

94
.
Neuro-ophthalmological disorders in cerebral palsy: ophthalmological, oculomotor, and visual
aspects. Developmental Medicine & Child Neurology. 2012 March; 54: p. 730–736.
11
.
Njambi L, Kariuki MM, Masinde S. Ocular findings in children attending occupational therapy
clinic at Kenyatta National Hospital, Nairobi, Kenya. East African Journal of Ophthalmology.
2009 July; 15(1): p. 21-26.
12
.
Swift SH, Davidson RC, Weems LJ. Cortical Visual Impairment in Children: Presentation
Intervention, and Prognosis in Educational Settings. TEACHING Exceptional Children Plus.
2008 May; 4(5): p. 1-14.
13
.
Boot F, Pel J, Evenhuis H, van der Steen J. Factors related to impaired visual orienting
behavior in children with intellectual disabilities. Research in developmental disabilities. 2012
May; 33: p. 1670-1676.
14
.
Alliance CP. Cerebral Palsy Alliance. [Online].; 2006 [cited 2013 February 26. Available from:
http://www.cerebralpalsy.org.au/about-cerebral-palsy/basic-guide-to-cerebral-
palsy/interventions.
15
.
Palisano RJ, Snider LM, Orlin MN. Recent Advances in Physical and Occupational Therapy for
Children With Cerebral Palsy. Pediatric Neurology. 2004 March; 11(1): p. 66–77.
16
.
Stanger M, Oresic S. Rehabilitation approaches for children with Cerebral Palsy: Overview.
Journal of Child Neurology. 2003 September; 18(1): p. 79-88.
17
.
Odding E, Roebroeck ME, Stam HJ. The epidemiology of cerebral palsy: Incidence,
impairments and risk factors. Disability and Rehabilitation. 2006 February; 28(4): p. 183-191.
18
.
Bax M, Goldstein M, Rosenbaum P, Leviton A, Paneth N. Proposed definition and classification
of cerebral palsy. Developmental Medicine & Child Neurology. 2005 April; 47: p. 571–576.
19
.
Scotland ASC. Cerebral Palsy and Visual Impairment. [Online].; 2011 [cited 2015 February 27.
Available from: www.capability-scotland.org.uk.
20
.
Jeglinsky I, Autti-Rämö I, Brogren Carlberg E. Professional background and the
comprehension of family-centredness of rehabilitation for children with cerebral palsy. Child:

95
care, health and development. 2010 December; 38(1): p. 70-78.
21
.
Shafer S. Cerebral Palsy and children with vision and hearing loss. [Online].; 1998 [cited 2013
March 9. Available from: http://www.tsbvi.edu/seehear/fall98/cpvh.htm.
22
.
Teasell R, Hussein N. Evidence Based Review of Stroke Rehabilitation. [Online].; 2013 [cited
2014 March 28. Available from: www.ebrsr.com.
23
.
Crouch R. The impact of poverty on the service delivery of occupational therapy in Afrcia. In
Alers V, Crouch R, editors. Occupational Therapy: An African Perspective. Johannesburg:
Sarah Shorten Publishers; 2010. p. 98-112.
24
.
Russel E, Nagaishi PS. Hospital and Paediatric Rehabilitation Services. In Falk K, editor.
Occupational Therapy for Children. 6th ed. Missouri: Mosby Elsevier; 2010. p. 744-785.
25
.
Mashele NP, Smit N. Comparing the effect of different living environments on the development
of independent living skills in children with visual impairment. South African Journal of
Occupational Therapy. 2011 December; 41(3).
26
.
Schoonover J, Argabrite Grove RE, Swinth Y. Influencing Participation Through Assistive
Technology. In Falk K, editor. Occupational Therapy for Children. 6th ed. Missouri: Mosby
Elsevier; 2010. p. 583-620.
27
.
Steultjens EM, Dekker J, Bouter LM, van de Nes JC, van de Lambregts BL, Ende CH.
Occupational therapy for children with cerebral palsy: a systematic review. Clinical
Rehabilitation. [Online].; 2004 [cited 2013 February 27. Available from:
http://www.ncbi.nlm.nih.gov/pubmed/14763715.
28
.
Deacy RM, Yuen HK, Barstow EA, Warren M, Vogtle LK. Survey of the Low Vision
Rehabilitation Curricula in Occupational Therapy and Occupational Therapy Assistant
Programs. The American Journal of Occupational Therapy. 2012 November/December; 66(6):
p. 114-118.
29
.
Russel E, Nagaishi PS. Services for Children with Visual or Auditory Impairments. In Falk K,
editor. Occupational Therapy for Children. 6th ed. St. Louis: Mosby Elsevier; 2010. p. 744-785.

96
30
.
Kielhofner G. The Biomechanical Model. In Mallinson T, editor. Conceptual Foundations of
Occupational Therapy.: F.A. Davis; 2009. p. 91-106.
31
.
Case-Smith J, Law M, Pollock CM, Stewart D. Foundations for Occupational Therapy Practice
with Children. In Falk K, editor. Occupational Therapy for Children. 6th ed. Missouri: Mosby
Elsevier; 2010. p. 22-56.
32
.
Berry J, Ryan S. Frames of Reference: their Use in Paediatric Occupational Therapy. British
Journal of Occupational Therapy. 2002 September; 65(9): p. 420-427.
33
.
Bendixen RM, Kreider CM. Review of Occupational Therapy Research in the Practice Area of
Children and Youth. The American Journal of Occupational Therapy. 2011 May/June; 65(3): p.
351-359.
34
.
Schultz-Krohn W, Royeen CB, Mccormack G, Pope-Davis SA, Jourdan JM. Traditional
Sensorimotor Approaches To Intervention. In Falk K, editor. Pedretti's Occupational Therapy:
Practice Skills for Physical Dysfunction. St. Louis: Mosby Elsevier; 2013. p. 726-747.
35
.
Levac D, DeMatteo C. Bridging the gap between theory and practice: Dynamic systems theory
as a framework for understanding and promoting recovery of function in children and youth
with acquired brain injuries. Physiotherapy Theory and Practice. 2009; 25(8): p. 544–554.
36
.
O'Brien J. Application Of Motor Control/Motor Learning to Practice. In Case-Smith J, O'Brien
JC, editors. Occupational Therapy For Children And Adolescents. 7th ed. St. Louis: Elsevier
Mosby; 2015. p. 193-220.
37
.
Diane Parham L, Mailloux Z. Sensory Integration. In Falk K, editor. Occupational Therapy for
Children. 6th ed. Missouri: Mosby Elsevier; 2010. p. 325-373.
38
.
Butler C, Darrah J. Effects of Neurodevelopmental Treatment (NDT) for Cerebral Palsy: An
AACPDM evidence report. Developmental Medicine & Child Neurology. 2001 July; 43: p. 778-
790.
39
.
Northern Territory Government of Australia. Department of Health. [Online].; 2015 [cited 2015
August 3. Available from:
http://www.health.nt.gov.au/Cancer_Services/CanNET_NT/Multidisciplinary_Teams/index.aspx
97
.
40
.
Mandich A, Wilson J, Gain K. Cognitive Interventions for Children. In Case-Smith J, O'Brien
JC, editors. Occupational Therapy for Children and Adolescents. 7th ed. St. Louis: Elsevier
Mosby; 2015. p. 304-320.
41
.
O'Brien JC, Williams H. Application of Motor Control/Motor Learning to Practice. In Falk K,
editor. Occupational Therapy for Children. 6th ed. Missouri: Mosby Elsevier; 2010. p. 245-275.
42
.
Schultz-Kroon W, McHugh Pendleton H. Application of the Occupational Therapy Practice
Framework to Physical Dysfunction. In Falk K, editor. Occupational Therapy Practice Skills for
Physical Dysfunction. 6th ed. St. Louis: Mosby Elsevier; 2013. p. 28-52.
43
.
Pavão SL, dos Santos Silva FP, Savelsbergh GJ, Ferreira Rocha NA. Use of Sensory
Information During Postural Control in Children With Cerebral Palsy: Systematic Review.
Journal of Motor Behavior. 2014 December; 10(1080): p. 1-11.
44
.
Vallar G. Spatial frames of reference and somatosensory processing: a neuropsychological
perspective. The Royal Society. 1997; 352: p. 1401-1409.
45
.
Kielhofner G. The Sensory Integration Model. In Mallinson T, editor. Conceptual Foundations
of Occupational Therapy.: F.A. Davis; 2009. p. 185-202.
46
.
Kielhofner G. The Motor Control Model. In Mallinson T, editor. Conceptual Foundations of
Occupational Therapy.: F.A. Davis; 2009. p. 170-184.
47
.
van Jaarsveld A. Sensory integration in mental retardation and pervasive developmental
disorders. In Crouch R, Alers V, editors. Occupational therapy in psychiatry and mental health.
5th ed. Londen: Whurr Publishers Ltd; 2015. p. 369-392.
48
.
Glomstad J. Burden of proof: Occupational therapists are researching the science behind
sensory integration. Advance for Occupational Therapy Practitioners. 2004 October;: p. 1-33.
49
.
Kleim JA, Jones TA. Principles of Experience-Dependant Neural Plasticity: Implications for
Rehabilitation after Brain Damage. Journal of Speech, Language, and Hearing Research. 2008
February; 51: p. S225-S239.

98
50
.
Hurst CM, Van de Weyer S, Smith C, Adler PM. Improvements in performance following
optometric vision therapy in a child with dyspraxia. Ophthalmic and Physiological Optics. 2006
February; 26(2): p. 199-210.
51
.
Sugden D, Dunford C. Intervention and the role of theory, empiricism and experience in
children with motor impairment. Disability and Rehabilitation. 2007 January; 29(1): p. 3-11.
52
.
Oien I, Fallang B, Ostensjo S. Goal-setting in paediatric rehabilitation: perceptions of parents
and professional. Child: care, health and development. 2009 August; 36(4): p. 558–565.
53
.
Law MC, Darrah J, Pollock N, Wilson B, Russel DJ, Walter SD, Rosenbaum P, Galuppi B.
Focus on function: a cluster, randomized controlled trial comparing child- versus context-
focussed interventionfor young children with cerebral palsy. Developmental Medicine and Child
Neurology. 2011 July; 53(7): p. 621-629.
54
.
Von Isenburg M, Handler L. Duke University Medical Centre. [Online].; 2015 [cited 2015
February 18. Available from: http://guides.mclibrary.duke.edu/ebmtutorial.
55
.
Bennett S, Bennett JW. The process of evidence-based practice in occupational therapy:
Informing clinical decisions. Australian Occupational Therapy Journal. 2000 August; 47: p. 171-
180.
56
.
AlleyDog. AlleyDog.com. [Online].; 2015 [cited 2015 May 18. Available from:
http://www.alleydog.com/glossary/definition.php?term=Perceived%20Competence.
57
.
Gitlow L, Depoy E. Evidence-Based Practice for Occupational Therapy. In Falk K, editor.
Pedretti's Occupational Therapy: Practice Skills for Physical Dysfunction. 6th ed. St. Louis:
Mosby Elsevier; 2013. p. 53-63.
58
.
Benevides TW, Vause-Earland T, Walsh R. Impact of a Curricular Change on Perceived
Knowledge, Skills, and Use of Evidence in Occupational Therapy Practice: A Cohort Study.
The American Journal of Occupational Therapy. 2015 September/October; 69(1): p. 1-9.
59
.
Creswell JW, Ebersohn L, Eloff I, Ferreira R, Ivankova NV, Jansen JD, et al. First steps in
Research. 5th ed. Maree K, editor. Pretoria: Van Schaik Publishers; 2010.

99
60
.
SurveyMonkey. Survey Monkey. [Online].; 2009 [cited 2016 February 4. Available from:
https://www.surveymonkey.com/mp/aboutus/.
61
.
SurveyMonkey. SurveyMonkey. [Online].; 2015 [cited 2015 May 14. Available from:
https://www.surveymonkey.com/mp/likert-scale/.
62
.
Yaghmale F. Content validity and its estimation. Journal of Medical Education. 2003 ; 3(1): p.
25-27.
63
.
Penwarden R. FluidSurveys University. [Online].; 2014 [cited 2015 March 27. Available from:
http://fluidsurveys.com/university/response-rate-statistics-online-surveys-aiming/.
64
.
Owen A, Adams F, Franzsen D. Factors influencing model use in SA. SAJOT. 2014; 44(1): p.
41-48.

100
Appendix A
Information letter
Good morning/afternoon,
I am Zonè Janse van Rensburg, a MSc occupational therapy student at the Wits University. I am
currently doing a research project to achieve my MSc in occupational therapy. I am looking at the
current occupational therapy (OT) interventions used for children diagnosed with Cerebral Palsy
(CP) and visual impairment. This study will aim to investigate what the current OT treatment entail
for children with CP and visual impairment, what the skill and perceived confidence levels are of
OT’s that manage children with CP and visual impairment and if there are any gaps in how we
treat these children. I would like to invite you to please take part in this study should you fit the
criteria.
This will only take about 20 minutes of your time. In order for you to take part in this study please
make sure that you fit the population criteria: If you are a qualified and registered occupational
therapist working in either the public or private sector with a minimum of six months working
experience with children diagnosed with Cerebral Palsy, I would like to invite you to participate in
this research. Please ensure that you complete every section to ensure the reliability and validity
of this study. Please note that no single person including the researcher will have any access to
your personal information. To protect your integrity the questionnaires will be kept anonymous
and the only link the researcher will have to you is your IP address. Taking this into consideration
please ensure that you complete every question honestly and comprehensively. If you
participated in the pilot study please refrain from participating in the study now.
Participation in the study is voluntary but your participation will be greatly appreciated as it will
assist in the reliability of the study. Please note that should you complete this questionnaire it will
serve as informed consent to participate in the study and your information will be used to describe
the results of the study. In order to protect the validity and reliability of this study please complete
this study only once and refrain from speaking to your colleagues about your answers.
Feedback on the results of the research will be available on request.
Please contact me on the details below should you have any questions. If you have any
complaints or ethical queries, please contact the chairman of the Human Research Ethics
Committee, Prof P Cleaton Jones at Anisa.Keshav@wits.ac.za or on 011 717 1234.
101
If you agree to participate, please continue to the survey.
Regards,
Zonè Janse van Rensburg
072 240 8673

102
Appendix B
QUESTIONNAIRE
Within this questionnaire the following will be important for participants to understand:
CP is short for the condition cerebral palsy
Visual impairment implies
low vision, poor visual acuity or decreased visual field
blindness including cortical blindness – no vision or neurological blindness where
there is total or partial visual loss in a normal appearing eye
strabismus – which implies that the eyes are not aligned properly and point in
different directions
astigmatism – optical defect where vision is blurred
stereopsis – where there is a difficulty to perceive depth perception
nystagmus – involuntary eye movement
In the child this presents as difficulty to fixate on objects, follow objects, visual
processing and understanding objects, poor figure ground and depth perception,
spatial relational issues and lastly having a decreased visual field
SECTION A.1:
Demographic information
1. Male
Female
2. Where did you complete your undergraduate training?
____________________________________________________________________
3. What year did you qualify? _____________________________________________
4. Where are you currently working?
Public sector
Private sector
Both
5. In what area are you currently working in?
Hospital
Clinic
Community
School
Private practice
NGO
Other: _______
6. Have you had any other specific training, besides undergraduate training, in the
Yes
No
103
rehabilitation of children with CP?
If your answer was yes, please specify with name and duration of course:
__________________________________________________________________________
__________________________________________________________________________
__________________________________________________________________________
7. What percentage of your current caseload is made up of CP children? ____________
8. What percentage of your current CP caseload has some form of visual impairment?
_______________________ .
9. What type of visual impairments relating to your CP caseload do you see at your practice?
Please tick appropriate box:
Low vision/poor visual acuity
Strabismus
Nystagmus
Astigmatism
Stereopsis
Blindness
10. How many years have you been working with children diagnosed with CP? Please tick
appropriate block.
0 – 1
1 – 2
2 – 5
5 – 10
10 – 15
15+
If you are currently or have in the past worked with children with a dual diagnosis of CP and
visual impairment please continue to Section B
SECTION B.1:
This section will gather information related to post graduate training in the form of courses,
diplomas or degrees.
1. My undergraduate training was adequate to guide me in managing children diagnosed with
CP and visual impairment.

104
Strongly agree
Agree
Neutral
Disagree
Strongly disagree
2. I attend continuous professional development (CPD) courses directed to improve my
knowledge and skill with treating children diagnosed with CP and visual impairment.
Strongly agree
Agree
Neutral
Disagree
Strongly disagree
3. The above mentioned courses assist me to improve my management of children diagnosed
with CP and a visual impairment
Strongly agree
Agree
Neutral
Disagree
Strongly disagree
4. CPD courses or post graduate courses that focus on management of children diagnosed
with CP and visual impairment are easily accessible to attend with regards to being
affordable.
Strongly agree
Agree
Neutral
Disagree
Strongly disagree
5. CPD courses or post graduate courses that focus on management of children diagnosed
with CP and visual impairment are easily accessible to attend as it is presented regularly
Strongly agree
Agree
Neutral
Disagree
Strongly disagree
6. The CPD courses are scientifically proven and evidence based to improve the outcome of
therapy with children diagnosed with CP and visual impairment
Strongly agree
Agree
Neutral
Disagree
Strongly disagree

105
SECTION B.2:
Treatment intervention including modalities and frames of references
1. I know when a child diagnosed with CP has a visual impairment.
Strongly agree
Agree
Neutral
Disagree
Strongly disagree
2. I always make use of a Multi-disciplinary approach when treating a child diagnosed with CP
and visual impairment.
Strongly agree
Agree
Neutral
Disagree
Strongly disagree
3. I change my treatment management when I treat a child diagnosed with CP and a visual
impairment compared to the management of a child diagnosed only with CP.
Strongly agree
Agree
Neutral
Disagree
Strongly disagree
Please elaborate on how you change your treatment: ________________________________
___________________________________________________________________________
___________________________________________________________________________
Which of the following approaches do you use in your workplace? (Answer by using the
number that correlates with the following scale to describe how often you use the
approach)
Always: 5
Very often: 4
Sometimes: 3
Seldom: 2
Never: 1
Neurophysiological frame of reference
Neurodevelopmental therapy approach
Rood techniques
Neurodevelopmental technique (qualified in NDT)
Somatosensory approach (using children’s sensory systems)
Sensory integration approach
Sensory integration techniques (only if you are a qualified SI therapist)
Constraint-induced therapy
106
I feel these approaches are best used in combination with each other
Strongly agree
Agree
Neutral
Disagree
Strongly disagree
I use these approaches because it is effective: (Please mark with a tick all the answers
applicable to you)
Approaches
Due to my
undergraduate
training
experience
Due to my
work
experience
in this field
Because it
is used at
my
workplace
Because it
is
scientifically
proven
Because it
is evidence
based
Neurophysiological
Neurodevelopmental
Rood techniques
NDT
Somatosensory
Sensory integration
Approach
SI qualification
techniques
Constrain induced
therapy
SECTION C:
Personal knowledge, confidence and skill in treatment intervention
Treatment according to undergraduate training:
My undergraduate training with regard to the management of children diagnosed with CP is
adequate to effectively manage children diagnosed with CP.

107
Strongly agree
Agree
Neutral
Disagree
Strongly disagree
My undergraduate training with regard to the management of children diagnosed with CP
and with visual impairments is adequate to effectively manage these children.
Strongly agree
Agree
Neutral
Disagree
Strongly disagree
Treatment according to all training
I am confident that my knowledge of the theories and frames of references used in the
treatment of children diagnosed with CP and visual impairment is good. (Answer by using
the number that correlates with the following scale to describe how much you agree with
this statement)
Very Good: 5
Good: 4
Barely
acceptable: 3
Poor: 2
Very poor: 1
Neurophysiological frame of reference
Neurodevelopmental therapy approach
Rood techniques
Neurodevelopmental technique (qualified in NDT)
Somatosensory approach (using children’s sensory systems)
Sensory integration approach
Sensory integration techniques (only if you are a qualified SI therapist)
Constraint-induced therapy
I am confident that my skill in applying these theories and frames of references used in the
treatment of children diagnosed with CP and visual impairment is good. (Answer by using
the number that correlates with the following scale to describe how much you agree with
this statement)
Very Good: 5
Good: 4
Barely
acceptable: 3
Poor: 2
Very poor: 1
108
Neurophysiological frame of reference
Neurodevelopmental therapy approach
Rood techniques
Neurodevelopmental technique (qualified in NDT)
Somatosensory approach (using children’s sensory systems)
Sensory integration approach
Sensory integration techniques (only if you are a qualified SI therapist)
Constraint-induced therapy
I feel my treatment of children diagnosed with CP and visual impairment is effective
Strongly agree
Agree
Neutral
Disagree
Strongly disagree
I feel confident when I treat children diagnosed with CP and visual impairment
Strongly agree
Agree
Neutral
Disagree
Strongly disagree
What do you see as the three most functional short term aims during a session for children
diagnosed with CP and visual impairment: ___________________________________
______________________________________________________________________
_____________________________________________________________________
_____________________________________________________________________
_____________________________________________________________________
13. What do you see as the three most functional long term outcomes for children diagnosed with
CP and visual impairment:
______________________________________________________________________________
______________________________________________________________________________
______________________________________________________________________________
______________________________________________________________________________
14. What do you see as the most important principles needed in order to reach functional
outcomes in the treatment of children diagnosed with CP and visual impairment?

109
______________________________________________________________________________
______________________________________________________________________________
______________________________________________________________________________
______________________________________________________________________________
15. Are you successful in reaching these outcomes? Please explain:
______________________________________________________________________________
______________________________________________________________________________
______________________________________________________________________________
______________________________________________________________________________
Do you change/adapt your treatment by using different approaches or different
combinations when the child diagnosed with CP has a visual impairment, please explain:
________________________________________________________________________
________________________________________________________________________
________________________________________________________________________
________________________________________________________________________
________________________________________________________________________
Do you feel that the training available in South Africa is sufficient to educate therapists on
how to treat children diagnosed with a dual diagnosis of CP and visual impairment? Please
explain your answer:
________________________________________________________________________
________________________________________________________________________
________________________________________________________________________
________________________________________________________________________
________________________________________________________________________
________________________________________________________________________
As an occupational therapists do you support that the treatment for children with a dual
diagnosis of CP and visual impairment should be evidence based and scientifically proven
and what is your understanding of the terms evidence based practice:
________________________________________________________________________
________________________________________________________________________
________________________________________________________________________

110
________________________________________________________________________
________________________________________________________________________
Thank you for your time

111
Appendix C
Ethics Clearance Certificate
