
2023 AAHA Management of Allergic Skin Diseases
in Dogs an d Ca ts Guidelines
Julia Miller, DVM, DACVD,
†
Andrew Simpson, DVM, MS, DACVD,
†
Paul Bloom, DVM, DACVD, DABVP (Canine and Feline), Alison Diesel, DVM, DACVD,
Amanda Friedeck, BS, LVT, VTS (Dermatology), Tara Paterson, DVM, MS, Michelle Wisecup, DVM,
Chih-Ming Yu, DVM, MPH, ECFVG
ABSTRACT
These guidelines present a systematic approach to diagnosis, treatment, and management of allergic skin diseases in
dogs and cats. The guidelines describe detailed diagnosis and treatment plans for flea allergy, food allergy, and atopy in
dogs and for flea allergy, food allergy, and feline atopic skin syndrome in cats. Management of the allergic patient entails
a multimodal approach with frequent and ongoing communication with the client. Obtaining a comprehensive history is
crucial for diagnosis and treatment of allergic skin diseases, and the guidelines describe key questions to ask when presented
with allergic canine and feline patients. Once a detailed history is obtained, a physical examination should be performed, a
minimum dermatologic database collected, and treatment for secondary infection, ectoparasites, and pruritus (where indi-
cated) initiated. The process of diagnosing and managing allergic skin disease can be prolonged and frustrating for clients.
The guidelines offer recommendations and tips for client communication and when referral to a dermatologist should be
considered, to improve client satisfaction and optimize patient outcomes. (JAmAnimHospAssoc2023; 59:
䊏䊏䊏
–
䊏䊏䊏
.
DOI 10.5326/JAAHA-MS-7396)
AFFILIATIONS
Animal Dermatology Clinic, Louisville, Kentucky (J.M.); VCA Aurora
Animal Hospital, Aurora, Illinois (A.S.); Allergy, Skin and Ear Clinic for Pets,
Livonia, Michigan (P.B.); Animal Dermatology Clinic-Austin, Austin, Texas
(A.D.); Texas A&M University, College Station, Texas (A.F.); St. George’s
University, St. George’s, Grenada (T.P.); The Ohio State University,
Columbus, Ohio (M.W.); U-Vet Animal Clinic, Newburgh, Indiana (C-M.Y.)
CONTRIBUTING REVIEWERS
Lindsay McKay, DVM, DACVD, VCA Arboretum View Animal Hospital
Karen Trainor, DVM, MS, DACVP, Innovative Vet Path
Amelia White, DVM, MS, DACVD, Auburn University
Correspondence: [email protected]
†
J. Miller and A. Simpson are the cochairs of the AAHA Management
of Allergic Skin Diseases in Dogs and Cats Guidelines Task Force.
AAHA gratefully acknowledges the contribution of our task force
facilitator and writer, J.P. O’Connor, FASAE, in the preparation of this
manuscript.
These guidelines were prepared by a task force of experts convened by
the American Animal Hospital Association. This document is intended as
a guideline only, not an AAHA standard of care. These guidelines and
recommendations should not be construed as dictating an exclusive
protocol, course of treatment, or procedure. Variations in practice may
be warranted based on the needs of the individual patient, resources,
and limitations unique to each individual practice setting. Evidence-
guided support for specific recommendations has been cited whenever
possible and appropriate. Other recommendations are based on
practical clinical experience and a consensus of expert opinion. Further
research is needed to document some of these recommendations. Drug
approvals and labeling are current at the time of writing but may change
over time. Because each case is different, veterinarians must base their
decisions on the best available scientific evidence in conjunction with
their own knowledge and experience.
The 2023 AAHA Management of Allergic Skin Diseases in Dogs and
Cats Guidelines are generously supported by Hill’s Pet Nutrition Inc.,
Merck, and Zoetis.
AOE (allergic otitis externa); ASIT (allergen-specific immunotherapy);
DTM (dermatophyte test medium); FASS (feline atopic skin syndrome);
OTC (over the counter); PO (per os); SBF (superficial bacterial folliculitis);
SOC (spectrum of care)
Technician utilization
recommendation
Spectrum of care
recommendation
Referral
recommendation
© 2023 by American Animal Hospital Association JAAHA.ORG 1
VETERINARY PRACTICE GUIDELINES

Introduction
An itchy pet is one of the most common reasons a client seeks veter-
inary care. Allergic skin diseases can cause not only significant
discomfort and distress to the individual animal but also stress and
disruption to the pet’s family members. Because of the complex
nature of allergic skin disease, diagnosis can be time-consuming and
may require multiple follow-up visits before a final diagnosis is
achieved. Patients with allergic skin disease often require lifelong
management to optimize their quality of life. These guidelines offer a
step-by-step approach to diagnose and manage flea allergy, food
allergy, and atopy in the dog and cat.
Section 1 describes the steps in diagnosing the canine patient with
allergic skin disease.
Section 2 describes initial and long-term management of canine
allergic skin diseases and acute flares.
Section 3 addresses diagnosing allergy in the feline patient, including
clinical presentations of dermatitis in cats and key differences
between cats and dogs.
Section 4 describes initial and long-term management of feline aller-
gic skin diseases and acute flares.
Section 5 provides an overview of diagnosis and treatment of allergic
otitis externa.
Section 6 presents spectrum of care considerations for managing
allergic skin diseases, including referral recommendations, tele-
health, and communication tips.
Section 7 discusses the vital role of veterinary technicians in the
management of allergic patients and how to optimize their involve-
ment in these cases.
Section 8 offers key messaging points for client communication.
These guidelines are designed to simplify the path to diagnosis
and management of canine and feline allergic skin diseases, while
emphasizing a multimodal approach for the patient and effective cli-
ent communication to ensure the best possible outcome.
Section 1: Diagnosing the Allergic Canine
Patient
Top 3 Takeaways:
1. A detailed history, including a review of previous medical records,
should be obtained. Information regarding seasonality, pruritus
level, ectoparasite prevention, and response to previous therapies
are all paramount in the workup of the pruritic dog.
2. A minimum dermatologic database should be performed including
skin cytology, flea combing, skin scrapings, and ear cytology (if ear
disease is present).
3. Atopy is a diagnosis of exclusion. Allergy testing (intradermal or
serum) to identify allergens should only be performed if immuno-
therapy is planned.
Overview
Diagnosing allergic skin disease in the canine patient requires the
veterinary team to be well versed in obtaining accurate clinical histo-
ries that include key questions about the dog’s level of pruritus, the
environment, and any other medical conditions present. A minimum
dermatologic database should also be performed on pruritic patients
to assess for the presence of ectoparasites and skin infections.
Because atopy is a diagnosis of exclusion, the process may be time-
consuming and frustrating for clients. Clear communication regard-
ing timelines and expectations is crucial for successful results.
Step One: Clinical History and Dermatologic Physical
Examination
Clinical History
A detailed history should provide essential information about the
dog’s clinical signs, patterns of pruritus, and environment, which will
assist the practitioner in diagnosing the specific allergic disease.
When asking a client about the presence and intensity of pruritus, it
is important to clearly explain the signs of pruritus to owners who
may not readily recognize them. Clients may not understand that
scratching, biting, chewing, licking, gnawing, rubbing, or rolling can
all be evidence of an itchy dog. Pruritus scales (usually ranging from
1to10with10representingconstantitching)canbeahelpfultool
to use with clients. The validated canine Pruritus Visual Analog Scale
can be found at https://www.vetdermclinic.com/pruritus-visual-analog-
scale-canine/.
Educating clients and helping them to understand that each
question in the client history provides significant diagnostic clues
can make the process seem less of a formality and more like progress
toward the mutual goal of a more comfortable and happier dog.
Engaging clients in this way can create the sense that everyone is on
the same team, for what may be a long road ahead.
Veterinary technicians are an invaluable asset in
dermatologic appointments. From taking compre-
hensive clinical histories to educating clients, tech-
nicians serve a vital role in the workup and suc-
cessful management of pruritic patients.
Key Questions for Clinical History
1. What was the distribution of the pruritus initially? What is it now?
Have there been changes?
Note that only ectoparasites have a predictable distribution. The dis-
tribution of pruritus for atopy or food allergy is identical.
1
2. Is the pruritus seasonal, year-round, or year-round with a seasonal
flare?
Seasonal pruritus is most consistent with atopy. Year-round pruri-
tus may be associated with food allergy, atopy due to indoor aller-
gens, and atopy in certain geographical locations where outdoor
allergens lack seasonality.
3. What was the age of onset?
Food allergies may start at any age, but because atopy has a more
defined age of onset (i.e., clinical signs starting between 6 mo and
4yrofage),foodallergymaybeprioritizedintheveryyoungand
older patients.
2
Pruritus due to ectoparasites may present at any age.
2 JAAHA | 59:6 Nov/Dec 2023

4. What previous treatments were prescribed and how effective were they?
Response to treatments such as oclacitinib or lokivetmab will vary
among allergic patients. Response to glucocorticoids does not help
narrow the cause of pruritus as any pruritic disease may respond
to antipruritic doses of glucocorticoids. Failure to respond to gluco-
corticoids, however, may suggest the presence of secondary infections
(bacterial or Malassezia), ectoparasites, and/or food allergy. In addi-
tion, an incomplete response to antibiotic therapy may indicate the
presence of antimicrobial resistance. Commonly, antimicrobials and
antipruritic therapies are prescribed and discontinued at the same
time. To truly assess response to these therapies, it is helpful to avoid
discontinuat ion of these medications at the same time.
Complete response Partial response No response
Consider food
allergy concurrent
with atopy. Continue
diet trial while
treating for atopy.
Pruritus when diet
is challenged
Treat for atopy,
recheck MDB.
Ectoparasites were cleared vs seasonal atopy vs resolution
of secondary skin infections due to primary endocrinopathy
Nonseasonal Seasonal
Complete response AND
no return of pruritus after
medications stopped
Food allergy
Continue
hypoallergenic diet
Treat for atopy
Partial or no response OR return of pruritus after medications stopped
Presentation of dog:
Skin lesions +/- pruritus
STEP 1: Clinical History and Dermatologic
Physical Examination (skin AND ears)
STEP 3: Treat Pruritus (+/- oral glucocorticoid, oclacitinib, or lokivetmab, depending on severity)
STEP 4: Treat Secondary Infections, Ectoparasites, and OE
STEP 5: Recheck
STEP 6: Diet Trial
STEP 2: MDB (skin scraping,
skin cytology, +/- ear cytology)
MDB, minimum dermatologic database; OE, otitis externa
FIGURE 1
Diagnosing Allergic Skin Disease in the Canine Patient.
JAAHA.ORG 3

5. Are other pets or humans affected?
Pruritus affecting other pets or humans strongly suggests the pres-
ence of ectoparasites such as fleas, scabies, or Cheyletiella.
6. Is there any vomiting, soft stool, or increased flatulence that may sug-
gest a food allergy?
In addition to cutaneous signs, 19–27% of food-allergic dogs will
also exhibit vomiting, soft stool, and/or diarrhea.
3
Using a fecal score
chart can be beneficial (see https://www.proplanveterinarydiets.ca/
sites/g/files/2021-02/180107_PPPVD-Fecal-Scoring-Chart-UPDATE-
EN-FINAL.pdf).
Dermatologic Physical Examination
Perform a complete physical examination, including flea combing and
an otoscopic examination. An otoscopic examination should be per-
formed even if the owner does not report otic pruritus because it is
common for dogs to not show overt clinical signs of ear disease until
it is moderately severe. Note that up to 50% of allergic dogs may have
otitis externa
1
and this may be the first and only clinical signs of aller-
gicdisease.Besuretoassesstheskininareaswhereinflammatio n
may be less obvious, including the paws, claws, perianal skin, and
intertrigi nous areas such as the axillary and inguinal regions and skin
folds (see Figure 2). A complete nose-to-tail examination is essential
and may require sedation if an animal is very uncomfortabl e or resis-
tant to handling.
Flea combing should always be performed as part of
the initial physical examination.
Step Two: Minimum Dermatologic Database
A minimum dermatologic database should be collected as the next
step and consists of the following:
Cytology of skin and ears (where evidence of ear disease is present)
Skin scrapings (deep/superficial to assess for both Demodex and Sar-
coptes mites)
If there are financial constraints, consider a thera-
peutic trial with an isoxazoline, rather than per-
forming skin scrapings. However, be aware that
although uncommon, failures in the treatment of
mites using isoxazolines have been anecdotally
reported. A s alternatives to traditional deep skin
scrapings, plucking hairs (trichogram) or acetate
tape samples on pinched skin may be able to detect
Demodex mites in areas that are too sensitive for a
deep skin scrape.
6 Dermatophyte test medium (DTM) culture (depending on regional
prevalence, history, and index of suspicion)
Depending on state regulations, collecting samples
for a minimum dermatologic database may be
assigned to a veterinary technician.
Step Three: Treat Pruritus
A critical aspect in managing both the patient and the owner’squal-
ity of life is reducing pruritus. Consider the use of an antipruritic
agent (glucocorticoids, oclacitinib, or lokivetmab) and/or topical
therapy (see Table 1 and Section 2 for more information). These
therapies may be less effective in the face of active infection; there-
fore, appropriate diagnosis and treatment of secondary infections is
critical before assessing response to antipruritic therapy.
Step Four: Treat Secondary Infections and
Ectoparasites
Secondary bacterial and Malassezia infections must be treated con-
currently with controlling pruritus and diagnosing the underlying
allergic disease (see Tables 4 and 5). Otitis externa, if present, should
also be treated (see Section 5). Prescribe a flea and tick preventive if
the dog is not currently receiving one and discuss compliance with
the client. The guidelines task force prefers an oral isoxazoline as
this drug class offers flea, tick, and mite prevention and allows for
routine bathing. All parasiticides may lower seizure threshold, and
consultation with a neurologist is recommended in severely epileptic
patients.
Step Five: Recheck, Verify Medication, and Assess
Response to Treatment
Assessing the response to medications such as flea preventives and
antipruritic drugs is a key step in the diagnostic process. It is impor-
tant to ensure that the veterinary team and the client are all on the
same page about medication administration, duration of therapy,
and follow-up examinations. Response to therapy should be assessed
14 days after initiating therapy, and this is ideally done with an
in-person recheck examination. However, if a physical examination
is not feasible for the client, this would be a reasonable application
for a telehealth appointment. If multiple medications were pre-
scribed, it is recommended to discontinue these one at a time to help
determinewhich,ifany,wereresponsiblefortheresponse.Itisnot
ideal to stop antipruritic and antimicrobial therapies at the same
time as this muddies the water and does not allow you to inter-
pret what was causing the patient’sitch—the infection or the
allergic inflammation.
If the dog shows a full response to treatment (i.e., resolution of
pruritus, resolution of infection, skin lesions, etc.) after being weaned
off antipruritic therapy at the time of reassessment:
1. The diagnosis may be one of three things: ectoparasitism that has
now resolved, secondary infections that have now resolved, and/or
seasonal atopy.
4 JAAHA | 59:6 Nov/Dec 2023

FIGURE 2
Clinical Presentation of the Pruritic Canine Patient.
JAAHA.ORG 5

2. If a secondary infection was present, it may have been the
primary cause of the pruritus. Primary diagnoses to consider then
include:
a. Ectoparasites
b. Seasonal atopy
c. Endocrinopathy
i. If other clinical signs are present
ii. Note that these conditions are not pruritic unless secondary
infection is present
Next Steps
1. Continue routine use of flea/tick preventives.
2. If receiving antimicrobial therapy and the infection has resolved,
continue antimicrobial therapy for 7 days beyond clinical and cyto-
logical resolution (see Section 2 for more information).
3. If the history supports seasonal atopy, discuss management options
(see Section 2).
4. If the history supports an endocrinopathy, recommend additional
diagnostics.
TABLE 1
Antipruritic and Anti-inflammatory Medications for Dogs
Drug Name Oclacitinib
1
Lokivetmab
2
Cyclosporine
3
Glucocorticoids
4
Mode of action JAK-STAT inhibitor that
blocks signaling from
proinflammatory and
pruritogenic cytokines
Caninized monoclonal
antibody that
neutralizes the
pruritogenic cytokine
IL-31
Calcinurin inhibitor
that modulates T-cell
function
Influences gene
expression of
proinflammatory
cytokines
Administration PO
q 12 hr up to 14 days,
then reduce to q 24 hr
SC injection at
veterinary oce
q 4-8 wk
PO
q 24 hr
PO
q 12-24 hr with taper
Injectable not
recommended
Time to onset Hours Hours to 3 days 4-6 wk Hours
Age >1 yr Any >6 mo Any
Weight >3 kg Any >1.8 kg Any
Health restrictions History of demodicosis
History of neoplasia
Serious infection
None History of neoplasia
Renal insuciency
Congestive heart
failure
Diabetes mellitus
Hyperadrenocorticism
Hypertension
Adverse reactions Vomiting
Diarrhea
Nonspecific dermal
masses
Demodicosis
Pyoderma
Vomiting
Diarrhea
Lethargy
Pain at injection site
Rare: Hypersensitivity
eects (urticaria, facial
edema, anaphylaxis)
Vomiting
Diarrhea
Gingival hyperplasia
Hirsutism
Cutaneous
papillomatosis
Drug interactions
Polyuria/polydipsia
Polyphagia
Panting
Obesity
Muscle wasting
Iatrogenic
hyperadrenocorticism
Congestive heart
failure
JAK-STAT, Janus kinase signal transducers and activators of transcription; PO, orally; SC, subcutaneously.
1 Apoquel (oclacitinib tablet). Package insert. Zoetis, 2020.
2 Cytopoint. Package insert. Zoetis, 2015.
3 Atopica (cyclosporine capsules). Package insert. Elanco, 2020.
4 Saridomichelakis MN, Olivry T. An update on the treatment of canine atopic dermatitis. The Vet Jour. 2016;207:29–37.
6 JAAHA | 59:6 Nov/Dec 2023

5. If there is no history of previous skin or ear disease or an uncertain
history, propose observing for recurrence, but also discuss the possi-
bility of a future diagnosis of allergic disease.
If the dog is showing partial or no response while on an appro-
priate antipruritic agent:
1. Repeat cytology.
2. If evidence of bacterial infection is present (Figure 3) and a systemic
antibiotic has already been used:
a. Perform an aerobic bacterial culture and withhold systemic anti-
biotics pending culture and susceptibility results.
b. Choosing a second antibiotic empirically is strongly discouraged
owing to the risk of increasing incidence of antimicrobial drug
resistance. The cost of using the wrong antibiotic can exceed the
cost of culture.
c. If you MUST choose a second antibiotic, be sure to change the
class of antibiotic (e.g., do not change from one beta lactam anti-
biotic to another). See Table 4 for guidance on choosing first-
and second-tier antibiotics.
3. Discuss the owner’s ability to increase the frequency of topical anti-
microbial treatment—often, more intense topical treatment elimi-
nates the need for systemic antibiotics.
4
4. If Malassezia yeasts are identified cytologically from lesioned skin
(Figure 3), then antifungal treatment should be initiated topically
and/or systemically based on clinician discretion. The number of
Malassezia yeasts noted cytologically does not necessarily correlate
with the severity of the disease.
Addressing Malassezia is imperative, especially in individuals with a
hypersensitivity response to these organisms, which in turn worsens
clinical signs.
5
5. If lesions and/or infections have resolved but pruritus persists, the
dog has either atopy or food allergy.
a. Treatment for allergic skin disease is individualized for THIS
dog and THIS client.
b. In general, food allergy is less steroid responsive than atopy.
1
c. If a diet trial is not possible (e.g., the client is not able to comply
or the environment of the dog is not conducive), then symptom-
atic treatment for atopy should be initiated and response to ther-
apy should be assessed.
The guidelines task force acknowledges that a properly
performed diet trial is difficult to conduct and client
compliance can be challenging. The task force recom-
mends considering a consultation with or referral to a
veterinary dermato logist before beginning a diet trial.
Step Six: Diet Trial
Because there are no historical or physical examination findings that
can differentiate atopy from food allergy, a diet trial is an important
step in the diagnostic process. Other than the seasonality associated
with atopy, a higher incidence of gastrointestinal signs in food-allergic
animals, and the possibility that the pruritus may be less steroid
responsive in food-allergic dogs, there are no differences between the
diseases. The previously held observation that an “ears and rears”
pruritic pattern indicates a food allergy is no longer accurate.
1
Serum
tests, saliva tests, and hair tests are of no value in the diagnosis and
management of food allergy.
1,6
FIGURE 3
Cytology of Secondary Bacterial and Yeast Infections.
JAAHA.ORG 7

Diet trials should be conducted for 4–12 wk and a food chal-
lenge performed to confirm the diagnosis of food allergy if there is a
positive response. Recent studies show that a fair number of food-
allergic dogs may respond to strict prescription diet trials in 30 days,
however, 8 weeks may be needed to capture a diagnosis in .90% of
food-allergic dogs, and there is a small subset of dogs that may
require 12 weeks for complete resolution of pruritus.
7,8,9
Antipruritic treatment is frequently needed to give relief during
the initial stage of the diet trial. The guidelines task force considers
glucocorticoids or oclacitinib to be appropriate choices to control
pruritus. If a client is unable to give oral medication during the diet
trial, lokivetmab can be considered as an alternative; however,
because of the long-acting nature of this injection, the diet trial must
be extended more than 60 days to allow for individual variation in
duration of action. The exact length of time a diet trial must be
extended is not known, and for this reason, the task force does not
recommend using lokivetmab during diet trials unless absolutely
necessary—for example, in a young, growing puppy where glucocor-
ticoids are not ideal and oclacitinib is off label.
Diet Choices
Numerous prescription hydrolyzed or novel protein diets are available
in a multitude of formulations, and the option to home cook a highly
limited-ingredient novel protein diet is also available. Although home-
cooked diets potentially offer the strictest formulation, it may be
impractical for many clients in terms of labor and cost of ingredients.
The choice of diet will depend on the dog’s clinical and diet history,
the dog’s dietary preferences, and the owner’s financial constraints.
At present, there is no one-size-fits-all diet that is appropriate for
all patients. Prescription veterinary diets, compared with over-the-
counter (OTC) diets, are less likely to contain unidentified protein
sources
10
and therefore are the only acceptable commercial diet
choices for a true elimination diet trial.
Use of OTC diets should not be recommended
when conducting a diet trial. Ingredients not declared
on the label have been detected in OTC diets, possibly
negating the results of the trial.
11
Howeve r, the guide-
lines task force agrees that an OTC novel protein diet
can be used if financial constraints make other diets
impossible. The client should be warned that an OTC
diet may not provide optimal results and should be
considered a diet change, not a true diet trial.
During the diet trial, monthly oral flavored heartworm and flea
and tick preventives should be avoided. Topical or long-lasting isoxa-
zolines administered at the very beginning of a diet trial along with
topical or injectable heartworm preventives should be considered. It
is imperative to explain that the chosen diet must be the only thing
Recheck skin cytology—if
no indication of yeast
and/or bacterial infection
secondary to the diet
challenge, then the dog
does not have food
allergy. Consider atopy.
Return to the
elimination diet.
May require restarting
antipruritic therapy for 1-2
wk, then discontinuing to
evaluate response
Food allergy is ruled
OUT, consider atopy
Dog has food allergy
Food allergy is ruled
OUT, consider atopy
Did the pruritus return
within 14 days?
Did the pruritus
resolve within 14 days?
YES
Discontinue antipruritic therapy at wk 2–3 of trial,
then recheck and reassess pruritus at 4 wk
Resume antipruritic
therapy for 2-3 wk
and continue the diet
for an additional 4 wk
Perform a food
challenge by
reintroducing the dog’s
previous diet
Is dog pruritic?
YES NO
NO
YES
YES
NO
Discontinue
antipruritic therapy
again while
maintaining strict diet
Is dog pruritic?
NO
FIGURE 4
Assessing Diet Trial Results.
8 JAAHA | 59:6 Nov/Dec 2023

to “pass the lips” of the dog during the 4 to 12 wk trial. This includes
pill pockets, treats, flavored toys, cat food or feces, shared water
bowls, table scraps, etc.
Veterinary technicians can play an important role in
discussing the choice of an appropriate diet with own-
ers, as well as addressing any questions regarding com-
pliance with the trial diet. A follow-up call 2–3wkinto
the diet trial can be beneficial and allows the veteri-
nary team to address any challeng es or client concer ns.
Assessing a Diet Trial
The finalstepinperformingadiettrialistochallengethepatientby
reintroducing the original diet. This is essential in patients that have
responded well to the diet trial and is the sole means of confirming a
diagnosis of food allergy. Misdi agnosi s can result in unnecess ary
expense to the owner (due to long-term use of expensive therapeutic
diets) and the potential for ongoing dermatologic problems (due to
missed diagnosis of seasonal atopy or other pruritic condition).
Figure 4 illustrates the steps of assessing a diet trial.
Remember that a properly performed diet trial is
time-consuming for the veterinarian and client to
manage, and a discussion of a referral to a veteri-
nary dermatologist should be brought up with the
client and considered.
Seasonal or Nonseasonal with Seasonal
Fluctuation (Atopy)
Because atopy is a diagnosis of exclusion, if the dog is on an appropriate
treatment for ectoparasites and a food allergy has not been demon-
strated, then a diagnosis of atopy has been established. Intradermal and
serum allergy testing are NOT used to diagnose atopy. It should only be
used if the client is interested in administering allergy immunotherapy.
Section 2: Treating the Allergic Canine Patient
Top 3 Takeaways:
1. Treating the allergic dog is not one-size-fits-all, and a multimodal
approach often yields the best results.
2. Client education, communication, and compliance is critical in the
success of any treatment plan.
3. If previously successful management protocols stop working, first
perform a thorough history and physical examination and return to
the minimum dermatologic database to determine whether anything
has changed.
Overview
The clinical management of the allergic canine patient is often
viewed as frustrating by veterinarians and clients alike, as there is no
one-size-fits-all treatment. In addition to the need to manage second-
ary infections, inflammatory flares, and individual patient responses,
veterinary teams must consider client compliance, finances, and
other factors like time availability and access to transportation.
Atopic patients need lifelong medical care that will require routine
veterinary visits and an active working relationship with the client.
Tailoring a communication-rich, multimodal approach for each indi-
vidual patient will provide the best path to success.
Flea Allergy
Flea allergy dermatitis is one of the most common causes of pruritus
in canine patients, and successful management relies on a three-
tiered approach.
Step One: Choose the appropriate preventive.
Preventives that have potent adulticide activity should be used. Isoxa-
zolines are now widely considered the gold standard in prevention
and are recommended for initial consideration. It has been demon-
strated in recent years that dogs with flea allergy dermatitis may be
successfully managed with the routine administration of an oral iso-
xazoline.
12
The effectiveness of the preventive chosen is closely tied
to accurate application of the product.
Step Two: Use the preventive year-round in all
in-contact animals.
Step Three: Treat the environment in severe
infestation situations.
Food Allergy
Avoiding all offending allergens, based on the diet challenge trials, is
the goal for patients and clients. Here the client has two options: a
veterinary prescription diet or OTC food.
An unfortunate consequence of maintaining a patient on a pre-
scription diet is the potential for backorders. Consider other prescrip-
tion diets that avoid the offending allergen or have similar ingredients.
Pet food companies can provide excellent technical support and may
have additional recommendations. A helpful tip is to have clients keep
extra dog food bags on hand to avoid temporary backorder issues.
For some patients, control may be maintained by feeding an OTC
diet that does not claim to contain the offending allergen. In a small sub-
set of dogs, however, their severe sensitivity prohibits the use of OTC
diets because of potential contamination with unlabeled proteins.
10,13
If a flare occurs in a patient on an OTC diet, inquire whether
they were fed from a new bag of food as the formulation may have
changed or the batch may contain unlabeled proteins. Investigate
whether they are now displaying clinical signs of atopy in conjunc-
tion with food allergy and consider ectoparasites, as they are the
leading cause for acute-onset pruritus.
JAAHA.ORG 9

Atopy
Initial Management
When choosing a management protocol, the clinician must take into
consideration the level of inflammation and pruritus present and
whether any secondary infections are present. If a patient is 10/10
pruritic with severely inflamed skin, a glucocorticoid may offer an effec-
tive initial treatment and a short course may effectively manage a single
atopic episode. Many veterinary dermatologists would recommend the
use of glucocorticoids over oclacitinib in severely inflamed skin; how-
ever, there is evidence to show that oclacitinib can have the same anti-
inflammatory benefits as prednisolone in certain cases.
14
Lokivetmab
maybeanappropriatechoicewheninflammation is less severe.
For mild to moderate inflammation and pruritus, oclacitinib
and/or lokivetmab (see Table 1 and Table 2) may be administered.
Multiple factors should be considered when choosing one of these
drugs as neither medication is 100% effective, and there is significan t
variation in individual patient response.
15,16
Oclacitinib is more effec-
tive in some patients, and lokivetmab is more effective in others.
17
If the patient is presenting for extremely mild clinical signs, an
antihistamine (see Table 3) trial may be appropriate; however, it is
imperative to remember that antihistamines are best used as preven-
tive medicine, do not perform well as monotherapy, and are not
effective in treating moderate to severe inflammation or pruritus.
18,19
Long-term Management
A multimodal approach can promote successful long-term manage-
ment, but it will take patience while assessing which option works
for each patient.
If adequate control of clinical signs cannot be
achieved by the third veterinary visit, then referral
to a veterinary dermatologist should be presented
as an option to the owner
49
to provide more effec-
tive treatment and less cost to the client in the long
run. Referral could be discussed even earlier, but
this may not always be necessary. Availability to be
evaluated by a veterinary dermatologist could be
markedly delayed in certain geographic areas, in
which case more acute management by a general
practitioner would be needed.
If the veterinary team moves forward with treatment, the fol-
lowing steps are recommended.
1. Continue antipruritic/anti-inflammatory therapy and use routinely
in a preventive manner. If oclacitinib and lokivetmab have been
found ineffective, cyclosporine may be considered, with the under-
standing that it will take 4–6 wk to be maximally effective.
19
Some patients are glucocorticoid-responsive-only
and/or some clients cannot afford other treat-
ments; therefore, chronic management with gluco-
corticoids may be appropriate. A thorough discussion
of the potential long-term side effects and recom-
mended monitoring must take place.
2. Consider adjunctive therapies such as veterinary-formulated essen-
tial fatty acid supplementation, specially formulated dermatologic
diets, nutraceuticals, palmitoylethanolamide, probiotics, and pro-
ducts aimed at improving epidermal barrier dysfunction. These are
all excellent options to consider in atopic patients.
15
3. Topical therapy: routine bathing using shampoos with moisturizing
factors (i.e., fatty acids, oatmeal, ceramides, and lipids) can be help-
ful as adjunctive therapy. Particularly with dogs experiencing recur-
rent bacterial pyoderma and/or Malassezia dermatitis, anti-infective
shampoos, mousses, or sprays can be used routinely to help reduce
the recurrence of secondary infections.
4. Allergen-specific immunotherapy (ASIT) is a safe, drug-free treat-
ment that is effective in 50–100% of canine patients.
21
Clinical
benefit may not appear for up to a year, and routine antipruritic/
anti-inflammatory management will be required in the interim.
19
Successful ASIT protocols again require diligent, educated clients
who recognize that it is not a quick fix.
For allergy testing and ASIT management, referral
to a veterinary dermatologist is highly recommended
as tailoring individual protocols increases positive
response rates.
22
The preferred method of testing,
whether intradermal allergy testing or serum allergy
testing, is highly controversial and has not yet been
established in the literature.
23
Injectable immuno-
therapy is considered the standard; however, sublin-
gual immunotherapy has also been shown to be
effective.
24,25
Management of Acute Flares
All atopic dogs will experience allergic flares regardless of how well
managedtheyare.Whenaflare occurs, collect a thorough history
and a minimum dermatologic database to determine whether there
have been any changes in the patient’s lifestyle. Look for evidence of
ectoparasitism or secondary infections. If the flare is mild and sec-
ondary issues have been identified, managing the secondary issues
should resolve the increased pruritus.
If the inflammatory flare is severe, the addition of a short
course of glucocorti coids may be ben eficial in regaining control.
If glucocorticoids are contraindicated, administering twice-daily
oclacitinib for a limited time (e.g., up to 14 days) or adding loki-
vetmab may be appropria te. Cycl osporine is not appropriate for
an acute flare.
Acute Flare Factors
•
Secondary infections
•
Ectoparasites (fleas/mites)
•
Environmental/seasonal changes
•
Food challenges (holidays!)
10 JAAHA | 59:6 Nov/Dec 2023

TABLE 2
Acute Flare and Long-term Management Therapies in Dogs
JAAHA.ORG 11

Considerations in Treating Secondary Infections
When superficial bacterial folliculitis (SBF) is identified, there are
three guidelines to follow: correct antibiotic, correct dose, and cor-
rect duration.
4
Table 4 provides a tiered approach to appropriate
antibiotic choices including recommended doses for managing SBF.
The golden rule for duration of antibiotic therapy is 7 days past clini-
cal and cytologic resolution.
26
As such, the current recommended
course for oral antibiotics in treating SBF is typically 21 days.
Topical therapy is an integral part of managing SBF, and many
infections will resolve with topical therapy alone.
27,28
As this requires
advanced client compliance, prescribing more user-friendly formulations
(spot-ons, sprays, or mousses) may encourage more effective usage.
Topical antimicrobial therapy also acts as an excellent adjunctive
therapy to oral antibiotics.
TABLE 3
Oral Antihistamine Doses for Dogs
Drug Name Dose
Hydroxyzine 2 mg/kg q 12 hr
1
Cetirizine 1–2 mg/kg q 24 hr
1
Chlorpheniramine 0.4 mg/kg q 12 hr
2
Cyproheptadine 0.3–2 mg/kg q 12 hr
2
Clemastine 0.05–1 mg/kg q 12 hr
2
Loratadine 1 mg/kg q 12 hr
2
Fexofenadine 5–15 mg/kg q 24 hr
3
Amitriptyline 1–2 mg/kg q 12 hr
2
Diphenhydramine 2–3 mg/kg q 12 hr
2
4
1 Bizikova P, Papich MG, Olivry T. Hydroxyzine and cetirizine
pharmacokinetics and pharmacodynamics after oral and
intravenous administration of hydroxyzine to healthy dogs. Vet
Dermatol. 2008;19:348–57.
2
Muller & Kirk’s Small Animal
Dermatology. 7th ed. St. Louis:Elsevier;2013.
3
antihistamine fexofenadine versus methylprednisolone in the
treatment of atopic dermatitis in dogs. Slov Vet Res. 2009;46:5–12.
4
and cetirizine on immediate and late-phase cutaneous allergic
reactions in healthy dogs: a randomized, double-blinded
crossover study. Vet Dermatol. 2020;31:256–e58.
TABLE 4
Antimicrobials for Skin Infections in Dogs
1
*
12 JAAHA | 59:6 Nov/Dec 2023

Malassezia dermatitis is a common flare factor and may dra-
matically increase pruritus in atopic dogs. In many cases, appropriate
treatment for Malassezia significantly increases the effectiveness of
antipruritic/anti-inflammatory therapy. Topical treatment for Malas-
sezia may be useful, however, some cases of deep or chronic Malasse-
zia dermatitis (such as Malassezia in the claw folds or in severely
lichenified skin) necessitate oral antifun gal therapy with
ketoconazole, fluconazole, itraconazole, or terbinafine (Table 5). The
golden rule of 7 days past clinical and cytologi c resolution applies
here, too.
Section 3: Diagnosing the Feline Patient
Top 3 Takeaways:
1. Cats, unlike dogs, have a more varied clinical presentation of aller-
gic dermatitis, including scratching, overgrooming, and several
cutaneous inflammatory reaction patterns.
2. Treating all pruritic cats for fleas/mites is not only a potentially
important therapeutic measure but also a key diagnostic step on the
path to determining the primary cause of pruritus.
3. There are no accurate allergy tests for diagnosing feline atopic skin
syndrome (environmental allergies) in cats. This diagnosis is deter-
mined through diligently ruling out all other causes of pruritus.
Overview
Compared with dogs, the pathogenesis of skin diseases in cats is not
as well understood. Recently, there has been a resurgence in investi-
gation for this species and attempts to clarify and classify the feline
allergic profile.
Feline atopic syndrome has been proposed as the umbrella
nomenclature describing allergic dermatitis involving environmental
allergens, food allergy (gastrointestinal manifestation), and allergic
asthmas (respiratory disease) often associated with immunoglobulin
E antibodies. Feline atopic skin syndrome (FASS) refers to the entity
associated with inflammatory and pruritic allergic skin disease from
environmental allergens.
29
Presentation of the Feline Patient
Four distinct clinical patterns of allergic dermatitis have been
described in the cat: miliary dermatitis, head and neck pruritus, self-
induced alopecia, and eosinophilic granuloma complex (eosinophilic
plaques, granulomas, and indolent ulcers) (see Figure 5). Pruritus,
from mild to severe, is typically present in cats with allergic dermatitis,
whether due to food allergy, flea allergy, and/or FASS (environmental
allergies). Exceptions include indolent ulcers or eosinophilic granulo-
mas, which can occur without pruritus.
30
None of the feline cutaneous reaction patterns are pathogno-
monic for any particular pruritic disease, emphasizing the need to
perform a thorough diagnostic workup,
31
including an accurate clini-
cal history, dermatologic physical examination, and a minimum der-
matologic database. Atypical or non–treatment-responsive lesions
mayrequireaskinbiopsyfordefinitive diagnosis.
Step One: Clinical History and Dermatologic Physical
Examination
Clinical History
When inquiring about the presence and intensity of pruritus in
the cat, it is important to educate the client that feline pruritus can
manifest as scratching (head, neck, ears) with the hind paws and/or
overgrooming (licking/biting/chewing) of specific areas such as the
ventral abdomen, lumbar region, tail, and along the front and hind
limbs. In addition, clients should know that some cats are “closet
groomers” and may engage in overgrooming when clients are not
directly supervising them. A trichogram demonstrating sharply bro-
ken hair shafts is an excellent way to confirm self-trauma as the
cause of hair loss. A validated scoring method for pruritus has been
published recently for cats,
30
which provides the client with detailed
direction on ranking both scratching and licking behaviors by mark-
ing responses along a series of descriptions. This should be used at
the initial appointment and then at each subsequent appointment
after starting ectoparasite treatment, an elimination diet trial, courses
of glucocorticoids, or long-term therapies for FASS (i.e., allergy
immunotherapy or cyclosporine).
Having technicians take the history is an excellent
way for them to build client trust and relationships
that can carry through treatment follow-ups, client
education, and ongoing control measures.
TABLE 5
Oral Antifungal Medication Doses for Dogs
JAAHA.ORG 13

FIGURE 5
Clinical Presentation of the Pruritic Feline Patient.
14 JAAHA | 59:6 Nov/Dec 2023
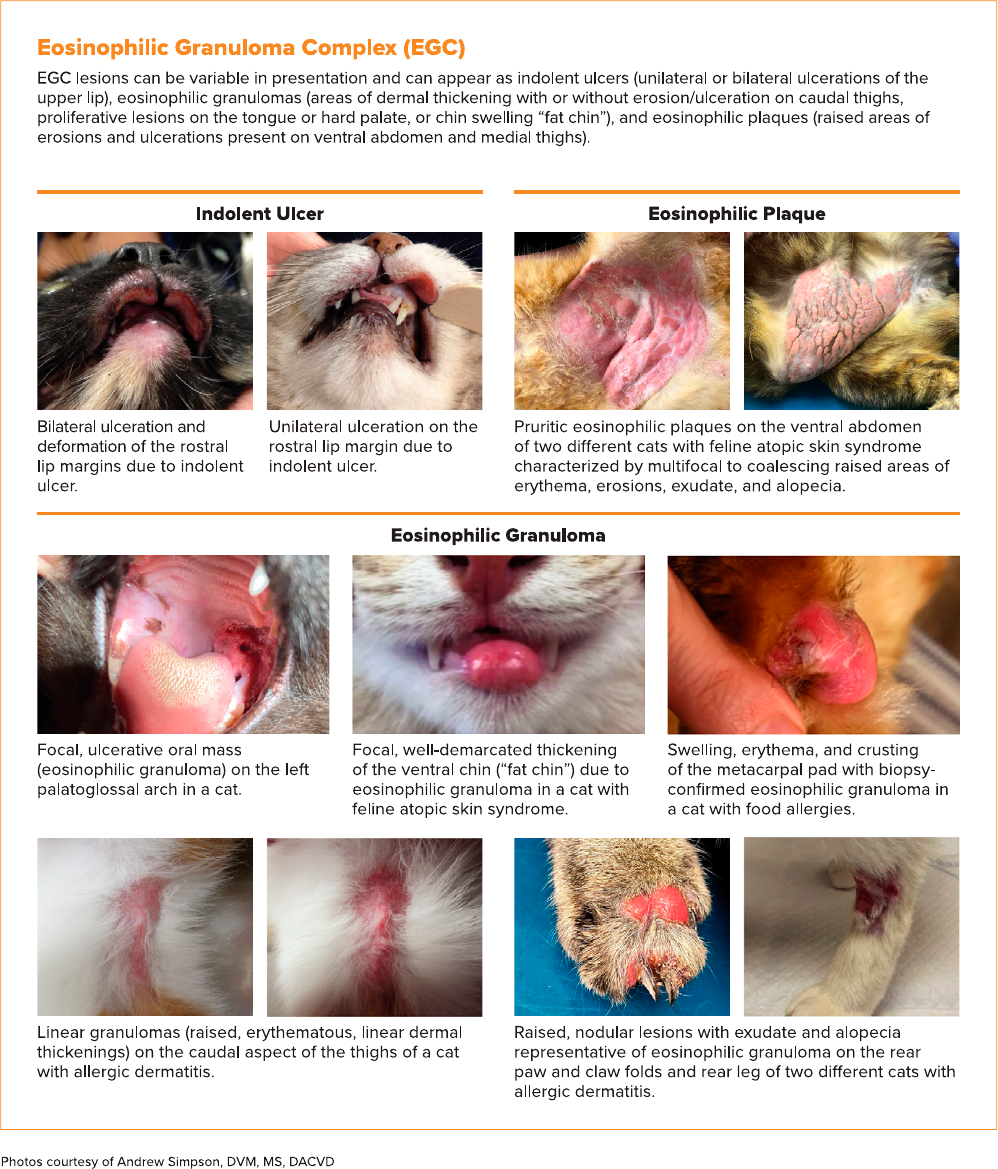
FIGURE 5
Continued.
JAAHA.ORG 15

Key Clinical History Questions
1. At what age did the pruritus start?
2. Is it seasonal?
3. Are other cats or dogs in the house itchy?
4. How much time is spent indoors versus outdoors?
5. Was the cat recently housed in a shelter/cattery/boarding facility?
6. Has there been any exposure to new or stray cats?
7. How often is ectoparasite control applied?
8. Has there been a response to other treatments, including antibiotics
or antipruritic medications?
9. What previous diagnostic tests have been performed?
Dermatologic Physical Examination
Evaluation should include the most commonly affected areas includ-
ing the head, neck, and ventral abdomen; however, any area of
haired skin could potentially be involved, such as along the dorsum,
sternum, axillae, medial thighs, forelimbs/hindlimbs, paws, perineum,
and tail.
31
The oral cavity should be examined to look for granulomas
of the tongue/palate and indolent ulcers of the upper lip. Flea comb-
ing is a crucial part of the examination to identify live fleas and/or
flea dirt to support a diagnosis of a flea infestation or allergy.
Otitis externa can occur in 20% of cats with feline atopic skin
syndrome,
31,32
but it can also occur in cats with food allergy. Evalua-
tion of the pinnae and otoscopic examination of the ear canals is an
integral part of the complete dermatologic examination.
Step Two: Minimum Dermatologic Database
The minimum dermatologic database should be collected based on
reaction patterns (Figure 6).
Cytology of skin and ear (if evidence of ear disease is present).
Superficial bacterial skin infections and Malassezia infections can be
present with all cutaneous reaction patterns, and thus, all skin
lesions on the cat should be sampled for secondary infection, placing
this diagnostic higher on the priority list. The exception to this
rule would be self-induced alopecia without overt evidence of cuta-
neous inflammation, as alopecia alone is not as likely to harbor
infection.
Superficial and deep skin scrapings. Ideal in all cases of pruritic
skin disease in cats to potentially provide a definitive diagnosis.
When broad-spectrum ectoparasiticides are used (i.e., isoxazolines),
keep in mind that treatment failures could still occur.
6 DTM culture. Considering that pruritus is typically minimal to
absent in most cases of dermatophytosis,
33
performing a fungal
culture (DTM) and/or dermatophyte polymerase chain reaction
test may not be necessary in all cases of cats with cutaneous reac-
tion patterns. This reflects the majority opinion of the guidelines
task force; however, not all members agreed on the overall ranking
of screening for dermatophytosis. One task force member felt that
although dermatophytosis is not t ypically pruritic (or at least
not severely), it should be ranked higher on the differe ntial list
because of its likelihoo d of occurrence. Consider ation of dermato-
phytosis may rank higher on the differential list under certain
circum stances, including indoor/outdoor cats, recently adopted
kittens, older immunocompromised cats, and Persians and other
long-h aired felines. In some cases, such as miliary d ermatitis and
self-induced alopec ia, DTM 6 de rmatophyte polymerase chain
reaction test may be more highly considered if parasites have been
ruled out.
Skin scrapings and otic preparations for mites
could be prioritized lower on the list with cost-
concerned clients, as pruritic mites are already
likely being treated if isoxazolines have been
prescribed.
Step Three: Treat Pruritus During the
Diagnostic Period
Many itchy cats require glucocorticoids because of their rapid and
reliable benefits for immediate treatment, especially when moder-
ate to severe pruritus and/or inflammatory lesions are present.
34
Antihistamines are not as reliable at controlling itch
35
and do not
have enough anti-inflammatory properties to reduce severely
inflamed lesions. Cyclosporine, although effective for long-term
treatment, does not typically provide immediate relief from
pruritus.
It is recommended to consider oral glucocorticoids (predniso-
lone 2 mg/kg/day, methylprednisolone 0.8–1.5 mg/kg/day,
34
or dexa-
methasone 0.2 mg/kg/day
26
tapered over a 3 wk period) rather than
injectable repositol glucocorticoids, given the inability to rapidly
withdraw the medication in the event of side effects (e.g., congestive
heart failure, diabetes, and skin fragility).
Step Four: Treat Ectoparasites and Secondary
Infections
Ectoparasite Treatment
It is essential to rule out external parasites (i.e., fleas and mites) in all
cases of feline pruritus with reliable parasite control measures. Dis-
cussion of all available flea treatment products is beyond the scope of
these guidelines; however, the guidelines task force generally recom-
mends the use of isoxazolines (fluralaner, sarolaner, and lotilaner)
owing to their relatively rapid flea adulticidal properties in addition
to off-label broad-spectrum ectoparasite coverage (i.e., Demodex cati,
Demodex gatoi,andOtodectes).
36–38
When reviewing the known or suspected clinical picture with
clients, it is important to discuss therapy durations. Be candid that
treating mites takes 6–8 wk on average, whereas a flea infestation
takes closer to 3 mo to treat under ideal conditions. Openly discuss-
ing client constraints (e.g., time, ability to comply, and finances) in
initial appointments will inform treatment choices and expectations
for the veterinary team and clients.
16 JAAHA | 59:6 Nov/Dec 2023

Complete response
after stopping
antipruritic medication
Assess for food allergy + maintain year-round flea preventives
FASS
STEP 5: Recheck/Assess Response to Antiparasitic/Antipruritic Treatment
STEP 4: Treat Ectoparasites and Secondary Infections
STEP 3: Treat Pruritus: oral glucocorticoids (prednisolone or methylprednisolone)
Flea allergy/mites or
seasonal FASS:
maintain year-round
flea preventives
Nonseasonal Seasonal
Food allergy
Consider food allergy concurrent
with FASS. Continue diet trial
while treating for FASS
Treat for FASS,
recheck MDB
Partial or no response after stopping antipruritic medication
Parasite treatment
Cytology
DTM
Skin scrape
Parasite treatment
DTM
Skin scrape
Parasite treatment
Ear cytology/mite treatment
Cytology
Skin scrape
DTM
Cytology
Parasite treatment
Presentation of cat:
Skin lesions +/- pruritus
STEP 1: Clinical History and
Dermatologic Physical Examination
Miliary Dermatitis Self-Induced Alopecia Head/Neck Pruritus Eosinophilic Lesions
STEP 2: MDB
Collect MDB based on reaction patterns (in order of priority)
DTM, dermatophyte test medium; FASS,
feline atopic skin syndrome; MDB, minimum
dermatologic database.
STEP 6: Diet Trial
Complete response Partial response No response
Pruritus when diet
is challenged
FIGURE 6
Diagnosing Allergic Skin Disease in the Feline Patient.
JAAHA.ORG 17

Treat Secondary Infections
Superficial skin cytology is the diagnostic method of choice to iden-
tify the presence of secondary infection with either bacteria or Malas-
sezia and can be performed using a microscope slide (for a direct
impression smear of exudative lesions) and acetate tape (for scaling,
crusting, and erythema).
Treatment for bacterial infection (amoxicillin-clavulanic acid
12.5–20 mg/kg orally twice daily; clindamycin 11–33 mg/kg orally
once daily; cefovecin 8 mg/kg subcutaneously) should be based on
the presence of degenerate neutrophils with cocci-shaped bacteria.
39
Bacterial culture and susceptibility testing may be needed in more
complicated cases involving rod-shaped bacteria. Finding more than
one Malassezia per high-power field suggests yeast overgrowth
40
and
may warrant systemic therapy.
41
For Malassezia dermatitis, itracon-
azole, fluconazole, or terbinafine should be selected (Table 9). Keto-
conazole may cause severe hepatotoxicity in cats.
42
Although topical antimicrobial therapies are ideal to reduce the
overall exposure to systemic antibiotics, the grooming behavior of
cats and their decreased tolerance for topical applications often limits
their use.
If diagnostics cannot be performed because of client
financial constraints, then it would be most advan-
tageous to use a broad-spectrum external parasite
treatment in addition to a tapering course of oral
glucocorticoids.
Step Five: Recheck, Assess Response to
Antiparasitic/Antipruritic Therapy
In flea-endemic areas, consistent flea prevention should be continued
in all cats year-round regardless of their flea history to reduce the
possible burden of flea allergy leading to worsening dermatitis and
pruritus. If there is no improvement or only partial improvement of
pruritus and clinical lesions after ectoparasiticide treatment and
addressing secondary infections, then other causes of pruritus should
be investigated. A skin biopsy is recommended in cases with atypical
lesions to rule out other pruritic dermatoses (e.g., pemphigus folia-
ceus), especially in cases of crusting dermatitis without cytologic evi-
dence of bacterial or yeast. With nonseasonal pruritus, a restrictive
diet trial should be pursued to rule out food allergies.
Step Six: Diet Trial
Food allergies in cats can only be diagnosed with an elimination diet
trial, by feeding either a hydrolyzed or a novel protein diet.
43–45
Definitive diagnosis is ultimately confirmed if the pruritus and/or
skin lesions return after challenging the cat with the previous diet
and then resolve again once returning to the restrictive diet. It is
recommended to conduct the elimination diet trial for 8 wk, as 90%
of food-allergic cats resolve their clinical signs by this time point,
whereas 50% of feline food-a llergic cases resolve at 4 wk.
46
Use of OTC diets should not be recommended
when conducting a diet trial in cats. Ingredients
not declared on the label (e.g., chicken) have been
detected in up to 82% of OTC feline diets,
47,48
pos-
sibly negating the results of the trial. However, the
guidelines task force agrees that an OTC novel pro-
tein diet can be used if financial constraints make
other diets impossible. The client should be warned
that an OTC diet may not provide optimal results
and should be considered a diet change, not a true
diet trial.
Systemic glucocorticoids can be withdrawn at the 3 wk point of
a diet trial and/or parasite treatment trial and again at the 6 wk point
to assess response to diet alone.
Feline Atopic Skin Syndrome Diagnosis
FASS can only be diagnosed based on compatible history and clini-
cal signs and by ruling out all other diseases that can look similar
to this disease (i.e., flea allergy, food allergy, external parasites, bac-
terial skin infection, and dermatophytosis). Up to 25–30% of cats
with FASS will exhibit seasonal patterns,
32
which supports a diag-
nosis of environmental allergies without the need for an elimina-
tion diet trial, if external parasites and secondary skin infections
have been treated and/or ruled out. Otherwise, lack of response to
a restrictive diet trial would indicate FASS in the nonseasonal pru-
ritic cat.
Once a diagnosis of FASS has been achieved by pro-
cess of elimination, intradermal or serum allergy test-
ing by a veterinary dermatologist is then a useful
tool to identify which specific environmental allergens
should be included in allergy immunotherapy.
Superficial bacterial skin infection due to Staphylococcus spp. on
the lateral neck of a cat. Note the alopecia, exudate, crusting, ery-
thema, and erosions.
Credit: Photo courtesy of Andrew Simpson, DVM, MS, DACVD
18 JAAHA | 59:6 Nov/Dec 2023

Section 4: Managing Feline Chronic
Allergic Conditions
Top 3 Takeaways:
1. Ectoparasites and infections need to be ruled in/out and addressed
before treating allergic skin disease in cats.
2. Flea allergy dermatitis is the most common allergic skin disease; dil-
igent adulticidal flea prevention is key in any pruritic feline patient
as this can be a complicating concurrent factor.
3. FASS has different management considerations compared with
canine atopic dermatitis; partnership with a veterinary dermatolo-
gist can be beneficial for these patients.
Overview
Identifying the cause(s) of an allergic condition can be a long, often
frustrating process of trial and error for both clients and veterinary
staff. Although ultimately discovering the source brings relief, this is
actually just the beginning of another stage that will last the cat’s
lifetime—that of managing a chronic condition. Before launching
into what will be required next, however, pausing to congratulate the
client for seeing the diagnosis process through speaks volumes about a
practice’s compassion and desire to cultivate long-lasting relationships.
Treating Flea Allergy
Flea allergy dermatitis is the most common allergic skin disease, seen
solely or concurrently with other allergic conditions. Diligent adulti-
cidal flea prevention must continue long term and consists of the
following considerations:
1. Use FDA-approved products for cats.
2. Recommend isoxazoline medications for broad coverage (fluralaner,
sarolaner, lotilaner, 6 selamectin or moxidectin).
3. Treat for the proper duration and response for fleas versus mites.
TABLE 6
Antipruritic and Anti-inflammatory Medications for Cats
JAAHA.ORG 19

4. If there are multiple cats or the client has difficulty medicating, con-
sider imidacloprid/flumethrin collars.
5. Ensure other animals are treated and on year-round prevention as
well.
6. Consider environmental treatment.
7. Educate clients on the life cycle of fleas, including the time it takes
to see treatment response.
8. Symptomatic antipruritic therapy:
Prednisolone 2 mg/kg/day per os (PO) tapered over 3 wk
Methylprednisolone 0.8–1.5 mg/kg/day PO tapered over 3 wk
Dexamethasone 0.2 mg/kg/day PO tapered over 3 wk
Technicians can discuss treatment of other pets in
the households, explain parasite life cycles, and rein-
force the importance of year-round prevention with
clients.
Treating Food Allergy
Food allergy (at least anecdotally) seems to be more common in cats
than dogs. For cats, palatability of a diet and securing the preferred
formulation (e.g., dry only versus wet) are important considerations,
especially if the patient is a picky eater. Ideally, a prescription veteri-
nary diet should be fed long term with either a novel protein diet
(e.g., rabbit, kangaroo, or alligator) or a hydrolyzed diet (hydrolyzed
soy, hydrolyzed fish, or hydrolyzed poultry feather). If a specificaller-
gen is identi fied, an OTC diet that does not contain this allergen may
be an effective choice for long-term management. Once an appropri-
ate diet has been identified, clients must stick to the regimen and
understand this will be a commitment for the rest of the cat’slife.
During client education, technicians or members of the veteri-
nary team should advise clients to plan for possible shortages or
backorders of special diets. Keeping extra bags or cans of food on
hand is one strategy. Considering different brands with similar or
identical ingredients is another. Choosing a home-cooked diet in
consultation with a veterinary nutritionist is a third strategy, but it
should be done with extreme caution to account for the specific
nutritional needs of cats.
Treating Feline Atopic Skin Syndrome
A diagnosis of FASS is an excellent juncture in treatment to consider
referral to a veterinary dermatologist if this has not occurred already.
Finding the proper therapeutic regimen for a feline patient and client
can be challenging, and “tinkering” with options that do not provide
sufficient improvement tends to lead to client frustration and poten-
tial loss of trust.
49
Even for clients with cost concerns, a veterinary
dermatologist can provide more targeted treatment to bring the
patient relief. Moreover, there may be time and cost savings in the
long run with more targeted treatments.
If referral is not possible or desired, establishing a baseline level
of pruritus at this point is helpful to assess response to various
therapeutic interventions. Because glucocorticoids tend to provide
relief for most allergic cats, they should be considered as a first test
intervention to determine the degree of improvement. If FASS is sea-
sonal,theymaybeanoptionforcontinuedmanagement.
Once pruritus surpasses 6 out of 12 mo in a given year, alterna-
tive options should be discussed with the clients (see Table 7).
Cyclosporine is a labeled treatment for feline allergy and comes
in liquid form; however, its palatability is questionable, and many
owners struggle with administration. It takes time to reach therapeu-
tic levels (4–6 wk), but at that point, most cats can have the fre-
quency decreased to every other day (or possibly less). This should
not be recommended for cats that go outside owing to the increased
risk of infectious disease exposure that may be fatal on this medica-
tion (e.g., toxoplasmosis). Cats on this medication should be fed a
cooked diet and maintained on effective internal and external para-
site control measures.
Oclacitinib is not labeled for cats and has not been thoroughly
assessed in this species with regard to long-term safety and dosing.
The task force does not recommend the use of oclacitinib in cats at
this time.
Lokivetmab should not be used in cats; this caninized monoclonal
antibody can potentially be fatal if administered to a non-dog species.
Immunotherapy canbeanexcellentoptionforcatswithFASS
as this species tends to respond more favorably than not.
35
Keep in
mind that allergy tests, both serum and intradermal, do not diagnose
allergy but rather support the clinical diagnosis and aid in immuno-
therapy formulation; they should not be used as “allergic or not”
diagnostics, as they can be positive in animals with no clinical signs
of allergy. Both injectable and sublingual immunotherapy may be
considered depending on client and patient preference. Most owners
elect injections first due to ease of administration, but the oral option
is also effective in cats.
Opting for immunotherapy is another treatment
juncture where veterinary dermatologists may be
more adept at the intricacies of testing, formula-
tions, and making appropriate adjustments.
Alternative or adjunct therapies to consider in the allergic
feline include the following:
Antihistamines. Can be helpful in cats with concurrent upper respi-
ratory manifestation of allergy, but they do not provide much pruri-
tus relief (Table 8).
Nutraceuticals (e.g., ultra-micronized palmitoylethanolamide and essen-
tial fatty acids). These can be administered separately as supplements,
or some clients may appreciate the benefitfroma“skin support” diet
that includes these ingredients as opposed to another oral therapy.
Topical skin barrier support (e.g., fatty acid/essential oil spot-on
formulations). The benefits of these interventions to allergic cats are
somewhat uncertain owing to the lack of information supporting
the impact of barrier dysfunction in feline allergy. They may at least
20 JAAHA | 59:6 Nov/Dec 2023

be good options for mildly affected cats or as adjunct therapy to
reduce other medication requirements.
Treating Flares
As with dogs, even the best-managed allergic cat can experience
episodes of pruritic flare. It is imperative to reassess the presence
of ectoparasites and secondary bacterial and yeast infections in
this situation, as these remain common complications in the face
of allergy. Additionally, remind owners that treatment does not
just stop working once it has been determined to be beneficial;
rather, the cat may need a bit of extra support during these
episodes.
To provide antipruritic and anti-inflammatory benefit during
acute flares, a tapering course of systemic glucocorticoids should be
considered, such as prednisolone (2 mg/kg PO q 24 hr), methylpred-
nisolone (0.8–1.5 mg/kg PO q 24 hr), or dexamethasone (0.2 mg/kg
PO q 24 hr). In addition, in cases in which cats have been receiving
lower-dose cyclosporine (i.e., every-other-day dosing or twice-weekly
dosing), a temporary increase to once-daily dosing can be recom-
mended for 3–4wk.
Section 5: Otitis Externa
Top 3 Takeaways:
1. Recurrent otitis externa is commonly caused by underlying allergic
disease, and in some patients, it may be the only clinical manifesta-
tion of allergy.
2. Cytology should be performed in every case of otitis externa.
3. The goal of short-term treatment is to reduce inflammation and
treat secondary infection (where present), while long-term manage-
ment aims to control inflammation and maintain ear health.
TABLE 7
Acute Flare and Long-term Management Therapies in Cats
JAAHA.ORG 21

Overview
Allergic otitis externa (AOE) is a common manifestation of allergy in
animals and in some cases is the only clinical sign. AOE is an inflam-
matory condition of the ear and should not be confused with
infection—which commonly occurs secondary to AOE. Although it
is important to identify and treat secondary infections, identification
of the primary (underlying) cause of otitis externa is critical to the
prevention of recurrent otitis. More than half of dogs and 20% of
cats with allergies have AOE.
50–52
Other primary causes of otitis
externa include parasites, foreign body, neoplasia, endocrinopathy,
andkeratinizationdisordersandshouldberuledoutinevery
case.
26,51
AOE occurs frequently in patients with atopic dermatitis
andfoodallergybutisnotafeatureofflea allergy dermatitis.
Clinical Presentation
Most cases of AOE present as bilateral ear disease—although disease
severity may differ between ears. Otic pruritus manifests as head
shaking, scratching at the ears, and rubbing the face/head. Clinical
signs of AOE include pruritus, pain, erythema, ceruminous (waxy)
exudate, periauricular alopecia, and excoriation. When secondary
infection is present, otic exudate (6 malodorous), crusting/scaling,
erosions, and asymmetric ear carriage may also oc cur. Otitis
media/interna should be suspected in animals presenting with hear-
ing loss, head tilt, vestibular disturbances, Horner’ssyndrome,
and/or temporomandibular joint pain.
Diagnosis
The importance of a thorough evaluation of the ears in any patient
presenting with dermatologic disease cannot be overemphasized. This
includes examination of the periauricular region and pinna, palpa-
tion of the canals, and otoscopic examination. Pliability of the carti-
laginous structures of the ear canals provide clues to pathologic
changes that can result from chronic inflammation, which can ulti-
mately lead to calcification. Otoscopy not only is important for
examination of deeper ear structures but also helps to rule out most
other primary causes of otitis externa. Chronic inflammation can
lead to ceruminous gland hyperplasia within the ear canals causing a
cobblestone-like appearance.
51
Stenosis of the ear canals occurs
because of edema and inflammation and/or pathologic changes to
the ear over time.
Secondary infection is common in animals with AOE. Altera-
tions of the skin’s natural flora have been demonstrated in dogs with
TABLE 8
Oral Antihistamine Doses for Cats
Drug Name Dose
Hydroxyzine 5–10 mg/cat (NOT mg/kg) q 12 hr
1
Cetirizine
5–10 mg/cat (NOT mg/kg) q 24 hr
2
Chlorpheniramine
2–4 mg/cat (NOT mg/kg) q 12 hr
2
Cyproheptadine
2 mg/cat (NOT mg/kg) q 12 hr
2
Clemastine
0.68 mg/cat (NOT mg/kg) q 12 hr
2
Loratadine
2.5–5 mg/cat (NOT mg/kg) PO q 24 hr
1
Fexofenadine 30–60 mg/cat (NOT mg/kg) PO q 24 hr
3
Amitriptyline 2.5–7.5 mg/cat PO (NOT mg/kg) q 12 hr
1
Diphenhydramine 2–3 mg/kg q 12 hr
2
1 Plumb DC. Plumb’s Veterinary Drug Handbook. 9th ed. Wiley-Blackwell;2018.
2 Muller & Kirk’s Small Animal Dermatology. 7th ed.
St. Louis:Elsevier;2013.
3 Diesel A. Feline allergy: symptomatic treatments. In: Noli C, Foster A, Rosenkrantz W,
Miller WH, Grin GE, Campbell KL.
eds. Veterinary Allergy. West Sussex (UK):John Wiley and Sons;2014.
TABLE 9
Oral Antifungal Medication Doses for Cats
1,2
Drug Name Dose
Ketoconazole Contraindicated—causes
severe hepatotoxicity
2
Fluconazole 5–10 mg/kg q 24 hr
Itraconazole 5 mg/kg q 24 hr
Terbinafine 30–40 mg/kg q 24 hr
1 Muller & Kirk’s
Small Animal Dermatology. 7th ed.
St. Louis:Elsevier;2013.
2 Plumb DC.
Miller WH, Grin GE, Campbell KL.
Plumb’s Veterinary Drug Handbook.
9th ed. Wiley-Blackwell;2018.
22 JAAHA | 59:6 Nov/Dec 2023

atopic dermatitis, and a similar dysbiosis has also been observed
within the ear canals of atopic dogs having increased amounts of
Staphylococcus spp. relative to normal dogs.
53
Inflammation causes
changes to the ear canal microenvironment, altering the bacterial
population and creating an ideal environment for yeast (Malassezia
spp.) overgrowth.
51
Therefore, it is imperative that ear cytology be
performed in every case of AOE. Diagnostic evaluation should
include both a stained, dry-mounted sample to assess for microbial
infection and an unstained, mineral oil wet mount to rule out otic
ectoparasites. This is of particular importance in cats because of the
prevalence of Otodectes in this species.
Training technicians to obtain an d interpret ear
cytology facilitates increased efficiency when seeing
appointments.
Treatment
Topical therapy should always be guided by cytologic findings. In
cases with abundant exudate, an in-clinic ear flush should be per-
formed to aid in the removal of exudate and facilitate a more thor-
ough otoscopic examination. Caution should be exercised in cases of
a ruptured tympanic membrane, with careful selection of antimicro-
bial agents and cleaning solutions that are safe for use in the middle
ear. Discussion of specific products and ingredients is beyond the
scope of these guidelines.
In difficult cases of otitis externa in which the
patient has failed numerous treatment protocols
and/or there is no resolution after 3–6mooftreat-
ment, collaborative care with a board-certified der-
matologist is recommended as this h as been shown
to significantly improve resolution of chronic otitis
with infection.
54
Treatment recommendations for secondary infections in AOE
are beyond the scope of these guidelines.
Short-term and Long-term Management of AOE
The short-term goal of therapy is to reduce inflammation and treat
secondary microbial infection (where present). Oral corticosteroids
in a short, tapering course at anti-inflammatory doses or oclacitinib
may be used for control of inflammation and pruritus. Corticoster-
oids applied topically are also effective.
The long-term goal of therapy focuses on control of inflamma-
tion and maintenance of ear health. Managing the underlying allergy
is key to minimizing AOE. When crafting an allergy management
plan in patients with AOE, one must be mindful that medications
used to manage atopic dermatitis have varying efficacy against AOE
and individual patient response must be assessed.
Routine, topical maintenance therapies are often very helpful in
reducing the recurrence of AOE. Routine ear cleaning based on an
individual patient’s needs is useful to maintain a healthy microenvi-
ronment and remove debris and ceruminous material from the ear
canals. Cleansing agents that promote epidermal barrier function are
useful to reduce microbial adherence to the epithelium and should
be considered in individuals prone to secondary infection. Topical
glucocorticoids (e.g., hydrocortisone and dexamethasone) aid the
management of inflammation in the ear canal and may help prevent
allergic flares and secondary infections as well.
Referral is indicated if the patient has AOE that is
complicated with secondary i nfection that is not
responding to empiric treatment, if it involves a resis-
tant organism, and/or if the patient has otitis media.
54
Demonstration of ear cleaning technique and topi-
cal medication application is vital to success and
should be the responsibility of a veterinary techni-
cian. Veterinary technicians can also conduct interim
follow-up with the client via telephone, text message,
video chat, or email.
Section 6: Spectrum of Care Considerations
in Managing Allergic Skin Diseases
Top 3 Takeaways:
1. Gather a thorough and relevant history and use pattern recognition
and probabilistic clinical reasoning.
2. Recognize when diagnostics and referral are necessary.
3. Use efficient but effective client communication to manage client
expectations.
Overview
Spectrum of care (SOC) is the practice of providing a continuum of
acceptable care that considers available evidence-based medicine
while remaining responsive to client expectations and financial lim-
itations.
55
SOC considerations are highly relevant to allergic skin dis-
ease in dogs and cats because skin allergies, ear infections, and skin
infections were in the top 10 medical conditions submitted for
Nationwide pet insurance claims in 2021.
56
The key components of successfully practicing SOC are gather-
ing a thorough and relevant history, using pattern recognition and
probabilistic clinical reasoning, recognizing when diagnostics and
referral are necessary, and communicating with clients efficiently but
effectively to manage expectations.
Step One: Clinical History
During the history-taking process, it is critical to focus on previous
diagnostics, response to therapies, seasonality, signalment, and realistic
compliance from the client. Compliance can be affected not only by
financial limitations but also by the level of ability to give medications
JAAHA.ORG 23
and administer topical therapies, perform strict diet trials, and/or have
the time and access to return for recheck appointments. All of these
factors are important to understand and balance when developing
diagnostic and treatment plans.
Owing to the need for efficiency in general practice, having a
specific dermatologic history form sent to clients ahead of time can
be very helpful, as can training technical staff on proper history tak-
ing and client education. Also, consider an easily accessible area in
your records for recording the history of treatment successes and
failures to eliminate digging through previous records.
Step Two: Physical Examination
The practice of SOC relies heavily on pattern recognition and using a
probabilistic clinical reasoning approach to determine the most likely
diagnosis. This requires understanding common clinical presentations,
as well as using therapy trials to confirm or deny a suspected diagnosis.
Training technicians on collection of samples for cytology, skin
scrapings, flea combing, etc. can contribute to a more thorough and
efficient appointment.
Step Three: Treatment
Communicating the pros and cons of all therapeutic options to cli-
ents before treatment choices are made is vital for clients to be able
to make educated decisions. When developing a plan:
Acknowled ge that rising costs of many products to manage allergic dis-
ease, from oclacitinib to lokivetmab, immunotherapy, and prescription
diets, continue to make allergic management financially challenging;
Explain that using cost-effective therapies is at times necessary,
including steroids, antihistamines, and/or limited-ingredient diets for
SOC, but that the cat or dog is not getting substandard medicine;
Consider adjustments of monitoring protocols for certain medica-
tions as an area of cost that may need to be discussed, too.
Recognizing treatment failures and/or poor medical management
should trigger a change to a more standardized clinical approach if
possible. This shift in clinical approach often must start with helping
clients maintain realistic expectations and explaining why the need
now is for diagnostics and/or more aggressive therapies. Continued
conversations about SOC are essential for removing the substandard
care stigma associated with meeting clients where they are.
Step Four: When to Refer
Asignificant part of financial considerations for managing both the
short- and long-term costs associated with allergic skin disease is rec-
ognizing when early diagnostics or referral may have better clinical
and fin ancial outcomes. For example, early referral for chronic AOE
to specialis ts result ed in improved clini cal outcom es and reduced
recurrence.
54
Other considerations would be an early recommendation
for referral to a specialist for suspected canine atopy in young patients
who will require therapy for 51 yr, versus waiting until the patients
fail all medical management options offered in general practice. A sur-
vey performed by the American College of Veterinary Dermatologists
revealed that 82% of clients would have felt better about their primary
care veterinarian if they had been referred earlier. Seventy-three per-
cent of clients reached a “tipping point of frustration” if they visited
their primary care veterinarian more than three times for a dermato-
logic issue, and 15% of these clients stopped visiting their primary care
veterinarian for their pets’ routinecareaswell.
49,57
Step Five: Using Telehealth
Because the management of allergic disease is so dependent on fre-
quent communication, the use of telehealth technologies can cut
costs and save both clients’ and veterinarians’ valuable time. Most
practices are already using phone and email follow-ups. Photographs
or videos sent from clients can be reviewed for progress in an asyn-
chronous manner, allowing technicians to assist in the triage process.
Video calling and communication platforms like FaceTime and
Zoom can provide real-time visuals and conversations. It is impor-
tant to remember, however, that many dermatologic conditions may
be infectious in nature, and telehealth may have limited applications
as it does not afford the opportunity to perform cytologic evaluations
or otoscopic examination to detect occult cases of otitis externa.
When using telehealth, it is important to follow all applicable laws
and regulations regarding the establishment of a veterinarian-client-
patient relationship when required. For information about state-level
requirements, contact the state board of veterinary medicine.
The use of teleconsulting to bridge the gap between the client
and a specialist is also an increasingly available option to improve
access to specialty care. Teleconsulting can be useful when access to
specialists is limited by distance, wait times, or finances as this
modality allows access to a wider number of specialists.
To learn more about integrating telehealth options into veteri-
nary practice, refer to the 2021 AAHA/AVMA Telehealth Guidelines
for Small-Animal Practice at aaha.org/telehealth.
Section 7: Technician Utilization in
Managing Allergic Skin Diseases
Top 3 Takeaways:
1. Empower technicians to do everything within state regulations that
does not require a veterinary medical degree.
2. Spend time training technicians on how to conduct diagnostic tests
and the best way to explain procedures and treatments to clients.
24 JAAHA | 59:6 Nov/Dec 2023

3. Allowing technicians to do more will enable the veterinarian to see
more patients more efficiently.
Overview
Credentialed veterinary technicians play essential roles in clinics that
strive for outstanding client service, quality patient care, and efficient
workflow. The only limiting factors are state regulations and a veteri-
narian’s willingness to train technicians to take over specific duties
within defined parameters.
Many technicians want more responsibility commensurate with
their training, and empowering them to assume additional job duties
is a wise investment of time for veterinarians. For more information
on the many and varied roles technicians can take to streamline
practice and improve patient care, see the 2023 AAHA Technician
Utilization Guidelines at aaha.org/technician-utilization.
Key Duties During the Examination
Technicians are essential in many aspects of a veterinary dermato-
logic consultation, starting with a detailed dermatologic history,
physical examination, and setting expectations.
Technicians can collect, process, and interpret basic cytology. Train-
ing a technician on cytologic interpretation will take time, but once
training is complete, the technician should be able to analyze slides
very quickly. A single technician proficient in cytology can train the
rest of the staff.
Blood and urine can also be collected and processed by the technical
staff.
Key Veterinary Technician Duties During
Patient Discharge
Discharge patients and review treatment plans with clients, includ-
ing showing clients how to do treatments, such as ear cleanings or
topical therapies, which greatly improves client compliance and
therapy success rates.
Double-check that medications have clear directions and are sent
home with explanations.
Emphasize to clients how mu ltiple types of th erapies w ork
together to achieve results; therefore, all need to be part of the
comprehensive plan.
Remind clients to have realistic expectations when it comes to
results. Most treatments do not work overnight, and it will take sev-
eral weeks to see improvement. Technicians can help clients under-
stand that they are beginning a long journey while reassuring them
that they have the support of the veterinary team.
Essential Duties During Follow-up and
Ongoing Treatment
Early interaction during appointments helps clients feel comfortable
talking with technicians throughout follow-up and in instances in
which the veterinarian is unavailable. Involving technicians in client
education both in-clinic and once the patient leaves decreases the
time the veterinarian spends on the phone or in the examination
rooms.
Day-after calls to chec k on the patient( s) and ensure clients
can complete all treatments as directed is one area where techni-
cians can be involved. Phone follow-up is also beneficial at other
times, such as 2–3 wk into a diet trial or 1 wk after starting anti-
pruritic therapies. Howeve r, a caveat for risk management is that
technicians must always document client discussions in the
patient’s medical records, and “spoke with client ” is inadequate.
Thorough summaries of client discussions help protect the techni-
cian’s and veterinarian’ s licenses should anyone ever question
what was said.
Practice Tip: Technicians can be involved in preparing short
instructional videos that can be sent to clients or linked to the prac-
tice’swebsite.
Resources to Assist in Training Technicians
Resources that can be valuable to the veterinary team include the
following:
Teaching sets of cytologic samples collected for training purposes
Training videos, particularly if technicians have on-demand access
A dedicated space for telehealth consultations that is well lit and
quiet with a computer camera
Locally offered continuing education courses or sessions put on by
colleges and/or associations
In-house continuing education for the whole veterinary team,
including technicians and the veterinarian(s)
A veterinarian working with two technicians can see two
appointments in the time it would otherwise take to see one. As
Figure 7 shows, technicians can interface with clients from the begin-
ning of an appointment through discharge and beyond. Having
established a relationship with clients, they can be trusted team
members for follow-up checks and maintenance program assistance.
Working this way, a diagnostic plan can be developed for multiple
patients in the time it could have taken to see only one patient.
Section 8: Client Communication
Top 3 Takeaways:
1. Be clear about timelines and expectations—diagnosing and finding
the right combination of treatments may take 2–4 mo or sometimes
longer.
Being aware of state regulations is the responsibility of the creden-
tialed technician and the management team, and all actions taken
must fall within the scope of their license. The entire veterinary
team should become familiar with the scope of practice for creden-
tialed technicians in their state.
JAAHA.ORG 25

Tech 1 in Exam 1 obtains a detailed dermatologic history
and quick physical examination, and collects the minimum
dermatologic database (fl ea combing/cytologies/skin
scrapings).
Dr. enters the room, performs a physical exam, and asks
additional history/follow-up questions WHILE Tech 1
is processing slides and documenting fi ndings.
Tech 1 brings results to Dr. in Exam 1. Final plan is formed. Tech 2 in Exam 2 obtains history, quick physical exam, and
minimum database.
Dr. moves to Exam 2 to conduct a physical exam of the
patient and discussion with the client. Tech 2 is processing
and documenting minimum database results.
Tech 1 implements the plan for the patient in Exam 1, acquires
further diagnostics, gathers prescriptions, and instructs the
client on administration, expectations, and follow-ups.
Dr. moves on to the next exam room, and Tech 2 implements
the plan for the patient in Exam 2.
Tech 2 brings results to Dr. in Exam 2, and the fi nal plan is
formed.
1
5
4
8
2
6
3
7
FIGURE 7
Flowchart of Technician Utilization for Allergic Skin Diseases.
26 JAAHA | 59:6 Nov/Dec 2023

YES NO YES
YES
NO
NO
YES NO
Can oral medications be given by the caregiver or family members once every 8, 12, or 24 hr?
Injectable administration:
antibiotics, lokivetmab.
Oral administration:
ectoparasite treatment/
preventive, antibiotics,
antihistamines, oclacinitib,
cyclosporine, steroids.
Topical applications except
for medicated bath: sprays,
ointments, drops, flush,
mousse, or wipes.
Topical application with
medicated bath using
medicated shampoo.
Can anyone in the home bathe
the pet once to twice weekly?
Can anyone in the home
apply other topicals daily?
Can anyone in the home bathe
the pet once to twice weekly?
Can anyone in the home
apply other topicals daily?
YES NO
FIGURE 8
Client Communication Flow Chart for Treatment Plans.
JAAHA.ORG 27

2. Openly discuss any client constraints at the first appointment,
including time, work schedule, household environment, and finan-
cial concerns, so a realistic plan can be made.
3. Prepare clients for the fact that flares occur even in well-managed
cases so that they do not get frustrated when they happen.
Overview
Effective client communication is vital in every aspect of a practice.
However, client communication becomes even more paramount
when initially explaining diagnostic options, time frames, and treat-
ment variables for allergic dogs and cats. With most of these patients,
this is the start of a long journey, and clients should be informed
that there are likely no quick fixes or cures, only lifetime manage-
ment strategies.
How effectively the veterinary team explains short-term and
long-term steps toward relief and healing will set up the client’s
expectations for what lies ahead.
Communication should start at the first appointment and carry
on throughout all follow-up visits. It is important to openly, and
without judgment, discuss any constraints (e.g., time, work sche-
dules, transportation, finances, and/or inability to administer specific
treatments) to better negotiate a plan that cares for the patient and is
within the client’s capability.
10 Key Messaging Points When Talking to Clients
Each dog and cat will need a specifically tailored plan for the pet and
client. Although there are basic steps to follow, some pets will
respond to one approach and others to another. Keep in mind that
diagnosing allergic skin diseases can be a long process that can
become frustrating and confusing for clients.
1. Be clear about goals: The goal is to bring the pet relief as soon as
possible, which often requires clearing any secondary infections
that may be present, possibly even before the source of the allergy
is determined.
2. Be clear about the costs associated with diagnosis and treatment.
Emphasize that altering strategies to meet the client’s current
capacities does not mean substandard care. Offer referral as an
option and allow the client to make an informed decision.
3. Provide timelines for clients. Determining the best long-term treat-
ment plan for an individual patient may take 2–4 mo. Be clear
about the stages of diagnosis/treatment and what needs to happen
concurrently.
4. Let clients know that management of the allergy is for the pet’slife
and medication adjustments will likely be needed over time. Alert the
client that flares are not uncommon, even if their pet is well managed.
5. Strive for empathetic and nonjudgmental communication so that cli-
ents feel comfortable expressing concerns, bringing up constraints,
and asking questions if they do not understand something. Encourage
clients to be active partners in determining the health of their pets.
6. Recognize that clients may suffer from information overload and
become overwhelmed during appointments. Provide clear written
instructions and repetition, and if necessary, take a break so they
can process the information.
7. Ask the client how they prefer to receive information, for example,
verbally, written, or on video. Provide several options and
always send home written or recorded instructions they can refer
to later.
8. Precise wording and label instructions are keys to good compliance
and secondary infection control. For example, to maintain an ade-
quate serum concentration level of cefpodoxime, be sure to say,
“Administer one tablet by mouth at the same time once every
24 hours,” instead of saying, “Administer one tablet daily.”
9. Praise clients for compliance when they bring their pets for
rechecks, even if the improvement is slight.
10. Be sure to talk to clients about ongoing monitoring, like blood
work, depending on what medications their animal is receiving.
Summary
Managing allergic skin diseases in dogs and cats requires a multi-
modal, communication-rich approach to ensure positive outcomes.
A detailed history must be taken, including response to previous
treatment, and a physical examination must be performed with par-
ticular attention to ears, skin folds, and paws. A minimum dermato-
logic database should be collected (cytology of skin and ears, skin
scrapings, 6 DTM). Optimal technician utilization can result in
more efficient intake, management, and follow-up of cases. Effective
communication with clients is crucial for these often-frustrating
cases. Clients must be prepared for the fact that these cases require
lifelong maintenance and treatment for the occasional flares that will
occur even in the most well-managed patients. Collaborative care
with dermatology specialists has been shown to increase client satis-
faction and speed resolution of cases and should be considered early
for some patie nts. SOC considerations entail “meeting clients where
they are” and providing viable options, while emphasizing that these
options do not mean the pet is getting substandard care.
REFERENCES
1 Favrot C, Steffan J, Seewald W, et al. A prospective study on the clinical
features of chronic canine atopic dermatitis and its diagnosis. Vet Derma-
tol 2010;21(1):23–31.
2 Olivry T, Mueller RS. Critically appraised topic on adverse food reactions
of companion animals (7): signalment and cutaneous manifestations of
dogs and cats with adverse food reactions. BMC Vet Res 2019;15:140.
3 Mueller RS, Olivry T. Critically appraised topic on adverse food reactions
of companion animals (6): prevalence of noncutaneous manifestations of
adverse food reactions in dogs and cats. BMC Vet Res 2018;14:341.
4 Hillier A, Lloyd DH, Weese JS, et al. Guidelines for the diagnosis and
antimicrobial therapy of canine superficial bacterial folliculitis (Antimi-
crobial Guidelines Working Group of the International Society for Com-
panion Animal Infectious Diseases). Vet Dermatol 2014;25:163–e43.
5 Bond R, Morris DO, Guillot J, et al. Biology, diagnosis and treatment of
Malassezia dermatitis in dogs and cats: Clinical Consensus Guidelines of
the World Association for Veterinary Dermatology. Vet Dermatol 2020;
31(1):75.
28 JAAHA | 59:6 Nov/Dec 2023
6 Lam ATH, Johnson LN, Heinze CR. Assessment of the clinical accuracy
of serum and saliva assays for identification of adverse food reaction in
dogs without clinical signs of disease. J Am Vet Med Assoc 2019;255(7):
812–6.
7 Olivry T, Mueller RS, Pr
elaud P. Critically appraised topic on adverse
food reactions of companion animals (1): duration of elimination diets.
BMC Vet Res 2015;11:225.
8 Possebom J, Cruz A, Gmyterco VC, et al. Combined prick and patch
tests for diagnosis of food hypersensitivity in dogs with chronic pruritus.
Vet Dermatol 2022;33(2):124–e36.
9 Fischer N, Spielhofer L, Martini F, et al. Sensitivity and specificity of a
shortened elimination diet protocol for the diagnosis of food-induced
atopic dermatitis (FIAD). Vet Dermatol 2021;32(3):247–e65.
10 Raditic DM, Remillard RL, Tater KC. ELISA testing for common food
antigens in four dry dog foods used in dietary elimination trials. JAnim
Physiol Anim Nutr (Berl) 2011;95(1):90–7.
11 Olivry T, Mueller RS. Critically appraised topic on adverse food reactions
of companion animals (5): discrepancies between ingredients and labeling
in commercial pet foods. BMC Vet Res 2018;14:24.
12 Becskei C, DeBock F, Illambas J, et al. Efficacy and safety of a novel oral
isoxazoline, sarolaner (Simparica) in the treatment of naturally occurring
flea and tick infestations in dogs presented as veterinary patients in
Europe. Vet Parasit 2016;222:49–55.
13 Biel W, Natonek-Wi
sniewska M, Ke¸pi
nska-Pacelik J, et al. Detection of
chicken DNA in commercial dog foods. BMC Vet Res 2022;18:92.
14 Gadeyne C, Little P, King VL, et al. Efficacy of oclacitinib (Apoquel
V
R
)
compared with prednisolone for the control of pruritus and clinical signs
associated with allergic dermatitis in client-owned dogs in Australia. Vet
Dermatol 2014;25(6):512–e86.
15 Santoro D. Therapies in canine atopic dermatitis: an update. Vet Clin
Small Anim 2019;49:9–26.
16 Marsella R, Ahrens K, Wilkes R, et al. Comparison of various treatment
options for canine atopic dermatitis: a blinded, randomized, controlled
study in a colony of research atopic beagle dogs. Vet Dermatol 2020;31:
284–e69.
17 Van Brussel L, Moyaert H, Escalada M, et al. A masked, randomized
clinical trial evaluating the efficacy and safety of lokivetmab compared to
saline control in client-owned dogs with allergic dermatitis. Vet Dermatol
2021;32:477–e131.
18 Olivry T, DeBoer DJ, Favrot C, et al. Treatment of canine atopic dermati-
tis: 2015 updated guidelines from the International Committee on Aller-
gic Diseases of Animals (ICADA). BMC Vet Res 2015;11:210–25.
19 Saridomichelakis MN, Olivry T. An update on the treatment of canine
atopic dermatitis. Vet J 2016;207:29–37.
20 Ngo J, Taminiau B, Fall PA, et al. Ear canal microbiota – a comparison
between healthy dogs and atopic dogs without clinical signs of otitis
externa. Vet Dermatol 2018;29(5):425–e140.
21 Fischer NM, Mueller RS. Allergen specific immunotherapy in canine
atopic dermatitis: An update. Curr Dermatol Rep 2019;8:297–302.
22 Fennis EEM, van Damme CMM, Schlotter YM, et al. Efficacy of subcuta-
neous allergen immunotherapy in atopic dogs: A retrospective study of
664 cases. Vet Dermatol 2022;33(4):321–e75.
23 Mueller RS. Update on allergen immunotherapy. Vet Clin North Am
Small Anim Pract 2019;49(1):1–7.
24 DeBoer DJ, Morris M. Multicentre open trial demonstrates efficacy of
sublingual immunotherapy in canine atopic dermatitis. Vet Dermatol
2012;23(suppl 1):65.
25 Carlotti DN, Gribeauval C, Costargent FA, et al. A retrospective survey
of the results of allergen-specific immunotherapy in 205 atopic dogs in
Aquitaine, France (1989–2001). Prat M
ed Chir Anim Comp 2013;48:
41–7.
26 Miller WH, Griffin GE, Campbell KL. Muller & Kirk’s Small Animal
Dermatology. 7th ed. St. Louis: Elsevier; 2013.
27 Borio S, Colombo S, La Rosa G, et al. Effectiveness of a combined (4%
chlorhexidine digluconate shampoo and solution) protocol in MRS and
non-MRS canine superficial pyoderma: a randomized, blinded, antibiotic-
controlled study. Vet Dermatol 2015;26(5):339–44, e72.
28 Loeffler A, Cobb MA, Bond R. Comparison of a chlorhexidine and a
benzoyl peroxide shampoo as sole treatment in canine superficial pyo-
derma. Vet Rec 2011;169(10):249.
29 Halliwell R, Pucheu-Haston CM, Olivry T, et al. Feline allergic diseases:
introduction and proposed nomenclature. Vet Dermatol 2021;32(1):8–e2.
30 Colombo S, Sartori R, Schievano C, et al. Development and validation of
an owner-assessed Visual Analog Scale for feline pruritus severity scoring
(VAScat). Vet Dermatol 2022;33(5):407–13.
31 Hobi S, Linek M, Marignac G, et al. Clinical characteristics and causes of
pruritus in cats: a multicentre study on feline hypersensitivity-associated
dermatoses. Vet Dermatol 2011;22(5):406–13.
32 Santoro D, Pucheu-Haston CM, Prost C, et al. Clinical signs and diagno-
sis of feline atopic syndrome: detailed guidelines for a correct diagnosis.
Vet Dermatol 2021;32(1):26–e6.
33 Moriello KA, Coyner K, Paterson S, et al. Diagnosis and treatment of
dermatophytosis in dogs and cats. Clinical Consensus Guidelines of the
World Association of Veterinary Dermatology. Vet Dermatol 2017;28:
266–e68.
34 Ganz EC, Griffin CE, Keys DA, et al. Evaluation of methylprednisolone
and triamcinolone for the induction and maintenance treatment of pruri-
tus in allergic cats: a double-blinded, randomized, prospective study. Vet
Dermatol 2012;23(5):387–e72.
35 Mueller RS, Nuttall T, Prost C, et al. Treatment of the feline atopic syn-
drome - a systematic review. Vet Dermatol 2021;32(1):43–e8.
36 Walker C. Treatment of Demodex gatoi mange in two sibling Bengal
cats with a combination of selamectin and sarolaner. Comp Anim 2019;24:
127–31.
37 Duangkaew L, Hoffman H. Efficacy of oral fluralaner for the treatment
of Demodex gatoi in two shelter cats. Vet Dermatol 2018;29(3):262.
38 Beccati MB, Pandolfi PP, DiPalma AD. Efficacy of fluralaner spot-on in
cats affected by generalized demodicosis: seven cases [abstract]. Vet Der-
matol 2019;30:454.
39 Ordeix L. Complications of cutaneous skin allergies (skin infections). In:
Noli C, Foster A, Rosenkrantz W, eds. Veterinary Allergy. 1st ed. Oxford:
John Wiley & Sons; 2014:217–22.
40 Ordeix L, Galeotti F, Scarampella F, et al. Malassezia spp. overgrowth in
allergic cats. Vet Dermatol 2007;18(5):316–23.
41 Bond R, Morris DO, Guillot J, et al. Biology, diagnosis and treatment of
Malassezia dermatitis in dogs and cats. Clinical Consensus Guidelines of
the World Association for Veterinary Dermatology. Vet Dermatol 2020;
31(1):28–74.
42 Plumb DC. Plumb’s Veterinary Drug Handbook. 9th ed. Wiley-Blackwell;
2018.
43 Noli C, Beltrando G. The usefulness of a hydrolysed fish and rice starch
elimination diet for the diagnosis of adverse food reactions in cats: an
open clinical trial. Vet Dermatol 2021;32(4):326–e90.
44 Vogelnest LJ, Cheng KY. Cutaneous adverse food reactions in cats: retro-
spective evaluation of 17 cases in a dermatology referral population
(2001-2011). Aust Vet J 2013;91(11):443–51.
45 Scott D, Miller W. Cutaneous food allergy in cats: a retrospective study
of 48 cases (1988-2003). Jap J Vet Dermatol 2013;19:203–10.
JAAHA.ORG 29
46 Olivry T, Mueller RS, Pr
elaud P. Critically appraised topic on adverse
food reactions of companion animals (1): duration of elimination diets.
BMC Vet Res. 2015;11:225.
47 Maine IR, Atterbury R, Chang KC. Investigation into the animal species
contents of popular wet pet foods. Acta Vet Scand 2015;57(1):7.
48 Kanakubo K, Fascetti AJ, Larsen JA. Determination of mammalian
deoxyribonucleic acid (DNA) in commercial vegetarian and ve gan
diets for dogs and cats. J Anim Physiol Anim Nutr (Berl) 2017;101:
70–4.
49 Hanna B. Earlier dermatology referral rewards primary care practice
(part 1): easing client expenses and enhancing patient care. DVM360
2022. Available at: https://www.dvm360.com/view/earlier-dermatology-
referral-rewards-primary-care-practice-part-1-easing-client-expenses-and-
enhancing-patient-care. Accessed May 24, 2023.
50 Saridomichelakis MN, Farnaki R, Leontides LS, et al. Aetiology of canine
otitis externa: a retrospective study of 100 cases. Vet Dermatol 2007;18(5):
341–7.
51 Paterson S. Discovering the causes of otitis externa. In Practice 2016;38:
7–11.
52 Ravens PA, Xu BJ, Vogelnest LJ. Feline atopic dermatitis: a retrospective
study of 45 cases (2001-2012). Vet Dermatol 2014;25:95–102, e27–8.
53 Ngo J, Taminiau B, Fall PA, et al. Ear canal microbiota – a comparison
between healthy dogs and atopic dogs without clinical signs of otitis
externa. Vet Dermatol 2018;29(5):425–e140.
54 Logas D, Maxwell EA. Collaborative care improves treatment outcomes
for dogs with chronic otitis externa: A collaborative care coalition study.
JAmAnimHospAssoc2021;57(5).
55 Fingland RB, Stone LR, Read EK, Moore RM. Preparing veterinary students
for excellence in general practice: building confide nce and competence by
focusing on spectrum of care. JAmVetMedAssoc2021;259(5):463–70.
56 Nationwide. Skin allergies, ear infections among most common condi-
tions that prompt veterinary visits. Nationwide 2022. Available at: https://
news.nationwide.com/commo n-pet-c onditions-that-prompt-veterinary-
visits. Accessed February 6, 2023.
57 Hanna B. Earlier dermatology referral rewards primary care practice
(part 2): boosting client perceptions. DVM360 2022. Available at: https://
www.dvm360.com/view/earlier-dermatology-referral-rewards-primary-
care-practice-part-2-boosting-client-perceptions. Accessed May 24, 2023.
30 JAAHA | 59:6 Nov/Dec 2023
