
Promoting Health and
Preventing Disease and Injury
Through Workplace Tobacco Policies
CURRENT INTELLIGENCE BULLETIN 67
DEPARTMENT OF HEALTH AND HUMAN SERVICES
Centers for Disease Control and Prevention
National Institute for Occupational Safety and Health
On the cover: e cover design includes a wispy background image intended to evoke the well-known health
hazard of smoke associated with the use of combustible tobacco products, and the much less studied misty
emissions associated with the use of electronic devices to “vape” liquids containing nicotine and other com-
ponents. e full range of hazards associated with tobacco use extends well beyond such air contaminants, so
the cover design also incorporates a text box to highlight the optimal “Tobacco-Free” (i.e., not just “Smoke-
Free”) status for both workplaces and workers. e text box also evokes the NIOSH Total Worker Health
TM
strategy. is strategy maintains a strong focus on protection of workers against occupational hazards,
including exposure to secondhand tobacco smoke on the job, while additionally encompassing workplace
health promotion to target lifestyle risk factors, including tobacco use by workers. Photo by ©inkstock.

Current Intelligence Bulletin 67
Promoting Health and
Preventing Disease and Injury
Through Workplace Tobacco Policies
DEPARTMENT OF HEALTH AND HUMAN SERVICES
Centers for Disease Control and Prevention
National Institute for Occupational Safety and Health
Robert M. Castellan, MD, MPH; L. Casey Chosewood, MD; Douglas Trout, MD;
Gregory R. Wagner, MD; Claire C. Caruso, PhD, RN, FAAN; Jacek Mazurek,
MD, MS, PhD; Susan H. McCrone, PhD, RN; David N. Weissman, MD

ii
NIOSH CIB 67
•
Workplace Tobacco Policies
This document is in the public domain and may be freely copied
or reprinted.
Disclaimer
Mention of any company or product does not constitute endorsement by the National In-
stitute for Occupational Safety and Health (NIOSH). In addition, citations to websites ex-
ternal to NIOSH do not constitute NIOSH endorsement of the sponsoring organizations
or their programs or products. Furthermore, NIOSH is not responsible for the content of
these websites. All Web addresses referenced in this document were accessible as of the
publication date.
Ordering Information
To receive documents or other information about occupational safety and health topics,
contact NIOSH at
Telephone: 1–800–CDC–INFO (1–800–232–4636)
TTY: 1–888–232–6348
CDC INFO: www.cdc.gov/info
or visit the NIOSH website at www.cdc.gov/niosh.
For a monthly update on news at NIOSH, subscribe to NIOSH eNews by visiting www.cdc.
gov/niosh/eNews.
Suggested Citation
NIOSH [2015]. Current intelligence bulletin 67: promoting health and preventing disease
and injury through workplace tobacco policies. By Castellan RM, Chosewood LC, Trout D,
Wagner GR, Caruso CC, Mazurek J, McCrone SH, Weissman DN. Morgantown, WV: U.S.
Department of Health and Human Services, Centers for Disease Control and Prevention,
National Institute for Occupational Safety and Health, DHHS (NIOSH) Publication No.
2015-113, http://www.cdc.gov/niosh/docs/2015-113/.
DHHS (NIOSH) Publication No. 2015–113
April 2015
Safer • Healthier • People
TM
iii
NIOSH CIB 67
•
Workplace Tobacco Policies
Foreword
Current Intelligence Bulletins (CIBs) are issued by the National Institute for Occupational
Safety and Health (NIOSH) to disseminate new scientic information about occupational
hazards. A CIB may draw attention to a formerly unrecognized hazard, report new data on
a known hazard, or disseminate information about hazard control.
Public health eorts to prevent disease caused by tobacco use have been underway for the
past half century, but more remains to be done to achieve a society free of tobacco-
related death and disease. e Centers for Disease Control and Prevention (CDC), of which
NIOSH is a part, has recently proclaimed a “Winnable Battle” to reduce tobacco use. NIOSH
marks a half century since the rst Surgeon General’s Report on the health consequences of
smoking by disseminating this CIB 67, Promoting Health and Preventing Disease and Injury
through Workplace Tobacco Policies.
Workers who use tobacco products, or who are employed in workplaces where smoking
is allowed, are exposed to carcinogenic and other toxic components of tobacco and to-
bacco smoke. Cigarette smoking is becoming less frequent, and smoke-free and tobacco-
free workplace policies are reducing exposure to secondhand smoke (SHS) and motivating
smokers to quit—but millions of workers still smoke, and smoking is still permitted in
many workplaces. Other forms of tobacco also represent a health hazard to workers who
use them. In addition to direct adverse eects of tobacco on the health of workers who use
tobacco products or are exposed to SHS, tobacco products used in the workplace—and
away from work—can worsen the hazardous eects of other workplace exposures.
is CIB addresses the following aspects of tobacco use:
• Tobacco use among workers.
• Exposure to secondhand smoke in workplaces.
• Occupational health and safety concerns relating to tobacco use by workers.
• Existing occupational safety and health regulations and recommendations prohibit-
ing or limiting tobacco use in the workplace.
• Hazards of worker exposure to SHS in the workplace.
• Interventions aimed at eliminating or reducing these hazards.
is CIB concludes with NIOSH recommendations on tobacco use in places of work and
tobacco use by workers.
NIOSH urges all employers to embrace a goal that all their workplaces will ultimately be made
and maintained tobacco-free. Initially, at a minimum, employers should take these actions:
• Establish their workplaces as smoke-free (encompassing all indoor areas without ex-
ceptions, areas immediately outside building entrances and air intakes, and all work
vehicles).
iv
NIOSH CIB 67
•
Workplace Tobacco Policies
• Assure compliance with OSHA and MSHA regulations that prohibit or otherwise re-
strict smoking, smoking materials, and/or use of other tobacco products in desig-
nated hazardous work areas.
• Provide cessation support for their employees who continue to use tobacco products.
• Doing all this will help fulll employers’ fundamental obligation to provide safe work-
places, and these actions can improve the health and well-being of their workers.
John Howard, M.D.
Director, National Institute for Occupational
Safety and Health
Centers for Disease Control and Prevention
v
NIOSH CIB 67
•
Workplace Tobacco Policies
Executive Summary
Introduction
Various NIOSH criteria documents on individual hazardous industrial agents, from asbes-
tos [NIOSH 1972] through hexavalent chromium [NIOSH 2013a], have included specic
recommendations relating to tobacco use, along with other recommendations to eliminate
or reduce occupational safety and health risks. In addition, NIOSH has published two Cur-
rent Intelligence Bulletins focused entirely on the hazards of tobacco use. CIB 31, Adverse
Health Eects of Smoking and the Occupational Environment, outlined how tobacco use—
most commonly smoking—can increase risk, sometimes profoundly, of occupational dis-
ease and injury [NIOSH 1979]. In that CIB, NIOSH recommended that smoking be cur-
tailed in workplaces where those other hazards are present and that worker exposure to
those other occupational hazards be controlled. CIB 54, Environmental Tobacco Smoke in
the Workplace: Lung Cancer and Other Health Eects, presented a determination by NIOSH
that secondhand smoke (SHS) causes cancer and cardiovascular disease [NIOSH 1991]. In
that CIB, NIOSH recommended that workplace exposures to SHS be reduced to the lowest
feasible concentration, emphasizing that eliminating tobacco smoking from the workplace
is the best way to achieve that. is current CIB 67, Promoting Health and Preventing Disease
and Injury rough Workplace Tobacco Policies, augments those two earlier NIOSH CIBs.
Consistent with the philosophy embodied in the NIOSH Total Worker Health™ Program
[NIOSH 2013b], this CIB is aimed not just at preventing occupational injury and illness
related to tobacco use, but also at improving the general health and well-being of workers.
Smoking and Other Tobacco Use by Workers—
Exposure to Secondhand Smoke at Work
Millions of workers use tobacco products. Since publication of the rst Surgeon General’s
Report on the health consequences of smoking, cigarette smoking prevalence in the United
States has declined by more than 50% among all U.S. adults—from about 42% in 1965 to
about 18% in 2013 [DHHS 2014; CDC 2014d]. Overall, smoking among workers has simi-
larly declined, but smoking rates among blue-collar workers have been shown to be consis-
tently higher than among white-collar workers. Among blue-collar workers, those exposed
to higher levels of workplace dust and chemical hazards are more likely to be smokers [Chin
et al. 2012]. Also, on average, blue-collar smokers smoke more heavily than white-collar
smokers [Fujishiro et al. 2012].
From 2004–2011, cigarette smoking prevalence varied widely by industry, ranging from
about 10% in education services to more than 30% in construction, mining, and accom-
modation and food services. Smoking prevalence varies even more by occupation, ranging
from 2% among religious workers to 50% among construction trades helpers [NIOSH
2014]. A recent survey of U.S. adults found that by 2013, approximately 1 in 3 current
vi
NIOSH CIB 67
•
Workplace Tobacco Policies
smokers reported ever having used e-cigarettes, a type of electronic nicotine delivery sys-
tem (ENDS) [King et al. 2015]. However, the prevalence of ENDS use by industry and occu-
pation has not been studied. Overall, about 3% of all workers use smokeless tobacco in the
form of chewing tobacco and snu, but smokeless tobacco use exceeds 10% among workers
in construction and extraction jobs and stands at nearly 20% among workers in the mining
industry [NIOSH 2014]. e use of smokeless tobacco by persons who also smoke tobacco
products—one form of what is known as “dual use”—is a way some workers maintain their
nicotine habit in settings where smoking is prohibited (e.g., in an oce where indoor smok-
ing is prohibited or in coal mines where smoking can cause explosions). More than 4% of
U.S. workers who smoke cigarettes also use smokeless tobacco [CDC 2014b; NIOSH 2014].
e implementation of smoke-free policies has eliminated or substantially decreased ex-
posure to SHS in many U.S. workplaces. But millions of nonsmoking workers not covered
by these policies are still exposed to SHS in their workplace. A 2009–2010 survey found
that 20.4% of nonsmoking U.S. workers experienced exposure to SHS at work on at least 1 day
during the preceding week [King et al. 2014]. Another survey conducted at about the
same time estimated that 10.0% of nonsmoking adult U.S. workers experienced exposure
to SHS at work on at least 2 days per week during the past year [Calvert et al. 2013]. Such
exposure varied by industry (ranging from 4% for nance and insurance to nearly 28%
for mining) and by occupation (ranging from 2% for education, training, and library oc-
cupations to nearly 29% for construction and extraction occupations). Inclusion of ENDS
in smoke-free policies has increased over time. In the United States, the number of states
and localities that explicitly prohibited use of e-cigarettes in public places where tobacco
smoking was already prohibited totaled 3 states and more than 200 localities before the
end of 2014 [CDC 2014c].
Health and Safety Consequences of Tobacco Use
Since the rst Surgeon General’s report on smoking and health, many reports from the Sur-
geon General and other health authorities have documented serious health consequences
of smoking tobacco, exposure to secondhand smoke (SHS), and use of smokeless tobacco.
Smoking is a known cause of the top fıve health conditions impacting the U.S. popula-
tion—heart disease, cancer, cerebrovascular disease, chronic lower respiratory disease, and
unintentional injuries [DHHS 2004, 2014]. Smoking also causes a variety of other diseases,
as well as adverse reproductive eects [DHHS 2004, 2014]. Smoking is responsible for more
than 480,000 premature deaths each year in the U.S. [DHHS 2014]. e risk of most ad-
verse health outcomes caused by smoking is related to the duration and intensity of tobacco
smoking, but no level of tobacco smoking is risk free [DHHS 2010b, 2014].
Likewise, there is no risk-free level of exposure to SHS [DHHS 2006, 2014]. SHS exposure
causes more than 41,000 deaths each year among U.S. nonsmokers [DHHS 2014]. Among
exposed adults, there is strong evidence of a causal relationship between exposure to SHS
and a number of adverse health eects, including lung cancer, heart disease (including
heart attacks), stroke, exacerbation of asthma, and reduced birth weight of ospring (due
to SHS exposure of nonsmoking pregnant women) [DHHS 2006, 2014; IARC 2009; IOM
2010; Henneberger et al. 2011]. In addition, there is suggestive evidence that exposure to
SHS causes a range of other health eects among adults, including other cancers (breast
cancer, nasal cancer), asthma, chronic obstructive pulmonary disease (COPD), and pre-
mature delivery of babies born to women exposed to SHS [DHHS 2006, 2014; IARC 2009].
vii
NIOSH CIB 67
•
Workplace Tobacco Policies
Because ENDS are relatively new products that vary widely and have not been well studied,
limited data are available on potential hazardous eects of active and passive exposures to
their emissions [Brown and Cheng 2014; Orr 2014; Bhatnagar et al. 2014]. A recent white
paper from the American Industrial Hygiene Association thoroughly reviewed the ENDS
issue and cautioned that “… the existing research does not appear to warrant the conclusion
that e-cigarettes are “safe” in absolute terms … e-cigarettes should be considered a source of
volatile organic compounds (VOCs) and particulates in the indoor environment that have
not been thoroughly characterized or evaluated for safety” [AIHA 2014].
Smokeless tobacco is known to cause several types of cancer, including oral, esophageal,
and pancreatic cancers [IARC 2012]. Some newer smokeless tobacco products (e.g., snus)
are processed in a way intended to substantially reduce toxicant and carcinogen content,
though variable residual levels remain even in these newer products and represent poten-
tial risk to users [Stepanov et al. 2008]. All smokeless tobacco products contain nicotine, a
highly addictive substance which is plausibly responsible for high risks of adverse repro-
ductive outcomes (e.g., low birth weight, pre-term delivery, and stillbirth) associated with
maternal use of snus [DHHS 2014].
Combining Tobacco Use and Occupational
Hazards Enhances Risk
Many workers and their employers do not fully understand that tobacco use in their work-
places (most commonly smoking) can increase—sometimes profoundly—the likelihood
and/or the severity of occupational disease and injury caused by other hazards present. is
can occur in various ways. A toxic industrial chemical present in the workplace can also be
present in tobacco products and/or tobacco smoke, so workers who smoke or are exposed
to SHS are more highly exposed and placed at greater risk of the occupational disease as-
sociated with those chemicals.
Heat generated by smoking tobacco in the workplace can transform some workplace
chemicals into more toxic chemicals, placing workers who smoke at greater risk of toxicity
[NIOSH 1979; DHEW 1979b; DHHS 1985]. Tobacco products can readily become con-
taminated by toxic workplace chemicals, through contact of the tobacco products with un-
washed hands or contaminated surfaces and through deposition of airborne contaminants
onto the tobacco products. Subsequent use of the contaminated tobacco products, whether
at or away from the workplace, can facilitate entry of these toxic agents into the user’s body
[NIOSH 1979; DHEW 1979b].
Oen, a health eect can be independently caused by tobacco use and by workplace ex-
posure to a toxic agent. For example, tobacco smoking can reduce a worker’s lung func-
tion, leaving that worker more vulnerable to the eect of any similar impairment of lung
function caused by occupational exposure to dusts, gases, or fumes [NIOSH 1979; DHEW
1979b; DHHS 1985]. For some occupational hazards, the combined impact of tobacco use
and exposure to a toxic occupational agent can be synergistic (i.e., amounting to an eect
profoundly greater than the sum of each independent eect). An example is the combined
synergistic eect of tobacco smoking and asbestos exposure on lung cancer, which results
in a profoundly increased risk of lung cancer among asbestos-exposed workers who smoke
[NIOSH 1979; DHEW 1979b; IARC 2004; Frost et al. 2011; Markowitz et al. 2013]
.
viii
NIOSH CIB 67
•
Workplace Tobacco Policies
e risk of occupational injuries and traumatic fatalities can be greatly enhanced when
tobacco use is combined with an occupational hazard. Obvious examples are explosions
and res when explosive or ammable materials in the workplace are ignited by sources as-
sociated with tobacco smoking [MSHA 2000; OSHA 2013a]. However, any form of tobacco
use may result in traumatic injury if the worker operating a vehicle or industrial machinery
is distracted by tobacco use (e.g., while opening, lighting, extinguishing, or disposing of a
tobacco product) [NIOSH 1979].
Preventive Interventions
Both health and economic considerations can motivate people to quit tobacco use. Work-
ers who smoke can protect their own health by quitting tobacco use and can protect their
coworkers’ health by not smoking in the workplace. Smokers who quit stand to benet -
nancially. Among other savings, they no longer incur direct costs associated with consumer
purchases of tobacco products and related materials, and they generally pay lower life and
health insurance premiums and lower out-of-pocket costs for health care.
Legally determined employer responsibilities set out in federal, state, and local laws and
regulations, as well as health and economic considerations, can motivate employers to
establish workplace policies that prohibit or restrict tobacco use. Even where smoke-free
workplace policies are not explicitly mandated by state or local governments, the general
duty of employers to provide safe work environments for their employees can motivate
employers to prohibit smoking in their workplaces, thereby avoiding liability for exposing
nonsmoking employees to SHS [Zellers et al. 2007]. Also, not only are nonsmoking workers
generally healthier, but they are more productive and less costly for employers. Considering
aggregate cost and productivity impacts, one recent study estimated that the annual cost
to employ a smoker was, on average, nearly $6,000 greater than the cost to employ a non-
smoker [Berman et al. 2013]. It follows that interventions that help smoking workers quit
can benet the bottom line of a business.
Several studies have shown that smoke-free workplace policies decrease exposure of non-
smoking employees to SHS at work, increase smoking cessation, and decrease smoking
rates among employees [Fichtenberg and Glantz 2002; Bauer et al. 2005; DHHS 2006; IARC
2009; Hopkins et al. 2010]. Less restrictive workplace smoking policies are associated with
higher levels of sustained tobacco use among workers [IARC 2009]. In workplaces without
a workplace rule that limits smoking, workers are signicantly more likely to be smokers
[Ham et al. 2011]. Policies that make indoor workplaces smoke-free result in improved
worker health [IARC 2009; Callinan et al. 2010]. For example, smoke-free policies in the
hospitality industry have been shown to improve health among bar workers, who are oen
heavily exposed to SHS in the absence of such policies [Eisner et al. 1998; DHHS 2006;
IARC 2009]. Smoke-free policies also reduce hospitalizations for heart attacks in the gen-
eral population [IARC 2009; IOM 2010; Tan and Glantz 2012; DHHS 2014] and several
recent studies suggest that these policies may also reduce hospitalizations and emergency
department visits for asthma in the general population [Hahn 2010; Mackay et al. 2010; Tan
and Glantz 2012; Herman and Walsh 2011]. e CDC-administered Task Force on Com-
munity Preventive Services recommends smoke-free workplace policies, not only to reduce
exposure to SHS, but also to increase tobacco cessation, reduce tobacco use prevalence, and
reduce tobacco-related morbidity and mortality [Hopkins et al. 2010; Task Force on Com-
munity Preventive Services 2010; GCPS 2012a].
ix
NIOSH CIB 67
•
Workplace Tobacco Policies
Some employers have taken action to extend restrictions on tobacco use by their employ-
ees beyond the workplace, for example by prohibiting smoking by workers during their
workday breaks, when away from the workplace, including during lunchtime. Several large
employers have gone further by barring the hiring of smokers. Such wide-ranging poli-
cies generate substantial controversy and are illegal in some jurisdictions [Asch et al. 2013;
Schmidt et al. 2013].
Workplace Tobacco Use Cessation Programs
Employees who smoke and want to quit can benet from employer-provided resources
and assistance. Various levels and types of cessation support can be provided to workers,
though more intensive intervention has a greater eect [Clinical Practice Guideline 2008].
Occupational health providers and worksite health promotion sta can increase quit rates
simply by asking about a worker’s tobacco use and oering brief counseling [O’Hara et al.
1993; Clinical Practice Guideline 2008]. Workers who smoke can be referred to publicly
funded state quitlines, which have been shown to increase tobacco cessation success [GCPS
2012b; Clinical Practice Guideline 2008]. Widespread availability, ease of accessibility, af-
fordability, and potential reach to populations with higher levels of tobacco use make quit-
lines an important component of any cessation eort [Clinical Practice Guideline 2008].
However, many employers do not make their employees aware of them [Hughes et al. 2011].
Mobile phone texting interventions and web-based interventions are also promising ap-
proaches to assist with tobacco cessation [Graham et al. 2007; Clinical Practice Guideline
2008; Whittaker et al. 2011; Civljak et al. 2013]. e most comprehensive workplace cessa-
tion programs incorporate tobacco cessation support into programs that address the overall
safety, health, and well-being of workers. A growing evidence base supports the enhanced
eectiveness of workplace health promotion programs when they are combined with oc-
cupational health protection programs [Sorensen et al. 2003; Barbeau et al. 2006; Hymel et
al. 2011; NIOSH 2013b].
Health Insurance and Smoking—Using Incentives
and Disincentives to Modify Tobacco Use Behavior
Many workers are covered by employer-provided health insurance, which is increasingly
being designed to encourage and help employees to adopt positive personal health-related
behaviors, including smoking cessation for smokers. Health insurance coverage of evi-
dence-based smoking cessation treatments is associated with increases in the number of
smokers who attempt to quit, use proven treatments in these attempts, and succeed in quit-
ting [Clinical Practice Guideline 2008]. Ideally, such coverage should provide access to all
evidence-based cessation treatments, including individual, group, and telephone counsel-
ing, and all seven FDA-approved cessation medications, while eliminating or minimizing
barriers such as cost-sharing and prior authorization [Clinical Practice Guideline 2008;
CDC 2014b].
e Aordable Care Act (ACA), Public Law 111-148, includes provisions pertinent to to-
bacco use and cessation [McAfee et al. 2015]. Some of these provisions are intended to
help smokers quit by increasing their access to proven cessation treatments. Other ACA
provisions are intended to encourage tobacco cessation by permitting small-group plans
to charge tobacco users premiums that are up to 50% higher than those charged to non-
tobacco users, subject certain limitations [78 Fed. Reg. 33158].
x
NIOSH CIB 67
•
Workplace Tobacco Policies
e appropriate intent of incentives is to help employees who use tobacco quit, thus im-
proving health and reducing health-care costs overall. e evidence for the eectiveness
of imposing insurance premium surcharges on tobacco users is limited, and care is need-
ed to ensure that incentive programs are designed to work as intended and to minimize
the potential use of incentives in an unduly coercive or discriminatory manner [Madison
et al. 2011, 2013]. e Task Force on Community Preventive Services has recommended
worksite-based incentives and competitions that are combined with other evidence-based
interventions (e.g., education, group support, telephonic counseling, self-help materials,
smoke-free workplace policies) as part of a comprehensive cessation program [GCPS 2005].
Conclusions
• Cigarette smoking by workers and SHS exposure in the workplace have both declined
substantially over recent decades, but about 20% of all U.S. workers still smoke and
about 20% of nonsmoking workers are still exposed to SHS at work.
• Smoking prevalence among workers varies widely by industry and occupation, ap-
proaching or exceeding 30% in construction, mining, and accommodation and food
services workers.
• Prevalence of ENDS use by occupation and industry has not been studied, but ENDS
has grown greatly, with about 1 in 3 current U.S. adult smokers reporting ever having
used e-cigarettes by 2013.
• Smokeless tobacco is used by about 3% of U.S. workers overall, but smokeless tobacco
is used by more than 10% workers in construction and extraction jobs and by nearly
20% of workers in the mining industry, which can be expected to result in disparities
in tobacco-related morbidity and mortality.
• Tobacco use causes debilitating and fatal diseases, including cancer, respiratory dis-
eases, and cardiovascular diseases. ese diseases aict mainly users, but they also
occur in those exposed to SHS. Smoking is substantially more hazardous, but use of
smokeless tobacco also causes adverse health eects. More than 16 million U.S. adults
live with a disease caused by smoking, and each year nearly a half million die prema-
turely from smoking or exposure to SHS.
• Tobacco use is associated with increased risk of injury and property loss due to re,
explosion, and vehicular collisions.
• Tobacco use by workers can increase, sometimes profoundly, the likelihood and the
severity of occupational disease and injury caused by other workplace hazards (e.g.,
lead, asbestos, and ammable materials).
• Restrictions on smoking and tobacco use in specic work areas where particular
high-risk occupational hazards are present (e.g., explosives, highly ammable materi-
als, or highly toxic materials that could be ingested via tobacco use) have long been
used to protect workers.
• A risk-free level of exposure to SHS has not been established, and ventilation is insuf-
cient to eliminate indoor exposure to SHS.
• Potential adverse health eects associated with using ENDS or secondhand exposure
to particulate aerosols and gases emitted from ENDS remains to be fully characterized.
xi
NIOSH CIB 67
•
Workplace Tobacco Policies
• Policies that prohibit tobacco smoking throughout the workplace (i.e., smoke-free
workplace policies) are now widely implemented, but they have not yet been univer-
sally adopted across the United States. ese policies improve workplace air qual-
ity, reduce SHS exposure and related health eects among nonsmoking employees,
increase the likelihood that workers who smoke will quit, decrease the amount of
smoking during the working day by employees who continue to smoke, and have an
overall impact of improving the health of workers (i.e., among both nonsmokers who
are no longer exposed to SHS on the job and smokers who quit).
• Workplace-based eorts to help workers quit tobacco use can be easily integrated into
existing occupational health and wellness programs. Even minimal counseling and/or
simple referral to state quitlines, mobile phone texting interventions, and web-based
intervention can be eective, and more comprehensive programs are even more ef-
fective.
• Integrating both occupational safety and health protection components into work-
place health promotion programs (e.g., smoking cessation) can increase participation
in tobacco cessation programs and successful cessation among blue-collar workers.
• Smokers, on average, are substantially more costly to employ than nonsmokers.
• Some employers have policies that prohibit employees from using tobacco when away
from work or that bar the hiring of smokers or tobacco users. However, the ethics
of these policies remain under debate, and they may be legally prohibited in some
jurisdictions.
Recommendations
NIOSH recommends that employers take the following actions related to employ-
ee tobacco use:
• At a minimum, establish and maintain smoke-free workplaces that protect those in
workplaces from involuntary, secondhand exposures to tobacco smoke and airborne
emissions from e-cigarettes and other electronic nicotine delivery systems. Ideally,
smoke-free workplaces should be established in concert with tobacco cessation sup-
port programs. Smoke-free zones should encompass (1) all indoor areas without ex-
ceptions (i.e., no indoor smoking areas of any kind, even if separately enclosed and/
or ventilated), (2) all areas immediately outside building entrances and air intakes,
and (3) all work vehicles. Additionally, ashtrays should be removed from these areas.
• Optimally, establish and maintain entirely tobacco-free workplaces, allowing no use
of any tobacco products across the entire workplace campus (see model policy in
Box 6-1).
• Comply with current OSHA and MSHA regulations that prohibit or limit smoking,
smoking materials, and/or use of other tobacco products in work areas characterized
by the presence of explosive or highly ammable materials or potential exposure to
toxic materials (see Table A-3 in the Appendix). To the extent feasible, follow all simi-
lar NIOSH recommendations (see Table A-2 in the Appendix).
• Provide information on tobacco-related health risks and on benets of quitting to all
employees and other workers at the worksite (e.g., contractors and volunteers).
ȣ Inform all workers about health risks of tobacco use.
ȣ Inform all workers about health risks of exposure to SHS.
ȣ Train workers who are exposed or potentially exposed to occupational hazards at
work about increased health and/or injury risks of combining tobacco use with
exposure to workplace hazards, about what the employer is doing to limit the
risks, and about what the worker can do to limit his/her risks.
• Provide information on employer-provided and publicly available tobacco cessation
services to all employees and other workers at the worksite (e.g., contractors and vol-
unteers).
ȣ At a minimum, include information on available quitlines, mobile phone texting
interventions, and web-based cessation programs, self-help materials, and
employer-provided cessation programs and tobacco-related health insurance
benets available to the worker.
ȣ Ask about personal tobacco use as part of all occupational health and
wellness program interactions with individual workers and promptly provide
encouragement to quit and guidance on tobacco cessation to each worker
identied as a tobacco user and to any other worker who requests tobacco
cessation guidance.
• Oer and promote comprehensive tobacco cessation support to all tobacco-using
workers and, where feasible, to their dependents.
ȣ Provide employer-sponsored cessation programs at no cost or subsidize cessation
programs for lower-wage workers to enhance the likelihood of their participation.
If health insurance is provided for employees, the health plan should provide
comprehensive cessation coverage, including all evidence-based cessation
treatments, unimpeded by co-pays and other nancial or administrative barriers.
ȣ Include occupational health protection content specic to the individual
workplace in employer-sponsored tobacco cessation programs oered to workers
with jobs involving potential exposure to other occupational hazards.
• Become familiar with available guidance (e.g., CDC’s “Implementing a Tobacco-Free
Campus Initiative in Your Workplace”) (see Box 6-2) and federal guidance on tobacco
cessation insurance coverage under the ACA (e.g., http://www.dol.gov/ebsa/faqs/faq-
aca19.html) before developing, implementing, or modifying tobacco-related policies,
interventions, or controls.
• Develop, implement, and modify tobacco-related policies, interventions, and controls
in a stepwise and participatory manner. Get input from employees, labor represen-
tatives, line management, occupational safety/health and wellness sta, and human
resources professionals. ose providing input should include current and former to-
bacco users, as well as those who have never used tobacco. Seek voluntary input from
employees with health conditions, such as heart disease and asthma, exacerbated by
exposure to SHS.
• Make sure that any dierential employment benets policies that are based on to-
bacco use or participation in tobacco cessation programs are designed with a primary
intent to improve worker health and comply with all applicable federal, state, and lo-
cal laws and regulations. Even when permissible by law, these dierential employment
benet policies—as well as dierential hiring policies based on tobacco use—should
be implemented only after seriously considering ethical concerns and possible
xiii
NIOSH CIB 67
•
Workplace Tobacco Policies
unintended consequences. ese consequences can include the potential for adverse
impacts on individual employees (e.g., coercion, discrimination, and breach of priva-
cy) and the workforce as a whole. Furthermore, the impact of any dierential policies
that are introduced should be monitored to determine whether they improve health
and/or have unintended consequences.
NIOSH recommends that workers who smoke cigarettes or use other tobacco products take
the following actions:
• Comply with all workplace tobacco policies.
• Ask about available employer-provided tobacco cessation programs and cessation-
related health insurance benets.
• Quit using tobacco products. Know that quitting tobacco use is benecial at any age,
but the earlier one quits, the greater the benets. Many people nd various types
of assistance to be very helpful in quitting, and evidence-based cessation treatments
have been found to increase smokers’ chances of quitting successfully. Workers can
get help from
ȣ tobacco cessation programs, including web-based programs (e.g., http://smokefree.
gov and http://www.cdc.gov/tips) and mobile phone texting services (e.g., the
SmokefreeTXT program, http://smokefree.gov/smokefreetxt);
ȣ state quitlines (phone: 1-800-QUIT-NOW [1-800-784-8669], or 1-855-DEJELO-YA
[1-855-335-3569 for Spanish-speaking callers]); and/or
ȣ health-care providers.
In addition, individual workers who want to quit tobacco may nd several of the websites
listed in Box 6-2 helpful.
NIOSH recommends that all workers, including workers who use tobacco and nonsmokers
exposed to SHS at their workplace:
• know the occupational safety and health risks associated with their work, includ-
ing those that can be made worse by personal tobacco use, and how to limit those
risks; and
• consider sharing a copy of this CIB with their employer.
is page intentionally le blank.
Contents
Foreword ................................................................. iii
Executive Summary ........................................................ v
Introduction .......................................................... v
Smoking and Other Tobacco Use by Workers—Exposure to
Secondhand Smoke at Work
........................................... v
Health and Safety Consequences of Tobacco Use ........................... vi
Combining Tobacco Use and Occupational Hazards Enhances Risk .......... vii
Preventive Interventions ................................................ viii
Workplace Tobacco Use Cessation Programs .............................. ix
Health Insurance and Smoking—Using Incentives
and Disincentives to Modify Tobacco Use Behavior
...................... ix
Conclusions .......................................................... x
Recommendations ..................................................... xi
Abbreviations ............................................................. xvii
Acknowledgments ......................................................... xviii
1 Background ............................................................. 1
2 Tobacco Use by Workers and Secondhand Smoke Exposures at Work ............ 3
Use of Conventional Tobacco Products by Workers ......................... 3
Tobacco Smoking ................................................... 3
Smokeless Tobacco ................................................. 3
Dual Use .......................................................... 4
Secondhand Smoke Exposures at Work ................................... 4
Electronic Nicotine Delivery Systems ..................................... 5
3 Health and Safety Consequences of Tobacco Use .............................. 7
Health Problems Caused by Use of Tobacco Products ....................... 7
Tobacco Smoking ................................................... 7
Secondhand Smoke ................................................. 10
Smokeless Tobacco ................................................. 10
Electronic Nicotine Delivery Systems .................................. 12
Traumatic Injuries and Fatalities Caused by Tobacco Use ................ 13
Tobacco Use and Increased Risk of Work-related Disease and Injury ....... 13
4 Preventive Interventions .................................................. 19
Workplace Policies Prohibiting or Restricting Smoking ..................... 21
Employer Prohibitions on Tobacco Use Extending Beyond the Workplace ..... 24
Workplace Tobacco Use Cessation Programs .............................. 25
xvi
NIOSH CIB 67
•
Workplace Tobacco Policies
Health Insurance and Smoking Behavior .................................. 26
Using Incentives and Disincentives to Modify Tobacco Use Behavior ......... 28
5 Conclusions ............................................................. 31
6 Recommendations ....................................................... 33
References ................................................................ 41
Appendix ................................................................. 57
xvii
NIOSH CIB 67
•
Workplace Tobacco Policies
Abbreviations
ACA Aordable Care Act
CDC Centers for Disease Control and Prevention
CIB Current Intelligence Bulletin
COPD chronic obstructive pulmonary disease
ENDS electronic nicotine delivery system
FDA Food and Drug Administration
MSHA Mine Safety and Health Administration
NHIS National Health Interview Survey
NIOSH National Institute for Occupational Safety and Health
OEL occupational exposure limit
OSHA Occupational Safety and Health Administration
SHS secondhand smoke
SIDS sudden infant death syndrome
xviii
NIOSH CIB 67
•
Workplace Tobacco Policies
Acknowledgments
For contributions to the technical content and review of this document, the authors ac-
knowledge the following NIOSH contributors: Toni Alterman, PhD; Richard J. Driscoll,
PhD, MPH; omas R. Hales, MD, MPH; Candice Johnson, PhD; and Anita L. Schill, PhD,
MPH, MA. From the Oce of Smoking and Health, CDC: Stephen Babb, MPH.
John Lechliter and Seleen Collins provided editorial support, and Vanessa Williams con-
tributed to the design and layout of this document.
e following external peer reviewers provided comments on a dra of this CIB:
William S. Beckett, MD, MPH
Associate Professor of Medicine
Harvard Medical School
Richard A. Daynard, JD, PhD
University Distinguished Professor of Law
Northeastern University School of Law
James A. Merchant, MD, DrPH
Professor of Occupational and Environmental Health
University of Iowa College of Public Health
Kristin M. Madison, JD, PhD
Professor of Law and Health Sciences
Northeastern University School of Law
Jonathan M. Samet, MD, MS
Distinguished Professor andFloraL. ornton Chair
Department of Preventive Medicine
University of Southern California Keck School of Medicine
Comments on a dra of this document were also submitted to the NIOSH docket by in-
terested stakeholders and other members of the public. All comments were considered in
preparing this nal version of the document.
is page intentionally le blank.
is page intentionally le blank.
1
NIOSH CIB 67
•
Workplace Tobacco Policies
1 Background
e widespread recognition that tobacco use is the
leading preventable cause of premature death and
a major cause of preventable disease, injury, and
disability in the United States is based on an ex-
traordinarily strong scientic foundation. e rst
Surgeon General’s report on smoking and health,
issued a half century ago, concluded that cigarette
smoke causes lung cancer and chronic bronchitis
[DHEW 1964]. Subsequent reports of the Surgeon
General have determined that both active tobacco
smoking and secondhand smoke (SHS) exposure
are important causes of cancer, heart disease, and
respiratory disease, and that smokeless tobacco use
also causes serious disease, including oral, esoph-
ageal, and pancreatic cancer [e.g., DHHS 1982;
1983; 1984; 1986a,b; 2004; 2006; 2014]. One Sur-
geon General’s report focused entirely on smoking-
enhanced risks of cancer and chronic lung disease
for workers exposed to hazardous industrial agents
in the workplace [DHHS 1985]. Several reports of
the Surgeon General have addressed benets of
eective smoking cessation programs and other
means of reducing tobacco use [DHHS 1990, 2000,
2012, 2014].
A Surgeon General’s report also established the
ongoing Healthy People strategy, aimed broadly at
improving the nation’s health [DHEW 1979a]. Cur-
rently, Healthy People 2020 includes a major goal of
reducing “illness, disability, and death related to to-
bacco use and secondhand smoke exposure” along
with several specic objectives that target eliminat-
ing tobacco smoking in workplaces [DHHS 2013].
e Centers for Disease Control and Prevention has
declared reducing tobacco use a “Winnable Battle,”
noting that tobacco use is one of several “public
health priorities with large-scale impact on health
and with known, eective strategies to address
them” [CDC 2013a]. e U.S. Department of Health
and Human Services has published a strategic plan
for tobacco control that envisions “a society free of
tobacco-related death and disease” [DHHS 2010a].
Over time, National Institute for Occupation-
al Safety and Health (NIOSH) publications have
evolved in how they have acknowledged and made
recommendations about hazards associated with
tobacco use by workers. e rst criteria document
published by NIOSH—on asbestos—only briey
mentioned smoking. Smoking was addressed in
the context of a discussion of research ndings that
concluded that smoking alone could not explain
the extremely high risk of lung cancer observed in
asbestos-exposed workers. Smoking was also men-
tioned in a suggestion that the medical monitor-
ing recommended by NIOSH for asbestos-exposed
workers would oer opportunity for various forms
of individualized medical management, including
smoking cessation [NIOSH 1972] (see Appendix
Table A-2). Nearly a decade later, aer substantial-
ly more research on asbestos had been published,
NIOSH disseminated a document arming syn-
ergistic (i.e., more than additive) eects on lung
cancer risk of combined exposure to asbestos and
smoking [NIOSH 1980].
In the late 1970s, NIOSH scientists authored a
chapter on “e Interaction between Smoking
and Occupational Exposure” in the 1979 Surgeon
General’s Report on Smoking and Health [DHEW
1979b]. at work led directly to the rst NIOSH
publication focused solely on tobacco smoke, a
Current Intelligence Bulletin (CIB) that outlined
several ways in which tobacco use can increase,
sometimes profoundly, the risk of occupational dis-
ease and injury [NIOSH 1979]. In that CIB, NIOSH
recommended that smoking be curtailed in work-
places where those other hazards are present and
that worker exposure to those other occupational
hazards be controlled (see Appendix Table A-1).
2 3
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Later, when scientic evidence became clear that
the health risk from inhaling tobacco smoke is
not limited to smokers but also aects bystanders,
NIOSH published another CIB focused solely on
tobacco smoke—this one on SHS in the workplace
[NIOSH 1991]. In that CIB, NIOSH presented its
determination that SHS (referred to in that docu-
ment as “environmental tobacco smoke”) causes
cancer and cardiovascular disease. In recommend-
ing that workplace exposures to SHS be reduced to
the lowest feasible concentration using all available
preventive measures, NIOSH emphasized that the
best approach is to eliminate tobacco smoking in
the workplace, and it endorsed employer-provided
smoking cessation programs for employees who
smoke [NIOSH 1991] (see Appendix Table A-1).
In retrospect, the CIB on SHS in the workplace
marked a watershed in the Institute’s approach to
occupational safety and health. Over time, NIOSH
recommendations concerning specic industrial
hazards—which earlier might have been relatively
silent about what were then narrowly understood
to be strictly personal health-related behaviors like
smoking—have come to embrace a more compre-
hensive preventive approach. is evolution has
been motivated by a better understanding of how
tobacco use adversely impacts occupational dis-
eases and injuries and—perhaps just as important-
ly—by a changing societal view of the health and
economic consequences of tobacco use. By way of
example, criteria documents produced in the past
decade on two lung hazards—refractory ceramic
bers [NIOSH 2006] and hexavalent chromium
[NIOSH 2013a]—have included entire sections on
smoking cessation, something not seen in earlier
criteria documents (see Appendix Table A-2). In a
2004 medical journal paper, the Director of NIOSH
concluded that “Smoking is an occupational haz-
ard, both for the worker who smokes and for the
nonsmoker who is exposed to [SHS] in his or her
workplace.” He also recommended that “Smoking
as an occupational hazard should be completely
eliminated for the sake of the health and safety of
American workforce” [Howard 2004]. A 2010 post
on the NIOSH Blog site pointed out that “Tobacco-
free workplaces, on-site tobacco cessation services,
and comprehensive, employer-sponsored health-
care benets that provide multiple quit attempts,
have all been shown to increase tobacco treatment
success” [Howard et al. 2010].
us, instead of staying focused nearly exclusively
on protecting workers from specic occupational
hazards, NIOSH has progressively adopted a “strat-
egy integrating occupational safety and health pro-
tection with health promotion to prevent worker
injury and illness and to advance health and well-
being” [NIOSH 2013b]. is integrated approach,
embodied by NIOSH in its Total Worker Health™
Program [Schill and Chosewood 2013], has mo-
tivated NIOSH to produce this CIB, Promoting
Health and Preventing Disease and Injury through
Workplace Tobacco Policies.
2 3
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
2 Tobacco Use by Workers and Secondhand
Smoke Exposures at Work
Use of Conventional Tobacco
Products by Workers
Tobacco Smoking
Since publication of the rst Surgeon General’s
report on the health consequences of smoking,
cigarette smoking prevalence has decreased sub-
stantially among U.S. adults, from 42.4% in 1965 to
17.8% in 2013 [DHHS 2014; CDC 2014d]. Nation-
ally representative studies on the smoking status of
workers in the United States, most oen based on
one or more iterations of the National Health Inter-
view Survey (NHIS), have demonstrated substan-
tial declines in overall cigarette smoking, which are
similar to the decrease in cigarette smoking among
all U.S. adults [Sterling and Weinkam 1976; Nel-
son et al. 1994; Lee et al. 2004, 2007; Barbeau et al.
2004]. e overall prevalence of current cigarette
smoking among workers during the 2004–2010
period was 19.6%, very closely approximating the
prevalence among all U.S. adults, which annually
ranged from a high of 20.9% to a low of 19.3% dur-
ing the 2004–2010 period [CDC 2011a, 2013b].
During the past several decades, a number of stud-
ies have assessed smoking habits among U.S. work-
ers. Consistently, these studies have shown substan-
tially higher cigarette smoking prevalence among
blue-collar workers compared with white-collar
workers, particularly among males [Sterling and
Weinkam 1976; DHHS 1985; Stellman et al. 1988;
Brackbill et al. 1988; Covey et al. 1992; Nelson et al.
1994; Bang and Kim 2001; Barbeau et al. 2004; Lee
et al. 2004, 2007; CDC 2011a; Calvert et al. 2013].
In addition, these studies provide evidence of high-
er intensity of smoking among blue-collar workers
who smoke than white-collar workers who smoke
[Fujishiro et al. 2012]. Among blue-collar workers,
those with higher levels of exposure to dust and
chemical hazards are more likely to be smokers
[Chin et al. 2012].
NIOSH publishes recent data on cigarette smok-
ing status by industry and occupation groupings
in the Work-Related Lung Disease (WoRLD) Sur-
veillance Report and corresponding online updates
[NIOSH 2008a, 2014]. e most recent tables,
covering the period 2004–2011, show that smok-
ing prevalence varies widely—nearly four-fold—by
industry. Smoking prevalence at or below 10% was
found among major industry sectors in education
services (9.8%) and among minor industry sec-
tors in religious, grantmaking, civic, labor, profes-
sional, and similar organizations (10.0%). Smoking
prevalence exceeding 30% was found among three
major industry sectors: construction (32.1%); ac-
commodation and food services (32.1%); and min-
ing (30.2%). Several minor sectors in other major
industries also exceeded 30%: gasoline stations
(37.6%); shing, trapping, and hunting (34.3%);
forestry and logging (32.9%); warehousing and
storage (32.0%); rental and leasing services (31.3%);
wood product manufacturing (30.7%); and non-
metallic mineral product manufacturing (30.4%).
Additional tables posted on that same NIOSH site
show that cigarette smoking prevalence varies even
more extremely—25-fold—by specic occupation-
al group, from 2.0% for religious workers to 49.5%
for construction trades helpers [NIOSH 2014] (see
Appendix Figures A-1a and A-1b).
Smokeless Tobacco
Smokeless tobacco is not burned when used. Types
of smokeless tobacco include chewing tobacco,
4 5
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
snu, dip, snus, and dissolvable tobacco products.
As with smoking, NHIS data have been used to es-
timate smokeless tobacco use by workers [Dietz et
al. 2011; NIOSH 2014]. During 2010, an estimated
3% of currently working adults used smokeless
tobacco in the form of chewing tobacco or snu.
Smokeless tobacco use ranged up to 11% for those
working in construction and extraction jobs and
more than 18% for those working in the mining in-
dustry [CDC 2014a; NIOSH 2014]. (Appendix Fig-
ures A-2a and A-2b display prevalence of smoke-
less tobacco use for major industry and occupation
categories.)
Dual Use
Someone who smokes cigarettes and also uses
smokeless tobacco engages in “dual use.” is is
one way smokers can try to maintain their nico-
tine habit when and where smoking is prohib-
ited. Based on 2010 NHIS data, more than 4% of
U.S. adult workers who smoke cigarettes also use
smokeless tobacco in the form of snu or chewing
tobacco [CDC 2014a; NIOSH 2014]. Dual use has
traditionally been practiced by many workers, in-
cluding coal miners and others, employed in mines
or factories where smoking poses risks for explo-
sion and re [Mejia and Ling 2010]. (Appendix Fig-
ures A-3a and A-3b display prevalence of dual use
among U.S. adult workers who are current smokers
for major industry and occupation categories, re-
spectively.) Use of electronic cigarettes by persons
who also smoke is another form of “dual use” that
is becoming more prevalent as electronic cigarette
use increases (see below, under “Electronic Nico-
tine Delivery Systems”).
Secondhand Smoke
Exposures at Work
SHS is a mixture of the “sidestream smoke” emitted
directly into the air by the burning tobacco product
and the “mainstream smoke” exhaled by smokers
while smoking. Workplace exposures to SHS have
been demonstrated by using air monitoring and
through the use of biological markers, such as co-
tinine, a metabolite of nicotine [Hammond et al.
1995; Hammond 1999; Achutan et al. 2011; Pache-
co et al. 2012]. By the late 1990s, studies that objec-
tively measured markers of SHS found levels that
varied substantially by workplace. Where smoking
was allowed, oces and blue-collar workplaces had
similar concentrations of nicotine in the air; higher
nicotine concentrations were present in restau-
rants, and still higher concentrations (an order of
magnitude higher than in oces) were measured
in bars [Hammond 1999]. More recently, in studies
involving nonsmoking card dealers at three casinos
where smoking was prevalent, objective evidence
of absorption of a cancer-causing component of
SHS (a tobacco-specic nitrosamine) was docu-
mented by showing signicant increases in urine
levels of a metabolite of that component over a
work shi [Achutan et al. 2011]. A comprehensive
review of research on SHS exposures in casinos has
been published elsewhere [Babb et al. 2015].
Smoke-free workplace policies have been increas-
ingly implemented over the past several decades in
the United States and have been shown to be ef-
fective in reducing exposure to SHS [DHHS 2006,
2014]. In a 1986 survey of the civilian U.S. popu-
lation, only 3% of employed respondents reported
working under a smoke-free workplace policy
[CDC 1988]. Subsequent surveys carried out in
the 1990s tracked an increasing proportion of in-
door workers who reported that they worked un-
der a smoke-free workplace policy—46.5% in 1993,
63.7% in 1996, and 69.3% by 1999 [Shopland et al.
2004]. e 1999 survey found wide disparities; al-
though smoke-free workplace policies covered 90%
of school teachers, they covered only 43% of food
preparation and service workers, and only 13% of
bartenders [Shopland et al. 2004].
Although establishment of smoke-free workplace
policies continues to progress in the United States,
these policies are not always 100% eective. A
2009–2010 nationwide survey found that, among
employed nonsmoking adults in the United States
whose workplaces were covered by an indoor
smoke-free policy, 16.4% reported exposure to
4 5
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
SHS at work 1 or more days during the past 7 days
[King et al. 2014]. Still, this favorably compared
with the much greater 51.3% of those not covered
by smoke-free policies who reported such exposure
to SHS at work [King et al. 2014].
e 2009–2010 nationwide survey also found that
20.4% of nonsmoking employed adults reported
SHS exposure in their indoor workplace on 1 or
more days during the past 7 days [King et al. 2014].
An analysis of recent NHIS data that used a more
restrictive denition of SHS exposure—exposure
to SHS at work on 2 or more days per week dur-
ing the past year—estimated that 10.0% of non-
smoking U.S. workers reported frequent exposure
to SHS at work [Calvert et al. 2013]. Prevalence
of such frequent exposure by major industry sec-
tor ranged from 4.1% for nance and insurance to
28.4% for mining, while prevalence by major oc-
cupation ranged from 2.3% for education, training,
and library occupations to 28.5% for “construction
and extraction” occupations (See Appendix Figures
A-4a and A-4b).
Data from 14 state-based population surveys con-
ducted in 2005 indicated that the majority of all
indoor workers reported a completely smoke-free
workplace policy at their place of employment.
State-specic proportions ranged from 54.8% (Ne-
vada) to 85.8% (West Virginia), with a median of
73.4% [CDC 2006]. Results from later surveys con-
ducted by 13 states in 2008 found proportions of
nonsmoking employed adults who reported SHS
exposure on 2 or more days during the past 7 days
in their indoor workplace ranging from 6.0% (Ten-
nessee) to 15.8% (Mississippi), with a state-specic
median of 8.6% [CDC 2009]. An even more recent
survey involving all states found proportions of
nonsmoking employed adults who reported SHS
exposure on 1 or more days during the past 7 days
in their indoor workplace ranging from 12.4%
(Maine) to 30.8% (Nevada) [King et al. 2014].
Prevalences of SHS exposure at work on 1 or more
days during the past 7 days were signicantly higher
among males (23.8%) than females (16.7%), among
those without a high school diploma (31.9%) than
those with a graduate school degree (11.9%), and
among those with an annual household income less
than $20,000 (24.2%) than those with ≥$100,000
income (14.8%). A recent study separated eects
on workplace SHS exposure associated with educa-
tion and income from eects associated with occu-
pation [Fujishiro et al. 2012]. Even aer statistically
adjusting for the eects of education and income,
blue-collar workers were more likely to report
workplace SHS exposure than managers and pro-
fessionals. at same study also found that blue-
collar workers were also more likely to be smokers
and more likely to be heavy smokers, suggesting
that SHS exposures in the workplace could be in-
tense for many blue-collar workers.
Electronic Nicotine Delivery Systems
First introduced into the U.S. market in 2007 [Re-
gan et al. 2013], electronic nicotine delivery sys-
tems (ENDS), which include electronic cigarettes,
or e-cigarettes, are rapidly increasing in use [King
et al. 2015]. e ENDS marketplace has diversied
in recent years and now includes multiple products,
including electronic hookahs, vape pens, electronic
cigars, and electronic pipes. Typically, an ENDS
product has a cartridge containing a liquid con-
sisting of varying amounts of nicotine, a propylene
glycol and/or glycerin carrier, and avorings. Inha-
lation draws the uid to a heating element, creating
vapor that subsequently condenses into an aerosol
of minute droplets [Ingebrethsen et al. 2012].
Available data suggest that e-cigarette use has in-
creased greatly in the United States during the past
several years. A mail survey of U.S. adults showed
that the percentage who had ever used e-cigarette
more than quadrupled from 0.6% in 2009 to 2.7%
in 2010 [Regan et al. 2013]. A more recent survey
of U.S. adults found that by 2013 approximately 1
in 3 current smokers reported ever having used
e-cigarettes [King et al. 2015]. To date, there have
been no nationally representative surveys of ENDS
use specically among workers or specically in
the workplace.
is page intentionally le blank.

7
NIOSH CIB 67
•
Workplace Tobacco Policies
3 Health and Safety Consequences of
Tobacco Use
Health Problems Caused by
Use of Tobacco Products
Tobacco Smoking
Smoking is a known cause of the top fıve health
conditions impacting the U.S. population—heart
disease, cancer, cerebrovascular disease, chronic
lower respiratory disease, and unintentional inju-
ries [DHHS 2004] (Table 3-1), and each of these is
amenable to preventive intervention [Task Force on
Community Preventive Services 2010]. e risk and
severity of most adverse health outcomes caused by
smoking are directly related to the duration and in-
tensity of tobacco smoking, but no level of tobacco
smoking is risk-free [DHHS 2010b, 2014]. Smok-
ing is responsible for more than 480,000 deaths
each year in the United States [DHHS 2014]. It is
estimated that more than 16 million U.S. adults
live with chronic obstructive pulmonary disease
or other disease attributable to tobacco smoking
[DHHS 2014].
Table 3-1. Some health conditions caused by active tobacco smoking
General disease category Site or specic health condition
Cancers Lung
Bladder
Esophageal
Laryngeal
Oral and throat
Cervical
Kidney
Pancreatic
Liver
Stomach
Colorectal
Acute myeloid leukemia
Cardiovascular disease Atherosclerosis
Coronary heart disease
Cerebrovascular disease (stroke)
Abdominal aortic aneurysm
Lung disease Chronic obstructive pulmonary disease
Acute respiratory infections, including pneumonia
Asthma exacerbation
Tuberculosis
Asthmatic and other respiratory symptoms
Accelerated lung function decline

8 9
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
General disease category Site or specic health condition
Reproductive eects Reduced fertility
Placental abnormalities
Ectopic pregnancy
Impaired fetal development and congenital orofacial
defects
Premature delivery
Low birth weight
Sudden infant death syndrome (SIDS)
Erectile dysfunction
Other diseases or conditions Cataracts, macular degeneration, and blindness
Low bone density and hip fractures
Poor wound healing
Peptic ulcer disease
Periodontitis
Diabetes
Rheumatoid arthritis
Impaired immune function
General poor health
Source: DHHS [2004, 2014]
Cancer
Smoking is estimated to cause nearly 164,000 can-
cer deaths among smokers each year in the United
States [DHHS 2014]. Cancers caused by smoking in-
clude lung, mouth, throat, bladder, and other cancers
(Table3-1). Among the carcinogens present in ciga-
rette smoke are polycyclic aromatic hydrocarbons;
N-nitrosamines; aromatic amines; 1,3-butadiene;
benzene; aldehydes; and ethylene oxide. In addition
to directly causing cancer, smoking can synergistically
interact with occupational exposures known to sepa-
rately cause cancer, leading to eects on cancer cau-
sation greater than the eects of the two factors sepa-
rately [Wraith and Mengersen 2007; Frost et al. 2011;
Markowitz et al. 2013] (see Box 3-1).
Cardiovascular Disease
Cigarette smoking is estimated to cause nearly
125,000 heart disease deaths among smokers
each year in the United States [DHHS 2014]. e
constituents of tobacco smoke believed to be re-
sponsible for causing cardiovascular disease include
oxidizing chemicals, nicotine, carbon monoxide,
and particulate matter. Coronary heart disease
(ischemic heart disease) makes up the majority of
those heart disease deaths. Cerebrovascular disease
(vascular disease in the brain), which can cause
strokes, is also a major cause of death from smok-
ing. Smoking also causes aortic aneurysms and pe-
ripheral arterial disease. Smoking is estimated to
cause nearly 27,000 cerebrovascular and peripheral
vascular deaths among smokers each year in the
United States [DHHS 2014]. Even low levels of ex-
posure to tobacco smoke—such as a smoking only
a few cigarettes per day, occasional smoking, or ex-
posure to SHS—are enough to greatly increase risk
of cardiovascular events [DHHS 2010b].
Lung Disease
Cigarette smoking is estimated to cause more than
113,000 deaths among smokers each year in the
Table 3-1 (Continued). Some health conditions caused by active tobacco smoking

8 9
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
United States from non-malignant lung diseases
[DHHS 2014]. Some of the chemical pathways by
which tobacco smoke produces lung damage have
been well characterized. It is likely that familial or
genetic factors inuence susceptibility to the ad-
verse eects of tobacco smoke. Chronic obstructive
pulmonary disease (COPD), a broad designation
encompassing bronchitis, emphysema, and airways
obstruction, accounts for most smoking-caused re-
spiratory deaths. As noted above, the eects of oc-
cupational exposure to agents that are toxic to the
lung can combine with the adverse health eects
of tobacco smoke to cause lung disease of greater
severity than that expected from either of the expo-
sures alone (see Box 3-2). Although smoking is the
single most common cause of COPD, occupational
exposures—oen combined with smoking—play a
role in causing about 10% to 20% of all COPD cases
[Balmes et al. 2003]. In addition, smoking causes
exacerbation of asthma, greater susceptibility to in-
fectious pneumonias, and higher risk of tuberculo-
sis [DHHS 2014].
Reproductive and Developmental Eects
Inhalation of tobacco smoke aects the reproduc-
tive system, with harmful eects related to fertil-
ity, fetal and child development, and pregnancy
outcome. Smoking is estimated to cause more
than 1,000 deaths from perinatal conditions each
year in the United States [DHHS 2014]. Exposure
to the complex chemical mixture of combustion
compounds in tobacco smoke—including carbon
monoxide, which binds to hemoglobin and can
deprive the fetus of oxygen—has been found to
contribute to a wide range of reproductive eects
in women. ese eects include altered menstrual
cycle and reduced fertility; placental abnormalities
and preterm delivery; reduced birth weight, still-
birth, neonatal death, and sudden infant death syn-
drome (SIDS) in their ospring; earlier and more
symptomatic menopause; and other eects [DHHS
2001, 2004, 2014; Soares and Melo 2008; Sadeu et
al. 2010]. Smoking by men causes erectile dysfunc-
tion [McVary et al. 2001; DHHS 2014], which can
also impair reproduction.
Box 3-1. Lung Cancer Risk in Insulators—Eects of Smoking, Asbestos Exposure, and Asbestosis
Cigarette smoking and exposure to asbestos are each well-known causes of lung cancer. Many studies
have assessed lung cancer risk among persons who have both smoking and asbestos exposure as risk
factors. Frost et al. [2011] conrmed the long-standing view that cigarette smoking raises the risk
of death from lung cancer among asbestos-exposed workers in a manner that is greater than addi-
tive, if not multiplicative. Results of the study by Markowitz et al. [2013] illustrate eects of smoking
combined not just with asbestos exposure, but also specically with asbestosis (a brotic lung disease
caused by asbestos). Markowitz et al. reported a long-term mortality study of 2,377 asbestos-exposed
insulators identied in 1967 and 54,243 contemporaneous blue-collar workers with little, if any, as-
bestos exposure. e insulators were divided into two subgroups—one with and the other with-
out radiographic evidence of asbestosis—with roughly equivalent asbestos exposure. Separate lung
cancer risks were 10.3-fold for smoking (without asbestos exposure), 3.6-fold for asbestos exposure
(without smoking), and 7.4-fold for asbestosis (without smoking). Combined lung cancer risks were
14.4-fold for smoking combined with asbestos exposure and 36.5-fold for smoking combined with
asbestosis. e former illustrates an apparent additive eect, because the combined eect was about
what would be expected by adding the separate risks for smoking and asbestos exposure. e latter
illustrates an apparent supra-additive (i.e., synergistic) eect, because the combined eect is substan-
tially greater than what would be expected by adding the separate risks for smoking and asbestosis.

10 11
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Other Adverse Eects
Smoking is known to cause other health problems
that contribute to the generally poorer health of
smokers as a group. ese include visual diculties
(due to cataracts and age-related macular degen-
eration), hip fractures (due to low bone density),
peptic ulcer disease, diabetes, rheumatoid arthritis,
and periodontitis [DHHS 2014] (Table 3-1). Smok-
ing may also cause hearing loss in adults [Cruick-
shanks et al. 1998].
Inammatory eects of tobacco smoke have
been associated with many other health ef-
fects. For example, smoking has been found to
delay wound healing aer surgery and lead to
wound complications [Sorensen 2012]. Also,
tobacco smoking may increase the risk of
hearing loss caused by occupational exposure
to excessive noise [Tao et al. 2013]. Research
on other health eects associated with ex-
posure to tobacco smoke will undoubtedly
provide a more complete understanding of the
adverse health eects of smoking.
Secondhand Smoke
In the United States, SHS exposure causes more
than 41,000 deaths among nonsmokers each year
[DHHS 2014]. ere is strong evidence of a causal
relationship between SHS of adults and adverse
health eects, including lung cancer, heart dis-
ease, stroke, exacerbation of asthma, nasal irrita-
tion, and (due to maternal exposure) reduced birth
weight of ospring (Table 3-2) [DHHS 2006, 2014;
IARC 2009; Henneberger et al. 2011]. e evidence
that exposure to SHS causes health eects among
exposed infants and children is also strong (Table
3-2)[DHHS 2006, 2014; IARC 2009].
ere is also suggestive evidence that exposure to
SHS causes a range of other health eects. ese
include respiratory diseases (asthma, COPD),
breast cancer, and nasal cancer among nonsmok-
ing adults, premature delivery of babies born to
women exposed to SHS, and cancers (leukemia,
lymphoma, brain cancer) among children exposed
to SHS [DHHS 2006, 2014; IARC 2009]. SHS ex-
posure may also be associated with hearing loss in
adults [Fabry et al. 2011].
Among nonsmoking adults, health risks of SHS
exposure extend to workplace exposures. A meta-
analysis of 11 pertinent studies provided quanti-
tative estimates of lung cancer risk attributable to
workplace exposure to SHS; lung cancer risk was
increased by 24% overall among workers exposed
to SHS in the workplace, and there was a doubling
of lung cancer risk among workers categorized as
highly exposed to SHS in the workplace [Stayner et
al. 2007]. A dramatic example of an adverse eect
of exposure to SHS in the workplace was an asth-
matic worker’s death (see Box 3-3).
Smokeless Tobacco
Some forms of smokeless tobacco are well docu-
mented as causes of oral cancer, esophageal cancer,
Box 3-2. Emphysema Risk in Coal Miners—Eects of Tobacco Smoking and Coal Mine Dust Exposure
A study [Kuempel et al. 2009] evaluated the eects of exposure to coal mine dust, cigarette smoking, and
other factors on the severity of lung disease (emphysema) among more than 700 deceased persons, including
more than 600 deceased coal miners. e study found that combined occupational exposure to coal mine
dust and cigarette smoking had an additive eect on the severity of emphysema among the coal miners.
Among smokers and never-smokers alike, emphysema was generally more severe among those who had
higher levels of exposure to coal mine dust. However, at any given level of dust exposure, miners who had
smoked generally had worse emphysema than miners who had not smoked.

10 11
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Box 3-3. Asthma Death and Exposure to Secondhand Smoke—A Case Report
On May 1, 2004, a 19-year-old part-time waitress, who had a history of asthma since childhood,
arrived at work. She spent 15 minutes chatting with a coworker in an otherwise unoccupied room
adjacent to the bar and was reported to have no apparent breathing diculty at that time. She then
entered the bar, which was occupied by dozens of patrons, many of whom were smoking. Less than 5
minutes later she reported to the manager that she wished she had her inhaler with her, needed fresh
air, and needed to get to the hospital. As she walked towards the door, she collapsed. An emergency
medical crew attempted resuscitation and transported her to a hospital emergency room, where she
was declared dead. “Status asthmaticus” and “asphyxia secondary to acute asthma attack’’ were the
causes of death recorded on the death certicate and autopsy report, respectively. e workplace was
described by an investigator from a NIOSH-funded state program as a ‘‘typical smoky bar.” Based on
the nature and circumstances of the waitress’s death, it was concluded by the principal investigator of
the state’s fatality investigation program and his colleagues that this waitress died from exposure to
work-related SHS [MIFACE 2006; Stanbury et al. 2008].
Table 3-2. Health Conditions Caused by Exposure to Secondhand Smoke
Aected population Adverse health eect
Eects on nonsmoking adults Premature death and disease
Lung cancer
Coronary artery disease
Stroke
Asthma exacerbation
Nasal Irritation
Eects on infants/children Premature death and disease
Reduced birth weight (due to maternal SHS exposure)
Sudden infant death syndrome (SIDS)
Slow lung growth and reduced lung function
Lower respiratory illnesses
More severe asthma
Wheeze illnesses
Respiratory symptoms (cough, phlegm, wheeze, breathlessness)
Middle ear disease
Source: DHHS [2006, 2014]; IARC [2009]; Henneberger et al. [2011]
and pancreatic cancer [IARC 2012], though at gen-
erally lower risk levels than those associated with
smoking [DHHS 2014]. e most harmful chemi-
cals in smokeless tobacco are tobacco-specific
nitrosamines, which are formed during the grow-
ing, curing, fermenting, and aging of tobacco. Other
cancer-causing substances in smokeless tobacco in-
clude polonium-210 (a radioactive element found
12 13
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
in tobacco fertilizer and soil) and polynuclear
aromatic hydrocarbons (also known as polycyclic
aromatic hydrocarbons) [DHHS 1986a]. Some
newer smokeless tobacco products (e.g., snus) are
processed in a way intended to substantially reduce
toxicant and carcinogen content, though variable
residual levels remain even in these newer prod-
ucts and represent potential risk to users [Stepanov
et al. 2008]. All smokeless tobacco products con-
tain nicotine, a highly addictive substance which
is plausibly responsible for high risks of adverse
reproductive outcomes (e.g., low birth weight, pre-
term delivery, and stillbirth) associated with mater-
nal use of snus [DHHS 2014].
Electronic Nicotine Delivery Systems
Because ENDS are relatively new products that
vary widely and have not been well studied, limited
data are available on potential hazardous eects
of active and passive exposures to their emissions
[Brown and Cheng 2014; Orr 2014; Bhatnagar et
al. 2014]. Questions remain regarding potential im-
pacts of ENDS use on individual and population
level health. Contrary to some marketing messages,
aerosol emitted from ENDS is not merely water va-
por. Many of the hazardous components identied
in tobacco smoke are present in ENDS emissions,
though mostly at much lower levels. Liquids for-
mulated for ENDS use commonly contain nicotine
and avorings in a propylene glycol and/or glycerin
carrier, but exact formulations of these predomi-
nant constituents and other additives and contami-
nants vary widely and are not well standardized
[Cheng 2014]. In sum, aerosol generated by ENDS
use is not as safe as clean air [CDC 2014c].
Secondhand exposure to nicotine is not with-
out potential risk for bystanders in the vicinity
ENDS use. Nicotine is addictive and is associated
with various systemic toxicities at sucient doses
[NIOSH 2012] and adverse vascular eects at low
doses [DHHS 2010b]. For non-smokers, nicotine is
an acute irritant, capable of causing headache, nau-
sea, and discomfort; for former smokers, nicotine
exposure can trigger cravings jeopardizing their
abstinence [DHHS 2014]. In pregnant women,
nicotine can be transferred to and have toxic ef-
fects on the developing fetus [DHHS 2014]. In ad-
dition, other substances that have been detected or
can be reasonably anticipated in aerosol produced
by ENDS include known carcinogens, respiratory
irritants, and other harmful and potentially harm-
ful constituents [FDA 2009; McAuley et al. 2012;
Schripp et al. 2013; Schober et al. 2014; Schaller et
al. 2013; Bhatnagar et al. 2014; Cheng 2014; Gonie-
wicz et al. 2014; Grana et al. 2014]. A recent review
of the safety of ENDS use concluded that more re-
search is warranted to determine the risk posed by
various components of the liquids used in ENDS,
including avoring components in particular “be-
cause the eects of inhaling avoring substances
approved for food use are largely unknown” [Far-
salinos and Polosa 2014]. Some avorings intended
for ingestion have been shown to cause serious
lung disease when inhaled at high concentrations
in other contexts [NIOSH 2004; CDC 2013c]. Fur-
thermore, beyond the concerns of nonuser expo-
sure to nicotine and these other components, there
is also potential for ENDS to be used to deliver psy-
choactive substances such THC, the active ingredi-
ent in marijuana [Welch 2014].
A study funded by an organization that promotes
consumer access to ENDS as a means of harm re-
duction for nicotine-addicted individuals, empha-
sizes that estimated exposure levels associated with
the use of ENDS are generally much lower than
occupational exposure limits (OELs) for toxic in-
dustrial hazards [Burstyn 2014]. However, this sort
of comparison should be interpreted with caution
because OELs are typically set to reduce, rather
than totally prevent, adverse eects among exposed
workers. Furthermore, OELs are not set to protect
persons with particular vulnerabilities (e.g., asthma,
cardiac or circulatory conditions, pregnancy). Fi-
nally, health-protective OELs have not been estab-
lished for all chemicals capable of causing serious
health impact on exposed workers [NIOSH 2004;
CDC 2013c]. us, ndings that exposures are be-
low OELs should not lead directly to a conclusion
that such exposures are entirely safe. Moreover,
12 13
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
another assessment concluded that current expo-
sure guidelines for some components of ENDS
emissions may in fact be exceeded during ENDS
use, even for those exposed secondhand [Oerman
2014]. A recent white paper from the American In-
dustrial Hygiene Association thoroughly reviewed
the ENDS issue and cautioned that “… the existing
research does not appear to warrant the conclusion
that e-cigarettes are “safe” in absolute terms … e-
cigarettes should be considered a source of volatile
organic compounds (VOCs) and particulates in the
indoor environment that have not been thoroughly
characterized or evaluated for safety” [AIHA 2014].
Although much remains to be done, evaluation
of ENDS exposures and short-term health eects
has been a rapidly developing area of research. An
experimental chamber study in which air contami-
nants were measured documented degradation of
indoor air quality during ENDS use and found that
air measurements of polycyclic aromatic hydrocar-
bons classied as probable carcinogens by IARC
increased an average of 20% during ENDS use
[Schober et al. 2014]. In light of irritant compounds
(e.g., formaldehyde, acetaldehyde, and acrolein)
identied in emissions from ENDS, it has been rec-
ommended that research be done to evaluate possi-
ble adverse eects of exposure to these compounds
among ENDS users and individuals exposed to sec-
ondhand ENDS aerosol [Goniewicz et al. 2014]. In-
deed, ndings relating to short-term adverse eects
on ENDS users include preliminary reports of sig-
nicantly increased airways resistance [Gennimata
et al. 2012] and respiratory irritation and cough,
particularly among individuals with asthma [Tsi-
krika et al. 2014]. No studies to date have observed
similar short-term eects due to secondhand expo-
sure to ENDS aerosol, but one experimental study
demonstrated that passive exposure of human vol-
unteers to ENDS emissions did cause measurable
changes in serum levels of cotinine, a metabolite of
nicotine [Flouris et al. 2013].
It is plausible that personal use of ENDS and even sec-
ondhand exposure to ENDS aerosol will also lead to
adverse long-term health eects, but current data are
insucient to quantify the risks [Wagener et al. 2012;
BMA 2013; Kamerow 2013; AIHA 2014; Bhatnagar
et al. 2014; Drummond and Upson 2014; Schrauf-
nagel et al. 2014]. Evaluating potential long-term
health eects of ENDS use is an important research
priority [Andrade and Hastings 2013; AIHA 2014].
Traumatic Injuries and Fatalities
Caused by Tobacco Use
Tobacco use is also an important cause of traumatic
death, injury, and property damage. In 2011, there
were an estimated 90,000 res related to lighted
tobacco products in the United States, resulting in
an estimated 540 deaths and 1,640 injuries among
civilians, and more than $600 million in property
damage. Of these res, 1 in every 4 fatalities was a
victim who was not the smoker whose cigarette or
other combusting tobacco product caused the re
[Hall 2013]. Annual estimates have been declin-
ing over time, in part due to the decline in smok-
ing [Hall 2013]. In addition to injuries caused by
smoking-related res, use of tobacco products is a
recognized distracting factor while operating mo-
tor vehicles [NHTSA 2009], and smoking while
driving has been shown to increase the risk of be-
ing involved in a crash [Young et al. 2003]. Adverse
smoking-associated physiological alterations in
bone mineralization, blood vessels, and inam-
matory response [Leistikow 2000a] may also con-
tribute to higher risk of injuries, impaired recov-
ery, and higher rates of associated disability among
smokers [Lincoln et al. 2003].
Tobacco Use and Increased Risk of
Work-related Disease and Injury
In the general population, personal use of tobacco
and exposure to SHS both cause debilitating and fa-
tal health problems, as outlined above. What many
workers and their employers oen do not fully un-
derstand is that tobacco use can increase, some-
times profoundly, the likelihood and/or the sever-
ity of occupational disease and injury caused by
other hazards present in their workplaces. In addi-
tion, workplace exposure to SHS can cause serious
health eects among nonsmoking workers [NIOSH

14 15
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
1991]. is section outlines some ways that tobacco
use by workers and in the workplace can cause or
worsen occupational risks (see Box 3-4). Readers
are referred to other sources for more conceptual
detail about how tobacco use can aect doses of
hazardous industrial agents received by workers,
metabolism of these agents by exposed workers,
and pathogenesis and carcinogenesis of diseases
caused by these agents, as well as how researchers
assess complex causal relationships involving mul-
tiple causes [NIOSH 1979; DHEW 1979b; DHHS
1985; IARC 2004.
In some workplaces, an industrial toxicant released
from work processes is also present in tobacco
products and/or tobacco smoke. us, exposures
to these toxicants and the risks of disease associ-
ated with them can be increased for workers who
use tobacco or are exposed to SHS. ese chemicals
include acetone, acrolein, aldehydes (e.g., formal-
dehyde), arsenic, cadmium, carbon monoxide, hy-
drogen cyanide, hydrogen sulde, ketones, lead,
methyl nitrite, nicotine, nitrogen dioxide, phenol,
and polycyclic aromatic compounds [NIOSH 1979].
Heat generated by smoking tobacco in the work-
place can transform a workplace chemical to a
more toxic chemical [NIOSH 1979; DHEW 1979b;
DHHS 1985]. ough smokers are most highly ex-
posed to the transformed chemical, nonsmoking
coworkers in the same work area may also be ex-
posed. Examples of occupational agents that have
the potential for conversion to highly toxic chemi-
cals by smoking tobacco products include polytet-
rauoroethylene (Teon
®
) and other chlorinated
hydrocarbons (see Box 3-5).
Box 3-4. Some Ways Tobacco Use by Workers or in the Workplace Can Cause or
Worsen Occupational Safety and Health Risks
• Tobacco smoke/tobacco products can contain the same toxic agent that is released into the
workplace from a work process, thus increasing the dose of that agent received by tobacco-
using workers.
• A workplace chemical can be transformed into a more harmful agent by the heat involved
in smoking.
• Tobacco products can become contaminated with industrial toxicants found in the workplace,
thus facilitating entry of the agent into the body through inhalation, ingestion, and/or skin
absorption.
• Smoking can contribute to an eect on the body comparable to that which can result from
exposure to an industrial toxicant in the workplace, thus causing an additive combined eect.
• Smoking can act synergistically with industrial toxicants found in the workplace to cause a
much more profound eect than anticipated based on the known individual eects of smoking
and the occupational exposure.
• Tobacco use at work can contribute to work-related traumatic injuries and fatalities, either as an
ignition source for explosive or ammable agents in the workplace, or through tobacco-related
distraction while operating a vehicle or machinery at work.
• Smoking at work exposes nonsmoking coworkers to the hazards of secondhand smoke.
Adapted from NIOSH [1979, 1991]

14 15
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Tobacco products can readily become contaminat-
ed by industrial toxicants in the workplace through
contact of the tobacco products with unwashed
hands or contaminated surfaces and through de-
position of airborne contaminants onto the tobacco
products. Subsequent use of the contaminated to-
bacco product, at or even away from the workplace,
facilitates entry of these toxic agents into the user’s
body by inhalation, ingestion, and/or skin absorp-
tion [NIOSH 1979; DHEW 1979b]. To protect
workers from such exposure, occupational safety
and health regulations for lead, cadmium, and many
other specic toxic agents prohibit use of (and even
carrying of) tobacco products in designated work
areas (see Appendix Table A-2 and A-3).
Oen, a particular health eect can be indepen-
dently caused by tobacco use and workplace expo-
sure to a toxic agent. us, even if tobacco is used
only away from work, users will be more severely
aected than non-users, typically in an additive
manner. For example, tobacco smoking reduces a
worker’s lung function, leaving that worker more
vulnerable to the eect of any similar lowering of
lung function caused by occupational exposure
to dusts, gases, or fumes. Occupational exposures
that, like tobacco smoking, cause chronic airways
diseases and lung function impairment, include
cotton dust, coal mine dust, grain dust, silica dust,
welding fumes, and others [NIOSH 1979; DHEW
1979b; DHHS 1985].
For some occupational hazards, the combined im-
pact of tobacco use and exposure to the occupa-
tional agent can be synergistic (i.e., amounting to
an eect much greater than the sum of each inde-
pendent eect). Adverse biological eects of smok-
ing on the respiratory tract can lead to higher eec-
tive doses of an industrial toxicant among smoking
workers compared with nonsmoking workers. For
example, deposition of hazardous occupational
dusts can be increased in airways narrowed by
smoking, and clearance of deposited dust can be
slowed by smoking-induced impairment of both
alveolar and mucociliary transport [DHHS 1985].
In addition, inammatory cells recruited to the
alveoli and airways by smoking can enhance lung
injury from hazardous occupational agents, and
tumor promoters in tobacco smoke can act on cells
initiated by an occupational carcinogen, leading
to an increased likelihood that cancer will develop
from the occupational exposure among smokers
[DHHS 1985; IARC 2004].
An example of a synergistic eect is the combined
eect of smoking and asbestos exposure on lung
cancer (see Box 3-1). Smoking and asbestos expo-
sure both independently cause lung cancer. Work-
ers who both smoke and are exposed to asbestos at
work face a much greater risk of dying from lung
cancer than would be expected from the known in-
dependent risks of smoking by itself and asbestos
exposure by itself [NIOSH 1979; DHEW 1979b;
Box 3-5. Polymer Fume Fever in Smokers with Occupational Exposure to Tetrauoroethylene
Soon aer use of a new spray product containing tetrauoroethylene (a uorocarbon monomer) was
introduced at a small industrial facility, workers began experiencing severe episodic “u-like” symptoms. e
symptoms—lower backache accompanied by fever, chills, and malaise, and a dry, nonproductive cough—
occurred only on work days and usually subsided by the next morning. e spray was used in a stamp-making
process, and only the employees making the stamps were aected. All the aected workers ate and smoked
in their work area. Aer smoking was prohibited, no further symptoms occurred. Investigators concluded
that workers had experienced polymer-fume fever due to contamination of cigarettes with the uorocarbon
(via the workplace air or direct contact with workers’ hands) and subsequent inhalation of decomposition
products created by the intense heat of the cigarettes as they smoked [CDC 1987].

16 17
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
IARC 2004; Frost et al. 2011; Markowitz et al. 2013].
Workers who only smoke outside of work remain
vulnerable to the synergistic combined eect of
smoking and asbestos exposure. Other sorts of syn-
ergistic eects may involve consideration of tempo-
rality of exposures and outcome. Workers who start
smoking before they are occupationally exposed to
radon may face a more-than-multiplicative risk of
lung cancer that is much higher than the additive
risk faced by radon-exposed workers who did not
smoke until aer their occupational exposure to ra-
don [omas et al. 1994; IARC 2004]. With regard
to temporality of outcome, radiation-induced lung
cancer among radon exposed workers may occur
earlier (i.e., with shorted latency) in workers who
smoke than in nonsmoking workers [DHHS 1985].
When combined with certain occupational haz-
ards, tobacco use can also enhance the risk of
occupational traumatic injuries, fatalities, and
property loss. First, smoking in the workplace
can ignite explosive and other ammable materi-
als. Smoking has been implicated as the known or
suspected cause of several major industrial disas-
ters in the United States, including the infamous
Triangle Shirtwaist Factory re in 1911 [Leistikow
et al. 2000b]. To help prevent occupational explo-
sions and res, the Occupational Safety and Health
Administration (OSHA) and the Mine Safety and
Health Administration (MSHA) have established a
number of regulations prohibiting use and posses-
sion of smoking-related materials (e.g., cigarettes,
cigars, pipes, lighters, matches) in designated haz-
ardous work areas (see Appendix Table A-3). De-
spite existing regulations and widespread aware-
ness of the risk, occupational injuries and fatalities
caused by smoking have continued to occur in the
United States. ough prohibited in underground
coal mines, smoking materials ignited three fa-
tal coal mine explosions between 1990 and 2000
[MSHA 2000]. OSHA records for 2000 through
2012 include documentation of 13 work-related
res or explosions—ve of them fatal and all of
them involving employee injuries—where smok-
ing materials were implicated as the ignition source
[OSHA 2013a] (see Box 3-6).
Tobacco use on the job can also cause occupational
traumatic injuries and property loss unrelated to
res or explosions. Worker distraction by tobacco
use (e.g., opening, preparing, lighting, extinguish-
ing, or disposing of a tobacco product) or by a
tobacco-caused coughing spell can result in trau-
matic injury or death when that worker is driving a
work vehicle or operating other potentially hazard-
ous machinery or equipment [NIOSH 1979]. Sev-
eral studies have shown that smokers are more like-
ly to be injured at work than nonsmokers [Ryan et
al. 1992; Sacks and Nelson 1994; Craig et al. 2006].
As evident from the above discussion, both the
type of tobacco/tobacco-related product used and
where it is used can inuence whether and how
occupational safety and health risks are enhanced
Box 3-6. Smoking-ignited Fire Engulfs a Painting Crew—Two Dead and 11 Others Hospitalized
On July 29, 2003, two painting crews were working in a new residential subdivision when one of
their two box trucks broke down near the end of the day. e company had the driver of the other
truck pick up the stranded crew. at put 13 employees in the back of the truck and four in the cab.
e truck was loaded with paints, lacquer thinner, stains, and acrylics, among other paint chemicals.
A can of lacquer thinner spilled while employees were smoking in the truck. A lighted cigarette or a
spark from a lighter ignited the lacquer thinner vapors. e truck was engulfed immediately. All 13
employees in the back of the truck were hospitalized for severe burns, and two of them died as a result
of their injuries [OSHA 2013b].
16 17
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
by tobacco use for users and for non-users. For
example, tobacco smoking in a workplace will
put nonsmoking workers in that workplace at in-
creased risk due to their workplace exposure to
SHS. In contrast, in workplaces free of other oc-
cupational chemical or physical hazards, use of
smokeless tobacco would not be expected to re-
sult in any increased occupational risk for users
or their coworkers. ENDS use in the workplace
could, like use of any tobacco product, plausibly
enhance a user’s exposure to hazardous workplace
toxicants present in the workplace, may serve as a
potential ignition source in workplaces where ex-
plosive atmospheres are present, and can result in
secondhand exposure of coworkers (see Electronic
Nicotine Delivery Systems, above).
is page intentionally le blank.

19
NIOSH CIB 67
•
Workplace Tobacco Policies
4 Preventive Interventions
A range of eorts has been undertaken to decrease
tobacco use in the workplace and by workers. Most
of these interventions focus on smoking, which is
the most prevalent form of tobacco use (see Part
I, above). Policies related to tobacco use in work-
places originally focused on prohibiting smoking
in industrial work areas where explosion hazards
were present. Currently, workplace tobacco policies
increasingly center on the following:
• Smoke-free or tobacco-free indoors or campus-
wide prohibitions.
• Other restrictions on tobacco use by employees.
• Tobacco vending machines removal and pro-
hibiting other onsite sales of tobacco in work-
places.
• Provision of tobacco cessation programs.
• Employer-provided health insurance benets
designed to increase access and remove bar-
riers to evidence-based cessation treatments
and to provide incentives to quit tobacco use.
• Design of hiring policies based on smoking
status.
Many preventive policies relating to smoking and
the workplace are governed by local, state, or fed-
eral government laws and/or regulations. Others
are independently implemented by employers as
workplace requirements or conditions of employ-
ment. Employees and/or labor organizations can
share in a sense of joint ownership if they meaning-
fully collaborate with the employer on policy lan-
guage, approaches and timing, cessation supports,
and compliance and consequence issues. Involving
employees in the development, implementation,
and evaluation of workplace programs is an eec-
tive strategy for changing employee culture and be-
havior [NIOSH 2008b].
Workplace tobacco policies are underpinned by
several motivating interests (Boxes 4-1 and 4-2).
First and foremost is an interest in protecting to-
bacco users’ health, given that tobacco use causes
Box 4-1. Some Reasons for Employers to Implement Workplace Tobacco Interventions
• Reducing occupational disease and injuries (and workers’ compensation insurance costs).
• Lowering health insurance and life insurance costs and claims.
• Decreasing costs of training workers to replace those who become disabled or die prematurely.
• Increasing productivity through reduced absenteeism and reduced presenteeism.
• Reducing accidents and res (and related insurance costs).
• Lessening property damage (and related insurance costs).
• Eliminating indoor air pollution (and related cleaning, maintenance, and ventilation costs).
• Limiting liability and legal costs for failing to provide a safe and healthful working
environment.
• Enhancing worker morale and corporate image by showing concern for employees/customers.
Adapted from DHHS [1996]

20 21
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Box 4-2. Some Reasons for Employees to Quit Tobacco Use
To improve one’s own health
• Reduce risk for lung, mouth, throat, and other types of cancer. For example, lung cancer risk
drops by as much as 50% 10 years aer quitting, and risks for cancers of the mouth and throat
and bladder drop by 50% 5 years aer quitting.
• Diminish risk for coronary heart disease, stroke, and peripheral vascular disease. For example,
heart disease risk drops by as much as 50% 1 year aer quitting. Stroke risk attributable to to-
bacco use may be eliminated 5 years aer quitting.
• Ease symptoms such as coughing, wheezing, and shortness of breath within months of quitting
and long-term risk for chronic obstructive pulmonary disease (COPD) and other respiratory
diseases.
• Reduce risk of ulcer.
• Reduce risks of infertility (for women who stop smoking during their reproductive years).
To protect the health of others
• Avoid exposing family, friends, coworkers, and others to the harmful eects of secondhand
smoke (SHS).
• Lessen the risk of having a low-birth-weight baby (for women who stop smoking before becom-
ing pregnant or during the rst trimester of pregnancy).
• Increase the likelihood that one’s young children will not use tobacco when they reach adoles-
cence and adulthood.
To improve personal/family nances
• Save money by not spending money on tobacco and other tobacco-related expenditures (e.g.,
higher insurance premiums).
• Reduce the risk of nancial devastation resulting from income loss due to smoking-related dis-
ability or premature death, or from property loss due to a smoking-related home re.
To avoid personal inconvenience
• Avoid the need to go outside, sometimes in the rain and cold, when working in a tobacco-free
workplace.
the top fıve health conditions that impact the U.S.
population [Task Force on Community Preven-
tive Services 2010]. Protecting the health of non-
smoking workers is another important motivating
interest. Although the health and safety conse-
quences of tobacco use oer sucient rationale
for workplace tobacco policies, legal and econom-
ic considerations are also important. Government
(i.e., taxpayers), employers, and employees all
bear nancial costs associated with adverse eects
of tobacco use by workers and occupational expo-
sure to SHS.
20 21
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Legally determined employer responsibility to pro-
vide employees with a safe workplace can motivate
action by employers. OSHA does not currently ap-
ply the “general duty clause” [29 USC § 654; Section
5(a)1] of the Occupational Safety and Health Act of
1970 (OSH Act), Public Law 91-596, to SHS expo-
sure, but this is “a matter of prosecutorial discre-
tion” [OSHA 2003]. erefore, employers would do
well not to ignore other legal implications of their
duty to provide safe workplaces, including work-
places that are free from SHS exposure [Zellers et
al. 2007]. Employees may bring claims under state
workers’ compensation laws for illness or injury
attributable to SHS smoke exposure in the work-
place, under federal or state disability law for failing
to provide reasonable accommodations to allevi-
ate an employee’s exposure to SHS, and under the
common law for failure to provide employees with
a reasonably safe work environment free of SHS
[Zellers et al 2007]. Adopting an eective smoke-
free (or tobacco-free) workplace policy would pro-
tect an employer from such liability and provide
employees with a safe workplace.
With respect to personal costs paid by individual
smokers, there are obvious direct costs associated
with consumer purchases of tobacco products and
related materials. However, many smokers, espe-
cially those with the least discretionary income, are
unaware of longer-term nancial costs. One nan-
cial writer estimated in 2007 that a typical pack-a-
day smoker who is spending nearly $2,000 annu-
ally just to purchase cigarettes could instead amass
more than $1 million by investing that amount
each year from ages 18 to 65 in an individual retire-
ment account invested with an emphasis on growth
[Karp 2007]. at estimate did not encompass costs
of smoking other than the purchase price of tobac-
co. Smokers may be charged higher premiums for
health and life insurance and generally pay more
out-of-pocket costs for health care. Families can
experience substantial loss of income when their
smoking breadwinner becomes disabled or dies
prematurely from a smoking-related disease. Fi-
nancial devastation can also result from smoking-
caused residential res through costly personal
injury to the smoker and/or family members and
through loss of residence and other personal prop-
erty. In addition, smokers and their families may
incur additional costs for more frequent cleaning,
repairing, or replacement of clothing and other
personal furnishings to remove smoke odors and
tobacco-related stains.
With respect to employers’ costs, a recent study esti-
mated excess annual cost to U.S.-based private em-
ployers associated with employees who smoke ciga-
rettes compared with those who do not. Considering
aggregate cost and productivity impacts associated
with smoking breaks, absenteeism, presenteeism,
healthcare expenses, and pension benets, the study
estimated that the annual cost to employ a smoker
was, on average, $5,816 greater than the cost to em-
ploy a nonsmoker [Berman et al. 2013]. Interven-
tions that help smoking workers quit can benet a
business’ bottom line [NBGH 2013].
Workplace Policies Prohibiting
or Restricting Smoking
For safety reasons, smoking has long been pro-
hibited in particular work settings where explo-
sive or extremely ammable materials are present
(see Appendix Tables A-2 and A-3). A century ago,
such prohibitions may have been motivated more
out of concern about property loss than concern
for the well-being of workers. Subsequently, con-
cern about worker health has motivated additional
policies prohibiting the use of tobacco products in
specic work sites where exposure to certain haz-
ardous occupational agents can be increased as a
result of tobacco use (see Appendix Tables A-1 and
A-3). e need for such venue-specic prohibitions
on tobacco use has been widely understood and
accepted; however, compliance with these prohibi-
tions has been imperfect [MSHA 2000], indicating
a need for ongoing training and vigilance.
In the last decades of the past century, as the pub-
lic became more aware of the hazards of exposure
to SHS, government (at the local, state, and federal
22 23
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
levels) acted with the intent to reduce workplace
exposures to SHS and subsequently to eliminate
SHS from workplaces [DHHS 2006]. e Sur-
geon General has concluded that there is no risk-
free level of exposure to SHS [DHHS 2006, 2010b,
2014]. Complete prohibitions on workplace smok-
ing have been shown to be eective in essentially
eliminating SHS in workplaces [Hammond 1999].
Other measures, such as separating smokers from
nonsmokers, cleaning the workplace air, and ven-
tilating buildings, cannot eliminate exposures of
nonsmokers to SHS [NIOSH 1991; DHHS 2006,
2014; ASHRAE 2013]. us, ventilation is not an
acceptable alternative to making workplaces com-
pletely tobacco smoke-free.
Federal actions have been implemented to elimi-
nate SHS from some workplaces. Actively sup-
ported by ight attendants and their union as a way
to protect their health by eliminating SHS in their
workplace, federal law has progressively prohibited
smoking during commercial passenger ights, be-
ginning in 1988 with shorter domestic ights and
by 2000 encompassing all ights originating and/or
terminating in the United States [Pan et al. 2005].
In 1990, the Interstate Commerce Commission act-
ed to ban smoking on interstate buses [49 CFR Part
374.201]. A 1997 Presidential Executive Order has
prohibited
tobacco smoking in all interior space
owned, rented, or leased by the executive branch
of the federal government, with limited excep-
tions (e.g.,
specially equipped designated smoking
areas, certain residential settings, and space occu-
pied by non-federal parties)[Cook and Bero 2009].
In 2009, this policy to prohibit smoking in all inte-
rior space owned, rented, or leased by the executive
branch of the federal government was extended
by action of the General Services Administration,
eliminating remaining indoor designated smoking
areas and additionally prohibiting smoking within
25 feet of doorways and air intakes and in court-
yards where those outdoor spaces are under GSA
jurisdiction [73 Fed. Reg. 77517]. OSHA proposed
a rule that would have more universally restricted
smoking in the workplace [OSHA 1994], but later
withdrew the proposed rule, noting that workplace
regulation of SHS was being advanced by private
employers and by state and local governments
[OSHA 2001].
e rst comprehensive local and state laws restrict-
ing smoking in private workplaces, restaurants, and
bars went into eect in 1993 (Shasta County, Cali-
fornia) and 2002 (Delaware), respectively [CDC
2011b, 2012]. By the end of 2010, CDC reported
that 26 states, the District of Columbia, and a ma-
jority of the 50 largest U.S. cities had enacted com-
prehensive smoke-free laws prohibiting, with no
exceptions, smoking in all indoor areas of private
workplaces, restaurants, and bars [CDC 2011b,
2012]. Additionally, there has been a decline from
12/31/04 to 12/31/09 in the number of states with
laws preempting the regulation by local authorities
of smoking in government workplaces (from 16 to
9 states), private workplaces (from 15 to 9 states),
and restaurants (from 18 to 12 states) [CDC 2010].
ere is no fundamental legal impediment to adop-
tion of smoke-free workplace policies by private
employers [Gra 2008], and the private sector has
taken independent actions to eliminate exposure
to SHS in the workplace. In the early 1990s, new
standards established by the Joint Commission on
Accreditation of Hospitals spurred industry-wide
adoption of workplace smoke-free policies by ac-
credited hospitals, achieving a high level of com-
pliance within just 2 years [Longo et al. 1995]. In
addition to its intended eect on exposure to SHS,
this policy has been associated with additional ben-
ecial impacts on workplace safety and property
loss (see Box 4-3). Many other businesses also vol-
untarily implemented smoke-free policies in their
workplaces and, by the late 1990s, nearly 70% of
U.S. workers employed in non-residential indoor
worksites were working in smoke-free workplaces
[Shopland et al. 2004].
A number of studies, including meta-analyses,
have shown that smoke-free workplace policies de-
crease exposure of nonsmoking employees to SHS
at work and increase cessation among employees
who smoke [DHHS 2006; IARC 2009; Hopkins et al.
2010]. Although one review of the literature found

22 23
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
inconclusive evidence that smoke-free workplace
policies cause smokers to quit altogether [Call-
inan et al. 2010], there is strong evidence that such
policies are associated with increased quit rates
among smoking workers and with a reduction in
the amount of smoking among those workers who
continue to smoke [Fichtenberg and Glantz 2002;
Bauer et al. 2005; DHHS 2006; IARC 2009; Hop-
kins et al. 2010]. In contrast, less restrictive work-
place smoking policies are associated with sus-
tained tobacco use among workers [DHHS 2006;
IARC 2009]. A nationally representative survey
found that in workplaces without a workplace rule
limiting smoking, workers were signicantly more
likely to be smokers [Ham et al. 2011].
ere is clear evidence of improved health among
workers as a result of policy interventions to make
indoor spaces, including workplaces, smoke-free
[Callinan et al. 2010]. is is especially true for
workers in the hospitality industry (see Box 4-4).
Smoke-free policies have been shown to improve
indoor air quality, reduce SHS exposure, reduce
sensory and respiratory symptoms, and improve
lung function among bar workers [DHHS 2006;
IARC 2009; DHHS 2014]. Implementation of
smoke-free policies also has been shown in eco-
logical studies to be associated with reduced hospi-
talizations for heart attacks in the general popula-
tion [IARC 2009; IOM 2010; Tan and Glantz 2012;
DHHS 2014]. Results of similar studies suggest that
such policies may also reduce hospitalizations and
emergency department visits for asthma [Hahn
2010; Mackay et al. 2010; Tan and Glantz 2012;
Herman and Walsh 2011]. Smoke-free policies in
Box 4-3. Smoke-free Policies and Reduction in Structural Fires in Health-Care Facilities
Coinciding with comprehensive smoke-free workplace policies being enacted across the U.S. health
care industry, the number of smoking-ignited structure res involving health-care facilities dropped
from well over 3,000 per year in the early 1980s to only about 100 per year since the late 1990s. No-
tably, the percentage of all structural res in health-care facilities determined to have been caused by
smoking materials dropped from 30% to 5% over the same period [Arhens 2010].
Box 4-4. Prohibiting Smoking in Bars Improves the Health of Bartenders
A state law that prohibited smoking in most California taverns and bars began on January 1, 1998.
Bartenders were surveyed in the month before the law took eect and again about 1 month aer-
ward. Self-reported exposure to SHS at work fell from a median of 28 hours per week before the law
took eect to 2 hours per week aerward. Respiratory symptoms and eye, nose, and throat irritant
symptoms were each reported by about 75% of bartenders before the law took eect. Of those with
symptoms at baseline, 59% with respiratory symptoms and 78% with irritant symptoms experienced
resolution of those symptoms aer the law took eect (P<0.001). On average, lung function mea-
surements also improved. e authors of this study concluded that making taverns and bars smoke-
free resulted in a rapid improvement in the health of bartenders [Eisner et al. 1998].
24 25
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
the hospitality industry have been found to receive
high levels of public support and compliance, and
they have not had a negative economic impact on
the hospitality industry [DHHS 2006; IARC 2009].
Acting on strong evidence of the eectiveness of
smoke-free policies available by 2001, the Task
Force on Community Preventive Services recom-
mended workplace smoking bans and restrictions
as eective means for reducing exposure to SHS
[Hopkins et al. 2010]. More recent evidence has
led the Task Force to now recommend smoke-free
workplace policies (i.e., total prohibition of smok-
ing in the workplace), not only as a means to reduce
exposure to SHS, but also as an eective means to
increase tobacco cessation, reduce tobacco use
prevalence, and reduce tobacco-related morbid-
ity and mortality [Hopkins et al. 2010; Task Force
on Community Preventive Services 2010; GCPS
2012a]. To prevent SHS exposures, the recent Sur-
geon General’s report urges that comprehensive
smoke-free indoor protections be extended to the
entire U.S. population [DHHS 2014].
World Health Organization reports have recom-
mended that, in the absence of evidence that can
assure authorities that use of ENDS does not ex-
pose bystanders to toxic emissions, ENDS should
not be exempted from laws that restrict the places
in which cigarette smoking is allowed [WHO 2009,
2014]. e British Medical Association has taken
the position that use of e-cigarettes should be pro-
hibited in workplaces and public places, not only
to limit potentially harmful eects of secondhand
exposures, but also to ensure that their use does
not undermine smoking prevention and cessation
eorts [BMA 2013]. Similarly concerned about
potentially hazardous secondhand exposure, the
Federal German Institute for Risk Assessment has
likewise recommended prohibiting use of ENDS
wherever tobacco smoking is prohibited [FGIRA
2012], and the American Heart Association has
recommended including e-cigarettes in smoke-
free laws [Bhatnagar et al. 2014]. e Forum of
International Respiratory Societies has recom-
mended that ENDS use be prohibited “in public
places, workplaces, and on public transportation”
[Schraufnagel et al. 2014]. e American Indus-
trial Hygiene Association similarly reviewed the
issue of ENDS and concluded that “their use in the
indoor environment should be restricted, consis-
tent with current smoking bans, until and unless
research documents that they will not signicantly
increase the risk of adverse health eects” to those
exposed secondhand [AIHA 2014]. In the United
States, the number of states and localities that ex-
plicitly prohibit use of e-cigarettes in public places
where tobacco smoking is already prohibited is in-
creasing with time [ANRF 2014], totaling 3 states
and more than 200 localities before the end of 2014
[CDC 2014c].
Employers are taking notice, and some are acting to
prohibit ENDS use in their workplaces [Slavit 2011;
Gay 2013; Moore 2014]. Given the current unregu-
lated nature of ENDS and the liquid concoctions
used them, along with uncertainty about the im-
pact of ENDS use in the workplace on the health of
non-users, the simplest approach is for employers
to simply add ENDS to the list of products covered
by their tobacco-free (or smoke-free) workplace
policy [Phillips 2014].
Employer Prohibitions on
Tobacco Use Extending Beyond
the Workplace
Some employers have taken action to extend re-
strictions on tobacco use by their employees be-
yond the workplace. For example, in 2013, the U.S.
Public Health Service Commissioned Corps be-
came the rst federal uniformed service to prohibit
tobacco use by its ocers whenever and wherever
they are in uniform [ACPM 2013]. More contro-
versial are attempts of private employers to con-
trol the behavior of their employees outside of the
workplace. For example, at a major medical center
that had a smoke-free campus policy in place for
years, the employer recently announced plans to
prohibit smoking by workers during their workday
breaks, including lunchtime, even when o campus
[Toland 2013]. Several large employers and orga-
nizations (including the Cleveland Clinic, Union
24 25
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Pacic Railroad, the World Health Organization,
and several others) have gone further by barring
the hiring of smokers [Asch et al. 2013; Schmidt et
al. 2013].
Controversy surrounds many organizational poli-
cies that bar the hiring of smokers or prohibit to-
bacco use by employees during the workday when
they are away from the worksite even on their own
time. Proponents argue that a nonsmoking work-
force serves as a positive role model for health, ex-
periences better health status, incurs substantially
lower health-care costs for employers and employ-
ees alike, and improves productivity [Asch et al.
2013]. Opponents posit the addictive nature of to-
bacco and the fact that tobacco use usually begins
in adolescence, note that tobacco use remains legal,
and cite the disparate and potentially discrimina-
tory eects such a policy might have on minority,
lower-income, or less educated workers and job
candidates—groups that tend to have higher levels
of tobacco use. ey also point out that employers
who refuse to hire smokers typically do not simi-
larly refuse to hire individuals with other personal
health behaviors that, like tobacco use, have adverse
health consequences. ey add that more than half
of states have laws in place prohibiting employ-
ers from refusing to hire individuals because they
smoke [Schmidt et al. 2013].
Workplace Tobacco Use
Cessation Programs
Smoking employees who want to quit can benet
from employer-provided resources and assistance.
In 2010, roughly 65% of employed smokers in the
United States expressed an interest in quitting to-
bacco and about half reported having tried to quit
in the previous year [Yong et al. 2014]. Just as poli-
cies increasing tobacco taxes at the state and federal
levels have led to increased calls to state telephone
tobacco cessation quitlines [McGoldrick and
Boonn 2010], implementing tobacco-free work-
place policies can be expected to increase worker
interest in quitting and cessation support services.
When a smoking cessation program is established
in a workplace, smokers employed at that work-
place are more likely to intend to quit in the next 6
months [Ham et al. 2011]. Various levels and types
of cessation support can be provided [DHHS 1996].
On a basic level, a health-care provider’s inquiry
about tobacco use and delivery of brief counseling
advice to tobacco users has been shown to increase
quit rates, with more intensive intervention having
a greater eect [O’Hara et al. 1993; Clinical Practice
Guideline 2008]. is basic approach can be read-
ily ‘piggy-backed’ on occupational health services
that already exist in many workplaces. For example,
all workers enrolled in OSHA-mandated respira-
tory protection programs must be asked about to-
bacco use as part of their medical evaluation (see
Appendix Table A-2 for applicable OSHA standard
numbers). Other existing opportunities to ascertain
individual smoking behavior include post-employ-
ment (pre-placement) examinations, tness-for-
duty evaluations, and other health examinations
already provided by employers. Whenever workers
who smoke are identied, they can be counseled
and oered cessation assistance.
Occupational health providers and workplace
health promotion sta can oer basic cessation
assistance by encouraging workers to use tobacco
cessation telephone quitlines, web-based cessation
services, and cessation text-messaging programs,
such as those oered by the National Cancer In-
stitute through http://smokefree.gov/smokefreetxt.
State quitlines exist in all 50 states and the District of
Columbia, are publicly funded, are typically avail-
able at no cost to smokers, and oen provide free or
discounted FDA-approved cessation medications.
Callers can access their state quitline by dialing
1-800-QUIT-NOW (1-800-784-8669). Similarly,
Spanish-speaking callers can access Spanish-lan-
guage services from their state quitline by calling
1-855-DEJELO-YA (1-855-335-3569). Because of
strong evidence that quitlines increase quit rates,
the 2008 Public Health Service Clinical Practice
Guideline and the Community Preventive Services
Task Force recommend quitline interventions, es-
pecially proactive quitlines where the counselor
initiates follow-up calls [GCPS 2012b; Clinical
26 27
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Practice Guideline 2008]. e Public Health Ser-
vice Guideline further concludes that quitlines are
eective with diverse populations and have broad
reach [Clinical Practice Guideline 2008]. Similarly,
the Community Preventive Services Task Force
found that quitlines—especially proactive quitlines
where the counselor initiates follow-up calls—in-
crease tobacco cessation among callers who are in-
terested in quitting and can help expand the use of
evidence-based cessation services among smokers
in populations that have limited access to cessation
treatment [GCPS 2012b]. An updated Cochrane
review has rearmed the eectiveness of proac-
tive quitlines [Stead et al. 2013]. eir widespread
availability, ease of accessibility, aordability, and
potential reach to populations with higher levels
of tobacco use make quitlines an important com-
ponent of any cessation eort [Clinical Practice
Guideline 2008]. Yet many employers do not make
their employees aware of them. For example, a 2008
Washington State survey of almost 700 employers
with at least 50 employees found that only 6% men-
tioned the availability of the state quitline in their
health promotion messages to workers [Hughes et
al. 2011].
e most comprehensive workplace cessation pro-
grams go well beyond minimal cessation counsel-
ing and referral to no-cost quitlines and web-based
programs. Employers can enter into preferred re-
lationships with state quitlines or contract quitline
providers to establish employer-specic quitlines
with special services [Lichtenstein et al. 2010]. Web-
based intervention to assist with tobacco cessation
is a less studied but promising approach [Clinical
Practice Guideline 2008; Civljak et al. 2013]. One
report described success achieved by a major cor-
poration with a program oering employees web-
based cessation intervention [Graham et al. 2007].
Individualized counseling and support can oen be
provided by an existing employee assistance pro-
gram. A systematic review of the literature found
that workplace-based smoking cessation services
such as individual and group counseling, pharma-
cological treatment, and social support are all eec-
tive in enhancing quit rates when compared with
no interventions or minimal interventions [Cahill
and Lancaster 2014]. Optimal work-based tobacco
cessation programs are designed to provide follow-
up assistance and to support multiple quit attempts,
because most smokers try to quit repeatedly before
nally succeeding [Clinical Practice Guideline 2008].
Ideally, employers should incorporate tobacco
cessation support programs into a more compre-
hensive approach that addresses the overall safety,
health, and well-being of workers. A growing evi-
dence base supports the enhanced eectiveness of
workplace programs that integrate health promo-
tion eorts such as smoking cessation with more
specic occupational health protection programs
[Hymel et al. 2011; NIOSH 2013b]. Such inte-
grated workplace tobacco cessation programs may
be most usefully implemented among blue-collar
workers, who generally have higher smoking (and
lower quitting) rates than oce workers and who
generally face higher risks from industrial hazards.
A large randomized study involving 15 manufac-
turing sites showed that combining occupational
health and safety messages with health promotion
messages resulted in a doubling of smoking quit
rates among hourly workers (from 5.9% to 11.8%;
P =0.04) compared with health promotion mes-
sages alone [Sorensen et al. 2003]. Another dem-
onstration study of an integrated program aimed
at enhancing smoking cessation among blue collar
workers targeted participants in a union appren-
ticeship program [Barbeau et al. 2006] (see Box 4-5).
Health Insurance and
Smoking Behavior
Another recent phenomenon is the increasing use
of health insurance to encourage employees to
adopt positive personal health-related behaviors
(e.g., smoking cessation) through modication
in the design of benets and out-of-pocket cost
for covered individuals. For example, it is known
that quit rates are higher when health insurance
covers the costs of evidence-based smoking cessa-
tion treatments [Clinical Practice Guideline 2008].

26 27
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Ideally, such coverage should provide access to
all evidence-based cessation treatments, includ-
ing individual, group, telephone counseling, and
all seven FDA-approved cessation medications
[Clinical Practice Guideline 2008; CDC 2014c].
is coverage should have minimal barriers (such
as cost-sharing and prior authorization) or no
barriers [Clinical Practice Guideline 2008; CDC
2014b]. e coverage should also be promoted to
tobacco users and health-care providers to ensure
that they are aware of it and to that the covered
treatments are used [Clinical Practice Guideline
2008; CDC 2014b].
Many workers are covered by employer-provided
health insurance, and the employer can negotiate
with the insurance company to set benets, pre-
miums, and cost shares for covered workers. For
multi-employer health insurance programs that
cover millions of union workers, representatives of
the union also have a voice in the process. Insur-
ance companies and human resources managers
responsible for designing and negotiating health
insurance plans need to be aware of various laws
at the state and federal levels that limit what can
be negotiated. Applicable federal laws include the
Health Insurance Portability and Accountability
Act (HIPAA), Public Law 104-191, and the Patient
Protection and Aordable Care Act (ACA), Pub-
lic Law 111-148, which is now being implemented
[Madison et al. 2013].
e ACA includes provisions pertinent to tobacco
use and cessation [McAfee et al. 2015]. For the
many workers covered by group and individual
private health insurance plans, including both fully
insured and self-insured employer coverage, the
ACA requires non-grandfathered private plans to
cover—without cost sharing—all preventive ser-
vices judged by the U.S. Preventive Services Task
Force to provide a high certainty of substantial
(grade A) or a moderate-to-substantial (grade B)
net benet. is includes tobacco use counseling
and tobacco cessation interventions, to which the
Box 4-5. Demonstration of a Smoking Cessation Program for Blue-Collar Workers
Apprentice ironworkers at a local union in Boston were studied before and aer a 4-month
smoking cessation demonstration program. With input from union leaders and members, the
program was carried out in a local union hall, where posters promoting cessation and featur-
ing photographs of ironworkers were displayed. Articles explaining and promoting the program
were published in the union newsletter. Occupational health protection aspects of the program
were featured in an educational module on “toxics and tobacco.” is module was taught by an
industrial hygienist and covered separate and combined adverse health eects, including cancer,
caused by smoking and workplace hazards (e.g., asbestos, welding fumes, and diesel exhaust)
commonly encountered by ironworkers. Tobacco treatment specialists led weekly group sessions
on tobacco cessation. Incentives to participate in the sessions included free lunches and, for those
attending all sessions, a chance for a rae prize. Self-help quit kits were provided to apprentices
who chose not to attend the group sessions. Nicotine replacement therapy was available at no cost
to participants. Of 337 participants, 139 (41.2%) were current smokers at the time the program
started. One month aer the program concluded, 27 (19.4%) of those smokers had quit—a rate
much higher than the expected ~5% quit rate. Program participants were 3 times more likely to
quit than nonparticipants [Barbeau et al. 2006].
28 29
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Task Force assigned an “A” grade [Kofman et al.
2012]. Federal guidance clarifying this requirement
states that health plans will be considered to be in
compliance with this requirement if, for example,
they cover (1) screening for tobacco use; (2) at least
two quit attempts a year, with each quit attempt in-
cluding four sessions of individual, group, and tele-
phone counseling of at least ten minutes each and
all seven FDA-approved cessation medications for
a 90-day course [USDOL 2014 McAfee et al. 2015].
e guidance further states that none of these treat-
ments should be subject to cost-sharing or prior
authorization [USDOL 2014; McAfee et al. 2015].
If fully implemented by health insurers, this level
of coverage, which is closely based on the 2008 U.S.
Public Health Service Clinical Practice Guideline,
would be expected to increase smokers’ access to
proven cessation treatments and to help thousands
of smokers quit [McAfee et al. 2015].
Insurers and employers who sponsor health insur-
ance coverage for their employees will have ex-
panded opportunities to design incentives for well-
ness programs, including interventions intended
to enhance tobacco cessation (or, with some limi-
tations, disincentives for continued tobacco use).
For example, in order to motivate employees to
quit smoking, the ACA allows employer-sponsored
health insurance issuers to charge tobacco users
premiums that are up to 50% higher than premi-
ums charged non-tobacco users [Kofman et al.
2012; Madison et al. 2013]. However, issuers who
impose these surcharges in the small-group mar-
ket must provide tobacco users the opportunity to
avoid them, for example by participating in a cessa-
tion program [78 Fed. Reg. 33158]. States have au-
thority to limit the magnitude of such surcharges,
and a number of states have done so [CMS 2014].
Using Incentives and
Disincentives to Modify
Tobacco Use Behavior
Increasingly, governmental and employer actions
are removing barriers and oering incentives for
employee quit attempts and success in quitting to-
bacco use. Likewise, such actions are increasingly
discouraging tobacco use by workers covered by
employer-sponsored health insurance programs
(e.g., through increased premiums for smokers).
For example, more than one-third of surveyed large
employers who oer their employees smoking ces-
sation programs incentivize participation in these
programs. e number of large employers who
are planning to reward or penalize smokers based
on their smoking status is increasing—more than
half of companies plan to do so by the end of 2013,
up from less than 25% of employers who did so in
2010 [Towers Watson 2011].
A clear barrier that reduces use of evidence-based
cessation treatments is out-of-pocket costs for
cessation counseling and FDA-approved cessa-
tion medications. Because of strong evidence that
the number of tobacco users who quit can be in-
creased by reducing these out-of-pocket costs, the
Community Preventive Services Task Force recom-
mends reducing tobacco users’ out-of-pocket costs
for cessation treatments [GCPS 2012c].
e Task Force had earlier examined the issue of
providing incentives for tobacco cessation, nding
insucient evidence at that time that workplace-
based incentives or competitions by themselves re-
duced tobacco use among employees [GCPS 2005].
Even then, the Task Force went on to recommend
worksite-based incentives and competitions when
they are combined with other evidence-based in-
terventions (e.g., education, group support, tele-
phonic counseling, self-help materials, smoke-free
workplace policies) as part of a comprehensive ces-
sation program [GCPS 2005].
A subsequent systematic review of the literature
identied a single well-designed study in which
nancial incentives integrated into a smoking ces-
sation program produced a substantial and sus-
tained benecial impact [Cahill and Perera 2011].
Incentive payments for that randomized trial were
structured as $100 for completion of the smoking-
cessation program; $250 for abstinence (conrmed
biochemically) during the rst 6 months aer study
28 29
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
enrollment; and $400 for abstinence (also con-
rmed biochemically) during the subsequent 6
months. Smokers oered the nancial incentives
were three times as likely to enroll in the program
(15.4% vs. 5.4%, P<0.001), four times as likely to
complete the program (10.8% vs. 2.5%, P<0.001),
and three times as likely to remain abstinent more
than a year later (14.7% vs. 5.0%, P<0.001) [Volpp
et al. 2009]. Notably, this study did not involve
establishing a new smoking cessation program;
rather, all participants were informed about exist-
ing smoking-cessation resources available in their
community and about employer-provided health
benets related to smoking cessation.
A recent review explored ethical and legal issues
relating to employer-provided incentives intended
to change individual health behaviors, including
tobacco use [Madison et al. 2011]. e authors
identied a number of specic issues that call for
scrutiny, including the need to ensure that incen-
tive programs are designed to work as intended,
and the potential for incentives to be used in an
unduly coercive or discriminatory manner. ey
emphasized that employers should play a collab-
orative, supportive role in advancing the health of
workers, and they further suggested that, in order
to limit the potential for discrimination, programs
should be designed to minimize differences in
individual employees’ abilities to access incentives
[Madison et al. 2011]. It should be recognized that,
while imposing insurance premium surcharges or
other disincentives on smokers has the potential to
motivate them to quit smoking, the evidence that
they are eective in doing so is quite limited, and
care is needed to avoid such practices having un-
intended consequences. For example, these prac-
tices could lead smokers to conceal their smoking
(and thereby not benet from cessation assistance),
or even to forgo health insurance coverage or quit
their jobs [Madison et al. 2011; McAfee et al. 2015].
e appropriate intent of incentives is to improve
health and reduce health-care costs overall, and not
merely to shi health-care costs to high-risk indi-
viduals [Madison et al. 2011, 2013].
In summary, workplace policies are powerful tools
that can benet worker health. Well-designed poli-
cies protect workers from occupational risks, pro-
vide workplace-associated opportunities for en-
hancing worker health, and motivate workers to
take benecial actions to protect their well-being.
Although not a primary focus of this CIB, work-
place policies that eectively sustain or improve
worker health can also be cost-eective and benet
the employer’s bottom line.
is page intentionally le blank.
31
NIOSH CIB 67
•
Workplace Tobacco Policies
5 Conclusions
• Cigarette smoking by workers and SHS ex-
posure in the workplace have both declined
substantially over recent decades, but about
20% of all U.S. workers still smoke and about
20% of nonsmoking workers are still exposed
to SHS at work.
• Smoking prevalence among workers var-
ies widely by industry and occupation, ap-
proaching or exceeding 30% in construction,
mining, and accommodation and food ser-
vices workers.
• Prevalence of ENDS use by occupation and
industry has not been studied, but ENDS has
grown greatly, with about 1 in 3 current U.S.
adult smokers reporting ever having used e-
cigarettes by 2013.
• Smokeless tobacco is used by about 3% of
U.S. workers overall, but smokeless tobacco is
used by more than 10% workers in construc-
tion and extraction jobs and by nearly 20% of
workers in the mining industry, which can be
expected to result in disparities in tobacco-
related morbidity and mortality.
• Tobacco use causes debilitating and fatal dis-
eases, including cancer, respiratory diseases,
and cardiovascular diseases. ese diseases
aict mainly users, but they also occur in
those exposed to SHS. Smoking is substan-
tially more hazardous, but use of smokeless
tobacco also causes adverse health eects.
More than 16 million U.S. adults live with
a disease caused by smoking, and each year
nearly a half million die prematurely from
smoking or exposure to SHS.
• Tobacco use is associated with increased risk
of injury and property loss due to re, explo-
sion, and vehicular collisions.
• Tobacco use by workers can increase, some-
times profoundly, the likelihood and the
severity of occupational disease and injury
caused by other workplace hazards (e.g., lead,
asbestos, and ammable materials).
• Restrictions on smoking and tobacco use in spe-
cic work areas where particular high-risk oc-
cupational hazards are present (e.g., explosives,
highly ammable materials, or highly toxic ma-
terials that could be ingested via tobacco use)
have long been used to protect workers.
• A risk-free level of exposure to SHS has not
been established, and ventilation is insu-
cient to eliminate indoor exposure to SHS.
• e risk of adverse health eects associated
with using ENDS or secondhand exposure to
particulate aerosols and gases emitted from
ENDS remains to be fully characterized.
• Policies that prohibit tobacco smoking through-
out the workplace (i.e., smoke-free workplace
policies) are now widely implemented, but they
have not yet been universally adopted across the
United States. ese policies improve workplace
air quality, reduce SHS exposure and related
health eects among nonsmoking employees,
increase the likelihood that workers who smoke
will quit, decrease the amount of smoking dur-
ing the working day by employees who con-
tinue to smoke, and have an overall impact of
improving the health of workers (i.e., among
both nonsmokers who are no longer exposed
to SHS on the job and smokers who quit).
• Workplace-based eorts to help workers quit
tobacco use can be easily integrated into ex-
isting occupational health and wellness pro-
grams. Even minimal counseling and/or sim-
ple referral to state quitlines, mobile phone
texting interventions, and web-based inter-
vention can be eective, and more compre-
hensive programs are even more eective.
• Integrating both occupational safety and
health protection components into workplace
health promotion programs (e.g., smoking
32 33
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
cessation) can increase participation in to-
bacco cessation programs and successful ces-
sation among blue-collar workers.
• Smokers, on average, are substantially more
costly to employ than nonsmokers.
• Some employers have policies that prohibit
employees from using tobacco when away
from work or that bar the hiring of smokers
or tobacco users. However, the ethics of these
policies remain under debate, and they may
be legally prohibited in some jurisdictions.
32 33
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
6 Recommendations
e following recommendations relate specically
to the issues raised in this CIB. NIOSH recom-
mends that employers take the following actions
related to employee tobacco use:
• At a minimum, establish and maintain smoke-
free workplaces that protect those in workplac-
es from involuntary, secondhand exposures to
tobacco smoke and airborne emissions from
e-cigarettes and other electronic nicotine de-
livery systems. Ideally, smoke-free workplaces
should be established in concert with tobacco
cessation support programs. Smoke-free zones
should encompass (1) all indoor areas without
exceptions (i.e., no indoor smoking areas of
any kind, even if separately enclosed and/or
ventilated), (2) all areas immediately outside
building entrances and air intakes, and (3) all
work vehicles. Additionally, ashtrays should be
removed from these areas.
• Optimally, establish and maintain entirely to-
bacco-free workplaces, allowing no use of any
tobacco products across the entire workplace
campus (see model policy in Box 6-1).
• Comply with current OSHA and MSHA
regulations that prohibit or limit smoking,
smoking materials, and/or use of other to-
bacco products in work areas characterized
by the presence of explosive or highly am-
mable materials or potential exposure to
toxic materials (see Table A-3 in the Appen-
dix). To the extent feasible, follow all similar
NIOSH recommendations (see Table A-2 in
the Appendix).
• Provide information on tobacco-related health
risks and on benets of quitting to all employ-
ees and other workers at the worksite (e.g.,
contractors and volunteers).
ȣ Inform all workers about health risks of
tobacco use.
ȣ Inform all workers about health risks of
exposure to SHS.
ȣ Train workers who are exposed or
potentially exposed to occupational
hazards at work about increased health
and/or injury risks of combining tobacco
use with exposure to workplace hazards,
about what the employer is doing to limit
the risks, and about what the worker can
do to limit his/her risks.
• Provide information on employer-provided
and publicly available tobacco cessation ser-
vices to all employees and other workers at the
worksite (e.g., contractors and volunteers).
ȣ At a minimum, include information on
available quitlines, mobile phone texting
interventions, and web-based cessation
programs, self-help materials, and
employer-provided cessation programs
and tobacco-related health insurance
benets available to the worker.
ȣ Ask about personal tobacco use as part
of all occupational health and wellness
program interactions with individual
workers and promptly provide encourage-
ment to quit and guidance on tobacco
cessation to each worker identied as a
tobacco user and to any other worker who
requests tobacco cessation guidance.
• Oer and promote comprehensive tobacco
cessation support to all tobacco-using work-
ers and, where feasible, to their dependents.
ȣ Provide employer-sponsored cessa-
tion programs at no cost or subsidize
34 35
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
cessation programs for lower-wage
workers to enhance the likelihood of
their participation. If health insurance is
provided for employees, the health plan
should provide comprehensive cessation
coverage, including all evidence-based
cessation treatments, unimpeded by co-
pays and other nancial or administrative
barriers.
ȣ Include occupational health protection
content specic to the individual workplace
in employer-sponsored tobacco cessation
programs oered to workers with jobs
involving potential exposure to other
occupational hazards.
• Become familiar with available guidance (e.g.,
CDC’s “Implementing a Tobacco-Free Cam-
pus Initiative in Your Workplace”) (see Box
6-2) and federal guidance on tobacco cessa-
tion insurance coverage under the ACA (e.g.,
http://www.dol.gov/ebsa/faqs/faq-aca19.
html) before developing, implementing, or
modifying tobacco-related policies, interven-
tions, or controls.
• Develop, implement, and modify tobacco-
related policies, interventions, and controls
in a stepwise and participatory manner. Get
input from employees, labor representatives,
line management, occupational safety/health
and wellness sta, and human resources pro-
fessionals. ose providing input should in-
clude current and former tobacco users, as
well as those who have never used tobacco.
Seek voluntary input from employees with
health conditions, such as heart disease and
asthma, exacerbated by exposure to SHS.
• Make sure that any dierential employment
benets policies that are based on tobacco
use or participation in tobacco cessation pro-
grams are designed with a primary intent
to improve worker health and comply with
all applicable federal, state, and local laws
and regulations. Even when permissible by
law, these differential employment ben-
efit policies—as well as dierential hiring
policies based on tobacco use—should be
implemented only aer seriously considering
ethical concerns and possible unintended con-
sequences. ese consequences can include
the potential for adverse impacts on individ-
ual employees (e.g., coercion, discrimination,
and breach of privacy) and the workforce as
a whole. Furthermore, the impact of any dif-
ferential policies that are introduced should be
monitored to determine whether they improve
health and/or have unintended consequences.
NIOSH recommends that workers who smoke cig-
arettes or use other tobacco products take the fol-
lowing actions:
• Comply with all workplace tobacco policies.
• Ask about available employer-provided to-
bacco cessation programs and cessation-re-
lated health insurance benets.
• Quit using tobacco products. Know that quit-
ting tobacco use is benecial at any age, but
the earlier one quits, the greater the benets.
Many people nd various types of assistance
to be very helpful in quitting, and evidence-
based cessation treatments have been found
to increase smokers’ chances of quitting suc-
cessfully. Workers can get help from
ȣ tobacco cessation programs, including
web-based programs (e.g., http://smokefree.
gov and http://www.cdc.gov/tips) and
mobile phone texting services (e.g., the
SmokefreeTXT program http://smokefree.
gov/smokefreetxt);
ȣ state quitlines (phone: 1-800-QUIT-NOW
[1-800-784-8669], or 1-855-DEJELO-YA
[1-855-335-3569 for Spanish-speaking
callers]); and/or
ȣ health-care providers.
In addition, individual workers who want to quit
tobacco may nd several of the websites listed in
Box 6-2 helpful.
34 35
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
NIOSH recommends that all workers, including
workers who use tobacco and nonsmokers exposed
to SHS at their workplace:
• Know the occupational safety and health risks
associated with their work, including those
that can be made worse by personal tobacco
use, and how to limit those risks; and
• Consider sharing a copy of this CIB with their
employer.

36 37
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Box 6-1: A Model Policy for a Tobacco-Free Workplace
[COMPANY]’s TOBACCO-FREE POLICY
I. PURPOSE
[COMPANY] is dedicated to providing a healthy, comfortable, and productive work environ-
ment for all of our employees and clients. e goal of this policy is two-fold. First, this policy aims
to promote a safe work environment for everyone who works on or visits [COMPANY]’s campus.
Second, this policy is designed to improve the health of [COMPANY]’s employees by promoting
tobacco use cessation.
II. POLICY
Eective [DATE], [COMPANY] is implementing a campus-wide tobacco-free policy that ap-
plies to all employees, clients, and visitors. is policy prohibits the use of any tobacco products,
including but not limited to smokeless tobacco, cigarettes, cigars, and electronic smoking/vaping
devices. is policy is in eect at all times, including during and aer regular business hours.
Smoking or use of tobacco products will not be permitted in any indoor or outdoor space owned,
leased, or used by the company or within 25 feet of any door, window, or ventilation system. Ad-
ditionally, tobacco use will not be permitted in company-owned parking lots or vehicles. is
policy also applies to any work function where two or more employees are present, regardless of
where the event is held.
Employees who choose to use tobacco products may do so during their regularly scheduled
breaks o company property. Ashtrays will not be provided or permitted in any company area.
Smoking areas may be designated at the discretion of management. Any designated smoking ar-
eas must be accompanied by proper signage, and they must be located at least 25 feet away from
any door, window, or ventilation system.
is policy also prohibits the sale on company property of any tobacco products, including but
not limited to cigarettes, cigars, pipe tobacco, smokeless tobacco, and electronic smoking/vaping
devices and materials.
III. PROCEDURE
Copies of this policy shall be distributed to all current employees in advance of the implementa-
tion date. All future employees will be provided a copy of this policy during the hiring process
and a copy will be available for review from [COMPANY]’s human resources department at any
time. Signs stating that this is a “Tobacco-Free Campus” will be posted.
Compliance with this policy is mandatory and violations will be subject to disciplinary action in
accordance with other relevant company policy. Repeated violations may result in more serious
disciplinary action, to be handled by supervisors in conjunction with the human resources de-
partment. [COMPANY] will not retaliate, discourage, or prohibit any employee, client or visitor
from reporting violations of this policy.
36 37
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Box 6-1: A Model Policy for a Tobacco-Free Workplace (Continued)
IV. TOBACCO CESSATION OPPORTUNITIES
[COMPANY] encourages all employees who currently use tobacco products to quit by taking
advantage of cessation programs available through the company. More information about these
oerings can be obtained by contacting [APPROPRIATE WORKPLACE CONTACT] or human
resources.
V. QUESTIONS
Any questions regarding this policy should be directed to [NAME OF APPROPRIATE WORK-
PLACE CONTACT] at [NUMBER].
ank you for your cooperation.
Adapted from CDC [2005], ANR [2014], and the University of Maryland Francis King Carey
School of Law Legal Resource Center [2014].
Box 6-2. Selected Web Resources
Government
U.S. Department of Health And Human Services
• Smokefree.gov
http://www.Smokefree.gov
• BeTobaccoFree.gov
http://betobaccofree.hhs.gov/index.html
• The Guide to Community Preventive Services: Reducing Tobacco Use and Second-
hand Smoke Exposure
http://www.thecommunityguide.org/tobacco/index.html
CDC
• Oce on Smoking and Health
http://www.cdc.gov/tobacco/quit_smoking/index.htm
• Tobacco Use Cessation
http://www.cdc.gov/workplacehealthpromotion/implementation/topics/tobacco-use.html

38 39
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Box 6-2. Selected Web Resources (Continued)
CDC (Continued)
• Tips from Former Smokers
http://www.cdc.gov/tips/
• Implementing a Tobacco-Free Campus Initiative in Your Workplace
http://www.cdc.gov/nccdphp/dnpao/hwi/toolkits/tobacco/index.htm
• “Save Lives, Save Money: Make Your Business Smoke-Free”
http://www.cdc.gov/tobacco/basic_information/secondhand_smoke/guides/business/pdfs/
save_lives_save_money.pdf
• A Practical Guide to Working with Health-Care Systems on Tobacco-Use Treatment
http://www.cdc.gov/tobacco/quit_smoking/cessation/practical_guide/pdfs/practical_guide.pdf
• Total Worker Health™
http://www.cdc.gov/niosh/twh/
http://www.cdc.gov/niosh/twh/essentials.html
• Tobacco Smoke in the Workplace
http://www.cdc.gov/niosh/topics/tobacco/
Other
North American Quitline Consortium (NAQC)
• Quitline Map
http://map.naquitline.org/
American Lung Association
• Stop Smoking
http://www.lung.org/stop-smoking/
• Workplace Wellness
http://www.lung.org/stop-smoking/workplace-wellness/
American Cancer Society
• Great American Smokeout
http://www.cancer.org/healthy/stayawayfromtobacco/greatamericansmokeout/index
• “Strategies for Promoting a Smoke-free Workplace Policy”
http://www.cancer.org/downloads/gahc/hp_strategies_for_promoting_and_implementing_
smokefree_workplace.pdf
• Making Your Workplace Smokefree: A Decision Maker’s Guide
http://www.cancer.org/acs/groups/content/@highplains/documents/document/makingyour-
workplacesmokefreegu.pdf

38 39
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Box 6-2. Selected Web Resources (Continued)
American Heart Association
• Quit Smoking
http://www.heart.org/HEARTORG/GettingHealthy/QuitSmoking/Quit-Smoking_
UCM_001085_SubHomePage.jsp
American Legacy Foundation
• EX: A New Way to Think About Quitting Smoking
http://www.becomeanex.org
National Business Group on Health
• Tobacco: The Business of Quitting—An Employer’s Website for Tobacco Cessation
http://www.businessgrouphealth.org/tobacco/benets
PACT (Professional Assisted Cessation Therapy)
• Employers’ Tobacco Cessation Guide: Practical Approaches to a Costly Workplace Problem
http://www.elginhealth.on.ca/downloads/RIYSEQXL.pdf
is page intentionally le blank.
41
NIOSH CIB 67
•
Workplace Tobacco Policies
References
Achutan C, West C, Mueller C, Bernert JT, Bernard B
[2011]. Environmental tobacco smoke exposure among
casino dealers. J Occup Environ Med 53(4):346–351,
http://doi.org/10.1097/JOM.0b013e318212235f. Date
accessed: September 5, 2013.
ACPM (American College of Preventive Medicine)
[2013]. Commissioned Corps rst uniformed ser-
vice to prohibit tobacco use. ACPM Headlines, July
22, 2013, http://www.acpm.org/?Headlines072213.
Date accessed: September 5, 2013.
AIHA [2014]. White paper: electronic cigarettes in
the indoor environment. Falls Church, VA: Ameri-
can Industrial Hygiene Association, https://www.
aiha.org/government-affairs/Documents/Elec-
tronc%20Cig%20Document_Final.pdf. Date ac-
cessed: October 28, 2014.
ALA [undated]. Why quit smoking. Chicago: Amer-
ican Lung Association, http://www.lung.org/stop-
smoking/how-to-quit/why-quit/. Date accessed:
December 17, 2013.
Andrade M de, Hastings G [2013]. Tobacco harm
reduction nicotine containing products. Lon-
don: Cancer Research UK, http://www.cancer-
researchuk.org/prod_consump/groups/cr_com-
mon/@nre/@pol/documents/generalcontent/
tobacco-harm-reduction.pdf. Date accessed: Sep-
tember 22, 2014
ANR [2014]. Model policy for a smokefree work-
place. Berkeley, CA: Americans for Nonsmokers’
Rights, http://www.no-smoke.org/pdf/modelwork-
placepolicy.pdf. Date accessed: September 22, 2014.
ANRF [2014]. U.S. state and local laws regulat-
ing use of electronic cigarettes (as of July 3, 2014).
Berkeley, CA: Americans for Nonsmokers’ Rights
Foundation, http://www.no-smoke.org/pdf/ecig-
slaws.pdf. Date accessed: July 24, 2014.
Ahrens M [2010]. Butt out. NFPA J Jan/Feb:63–65.
Asch DA, Muller RW, Volpp KG [2013]. Con-
icts and compromises in not hiring smokers. N
Engl J Med 368:1371–1373, http://doi.org/10.1056/
NEJMp1303632. Date accessed: September 5, 2013.
ASHRAE [2013]. ASHRAE position document on
environmental tobacco smoke. Atlanta: Ameri-
can Society of Heating, Refrigerating and Air-
Conditioning Engineers, http://www.no-smoke.
org/pdf/ASHRAE_PD_Environmental_Tobacco_
Smoke_2013.pdf. Date accessed: December 5, 2013.
Babb S, McNeil C, Kruger J, Tynan MA [2015].
Second hand smoke and smoking restrictions in
casinos: a review of the evidence. Tob Control
24:11–17, http://dx.doi.org/10.1136/tobaccocon-
trol-2013-051368. Date accessed: February 5, 2013.
Balmes J, Becklake M, Blanc P, Henneberger P, Kre-
iss K, Mapp C, Milton D, Schwartz D, Toren K, Vie-
giG [2003]. American oracic Society statement:
occupational contribution to the burden of airway
disease. Am J Respir Crit Care Med 167:787–797,
http://doi.org/10.1164/rccm.167.5.787. Date ac-
cessed: September 5, 2013.
Bang KM, Kim JH [2001]. Prevalence of cigarette
smoking by occupation and industry in the United
States. Am J Ind Med 40(3):233–239, http://doi.
org/10.1002/ajim.1094. Date accessed: May 9, 2013.
Barbeau EM, Krieger N, Soobader MJ [2004]. Work-
ing class matters: socioeconomic disadvantage, race/
ethnicity, gender, and smoking in NHIS 2000. Am
J Public Health 94:269–278, http://doi.org/10.2105/
AJPH.94.2.269. Date accessed: May 9, 2013.
Barbeau EM, Li Y, Calderon P, Hartman C, Quinn
M, Markkanen P, Roelofs C, Frazier L, Levenstein C
[2006]. Results of a union-based smoking cessation
intervention for apprentice iron workers (United
States). Cancer Causes Control 17(1):53−61, http://
doi.org/10.1007/s10552-005-0271-0. Date ac-
cessed: July 5, 2013.
42 43
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Bauer JE, Hyland A, Li Q, Steger C, Cummings KM
[2005]. A longitudinal assessment of the impact
of smoke-free worksite policies on tobacco use.
Am J Public Health 95(6):1024–1029, http://doi.
org/10.2105/AJPH.2004.048678. Date accessed:
September 17, 2013.
Berman M, Crane R, Seiber E, Munur M [2013]. Es-
timating the cost of a smoking employee. Tob Con-
trol 23:428–433, http://doi.org/10.1136/tobaccocon-
trol-2012-050888. Date accessed: August 20, 2013.
Bhatnagar A, Whitsel LP, Ribisl KM, Bullen C,
Chaloupka F, Piano MR, Robertson RM, McAuley
T, Go D, Benowitz N, on behalf of the American
Heart Association Advocacy Coordinating Com-
mittee, Council on Cardiovascular and Stroke Nurs-
ing, Council on Clinical Cardiology, and Coun-
cil on Quality of Care and Outcomes Research
[2014]. Electronic cigarettes: a policy statement
from the American Heart Association. Circulation
130:Epub ahead of print, http://doi.org/10.1161/
CIR.0000000000000107. Date accessed: September
29, 2014.
BMA [2013]. BMA calls for stronger regulation
of e-cigarettes. London: British Medical Associa-
tion, Board of Science and the Occupational Medi-
cine Committee, http://bma.org.uk/-/media/Files/
PDFs/Working%20for%20change/Improving%20
health/tobaccoecigarettespublicplaces_jan2013.
pdf. Date accessed: July 29, 2013.
Brackbill R, Frazier T, Shilling S [1988]. Smok-
ing characteristics of US workers, 1978–1980.
Am J Ind Med 13(1):5–41, http://doi.org/10.1002/
ajim.4700130103. Date accessed: May 14, 2013.
Brown CJ, Cheng JM [2014]. Electronic ciga-
rettes: product characterization and design con-
siderations. Tob Control 23:ii4–ii10, http://doi.
org/10.1136/tobaccocontrol-2013-051476. Date
accessed: May 5, 2014.
Burstyn I [2014]. Peering through the mist: sys-
tematic review of what the chemistry of contam-
inants in electronic cigarettes tells us about
health risks. BMC Public Health 14:18, http://doi.
org/10.1186/1471-2458-14-18. Date accessed: Sep-
tember 22, 2014.
Cahill K, Lancaster T [2014]. Workplace interven-
tions for smoking cessation. Cochrane Database Syst
Rev 2:CD003440, http://doi.org/10.1002/14651858.
CD003440.pub4. Date accessed: May 28, 2014.
Cahill K, Perera R [2011]. Competitions and incen-
tives for smoking cessation. Cochrane Database Syst
Rev 4:CD004307, http://doi.org/10.1002/14651858.
CD004307.pub4. Date accessed: September 12, 2013.
Callinan JE, Clarke A, Doherty K, Kelleher C
[2010]. Legislative smoking bans for reducing sec-
ondhand smoke exposure, smoking prevalence and
tobacco consumption. Cochrane Database Syst Rev
4:CD005992, http://doi.org/10.1002/14651858.
CD005992.pub2. Date accessed: September 11, 2013.
Calvert GM, Luckhaupt SE, Sussell A, Dahlhamer
JM, Ward BW [2013]. e prevalence of selected
potentially hazardous workplace exposures in the
US: ndings from the 2010 National Health Inter-
view Survey. Am J Ind Med 56(6):635–646, http://
doi.org/10.1002/ajim.22089. Date accessed: July 18,
2013.
CDC [1987]. Polymer fume fever associated with
cigarette smoking and the use of tetrauoroeth-
ylene—Mississippi. MMWR Morb Mortal Wkly
Rep 36(31):515–516, 521–522, http://www.cdc.gov/
mmwr/preview/mmwrhtml/00051631.htm. Date
accessed: September 3, 2013.
CDC [1988]. Passive smoking: beliefs, attitudes,
and exposures—United States, 1986. MMWR Morb
Mortal Wkly Rep 37(15):239−241, http://www.cdc.
gov/mmwr/preview/mmwrhtml/00000014.htm.
Date accessed: December 11, 2013.
CDC [2004]. e benets of quitting. Poster. At-
lanta: Centers for Disease Control and Preven-
tion, http://www.cdc.gov/tobacco/data_statistics/
sgr/2004/posters/benets/. Date accessed: Decem-
ber 17, 2013.
CDC [2005]. CDC tobacco-free campus policy. At-
lanta: Centers for Disease Control and Prevention,
42 43
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
http://www.cdc.gov/nccdphp/dnpao/hwi/down-
loads/CDC_tobacco_policy.pdf. Date accessed:
September 22, 2014.
CDC [2006]. State-specic prevalence of current cig-
arette smoking among adults and secondhand smoke
rules and policies in homes and workplaces—Unit-
ed States, 2005. MMWR Morb Mortal Wkly Rep
55(42):1148−1151, http://www.cdc.gov/mmwr/pre-
view/mmwrhtml/mm5542a2.htm. Date accessed:
May 9, 2013.
CDC [2009]. State-specic secondhand smoke
exposure and current cigarette smoking among
adults—United States, 2008. MMWR Morb Mortal
Wkly Rep 58(44):1232−1235, http://www.cdc.gov/
mmwr/preview/mmwrhtml/mm5844a3.htm. Date
accessed: May 9, 2013.
CDC [2010]. State preemption of local smoke-
free laws in government work sites, private work
sites, and restaurants—United States, 2005−2009.
MMWR Morb Mortal Wkly Rep 59(04):105−108,
http://www.cdc.gov/mmwr/preview/mmwrhtml/
mm5904a4.htm. Date accessed: May 9, 2013.
CDC [2011a]. Current cigarette smoking prevalence
among working adults—United States, 2004–2010.
MMWR Morb Mortal Wkly Rep 60(38):1305–
1309, http://www.cdc.gov/mmwr/preview/mmwrht-
ml/mm6038a2.htm. Date accessed: May 14, 2013.
CDC [2011b]. Smoke-free laws for worksites, res-
taurants, and bars—United States, 2000−2010.
MMWR Morb Mortal Wkly Rep 60(15):472−475,
http://www.cdc.gov/mmwr/preview/mmwrhtml/
mm6015a2.htm. Date accessed: May 9, 2013.
CDC [2012]. Comprehensive smoke-free laws—50
largest U.S. cities, 2000 and 2012. MMWR Morb
Mortal Wkly Rep 61(45):914−917, http://www.cdc.
gov/mmwr/preview/mmwrhtml/mm6145a3.htm.
Date accessed: May 9, 2013.
CDC [2013a]. Winnable battles. Atlanta: Centers
for Disease Control and Prevention, http://www.
cdc.gov/winnablebattles/index.html. Date ac-
cessed: April 3, 2013.
CDC [2013b]. Trends in Current Cigarette Smok-
ing Among High School Students and Adults,
United States, 1965–2011. Atlanta: Centers for Dis-
ease Control and Prevention, http://www.cdc.gov/
tobacco/data_statistics/tables/trends/cig_smok-
ing/. Date accessed: July 18, 2013.
CDC [2013c]. Obliterative bronchiolitis in workers
in a coee-processing facility—Texas, 2008–2012.
MMWR Morb Mortal Wkly Rep 62(16):305−307,
http://www.cdc.gov/mmwr/preview/mmwrhtml/
mm6216a3.htm. Date accessed: May 28, 2014.
CDC [2014a]. Current smokeless tobacco use
among working adults—United States, 2005 and
2010. MMWR Morb Mortal Wkly Rep 63:477–482,
http://www.cdc.gov/mmwr/preview/mmwrhtml/
mm6322a1.htm?s_cid=mm6322a1_e. Date ac-
cessed: June 12, 2014.
CDC [2014b]. Coverage for tobacco use cessation
treatments. Brochure, updated February 2014. At-
lanta: Centers for Disease Control and Prevention,
http://www.cdc.gov/tobacco/quit_smoking/cessa-
tion/pdfs/coverage.pdf. Date accessed: May 27, 2014.
CDC [2014c]. State laws prohibiting sales to mi-
nors and indoor use of electronic nicotine deliv-
ery—United States, 2014. MMWR Morb Mortal
Wkly Rep 63(49):1145–1150, http://www.cdc.gov/
mmwr/preview/mmwrhtml/mm6349a1.htm. Date
accessed: January 20, 2015.
CDC [2014d]. Current cigarette smoking among
adults—United States, 2005–2013. MMWR Morb
Mortal Wkly Rep 63(47):1108−1112, http://www.
cdc.gov/mmwr/preview/mmwrhtml/mm6347a4.
htm. Date accessed: February 4, 2015.
Cheng T [2014]. Chemical evaluation of electronic
cigarettes. Tob Control 23(suppl 2):ii11–ii17, http://
doi.org/10.1136/tobaccocontrol-2013-051482.
Date accessed: May 28, 2014.
Chin DL, Hong O, Gillen M, Bates MN, Okechuk-
wu CA [2012]. Cigarette smoking in building trades
workers: the impact of work environment. Am J
Ind Med 55(5):429–439, http://doi.org/10.1002/
ajim.22031. Date accessed: September 19, 2013.
44 45
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Civljak M, Stead LF, Hartmann-Boyce J, Sheikh
A, Car J [2013]. Internet-based interventions for
smoking cessation. Cochrane Database Syst Rev
7:CD007078, http://doi.org/10.1002/14651858.
CD007078.pub4. Date accessed: September 26, 2014.
Clinical Practice Guideline for Treating Tobacco
Use and Dependence 2008 Update Panel, Liaisons,
and Sta [2008]. A clinical practice guideline for
treating tobacco use and dependence: 2008 up-
date: a U.S. Public Health Service report. Am J
Prev Med 35(2):158–176, http://doi.org/10.1016/j.
amepre.2008.04.009. Date accessed: May 1, 2013.
CMS [2014]. State specic rating variations. Balti-
more: Centers for Medicare & Medicaid Services,
http://www.cms.gov/CCIIO/Programs-and-Initia-
tives/Health-Insurance-Market-Reforms/state-rat-
ing.html. Date accessed: February 5, 2015.
Cook DM, Bero LA [2009]. e politics of smoking
in federal buildings: an executive order case study.
Am J Public Health 99(9):1588–1595, http://doi.
org/10.2105/AJPH.2008.151829. Date Accessed:
September 4, 2009.
Covey LS, Zang EA, Wynder EL [1992]. Cigarette
smoking and occupational status: 1977 to 1990.
Am J Public Health 82:1230–1234, http://doi.
org/10.2105/AJPH.82.9.1230. Date accessed: May
10, 2013.
Craig BN, Congleton JJ, Kerk CJ, Amendola AA,
Gaines WG [2006]. Personal and non-occupa-
tional risk factors and occupational injury/illness.
Am J Ind Med 49:249–260, http://doi.org/10.1002/
ajim.20290. Date accessed: September 5, 2013.
Cruickshanks KJ, Klein R, Klein BEK, Wiley TL,
Nondahl DM, Tweed TS [1998]. Cigarette smok-
ing and hearing loss: the epidemiology of hearing
loss study. JAMA 279(21):1715‒1719, http://doi.
org/10.1001/jama.279.21.1715. Date accessed: Feb-
ruary 12, 2014.
DHEW [1964]. Smoking and health: report of
the advisory committee to the Surgeon General
of the Public Health Service. Washington, DC:
U.S. Department of Health, Education, and Wel-
fare, Public Health Service, Center for Disease
Control, PHS Publication No. 1103, http://proles.
nlm.nih.gov/NN/B/B/M/Q/. Date accessed: April
3, 2013.
DHEW [1979a]. Healthy People: the Surgeon Gen-
eral’s report on health promotion and disease preven-
tion. Washington, DC: U.S. Department of Health
and Human Services, Public Health Service, Oce of
the Assistant Secretary for Health and Surgeon Gen-
eral, DHEW (PHS) Publication No. 79-55071, http://
proles.nlm.nih.gov/ps/retrieve/ResourceMetadata/
NNBBGK. Date accessed: April 3, 2013.
DHEW [1979b]. Smoking and health: a report of
the Surgeon General. Washington, DC: U.S. De-
partment of Health and Human Services, Public
Health Service, Oce on Smoking and Health,
DHEW Publication No. (PHS) 79-50066, http://
proles.nlm.nih.gov/ps/retrieve/ResourceMetada-
ta/NNBCMD. Date accessed: April 3, 2013.
DHHS [1982]. e health consequences of smok-
ing: cancer. A report of the Surgeon General. Rock-
ville, MD: U.S. Department of Health and Human
Services, Public Health Service, Oce on Smok-
ing and Health, DHHS Publication No. (PHS) 82-
50179, http://proles.nlm.nih.gov/NN/B/C/D/W/.
Date accessed: April 3, 2013.
DHHS [1983]. e health consequences of smok-
ing: cardiovascular disease. A report of the Sur-
geon General. Rockville, MD: U.S. Department of
Health and Human Services, Public Health Service,
Oce on Smoking and Health, DHHS Publication
No. (PHS) 84-50204, http://proles.nlm.nih.gov/
NN/B/B/T/D/. Date accessed: April 3, 2013.
DHHS [1984]. e health consequences of smok-
ing: chronic obstructive lung disease. A report of
the Surgeon General. Rockville, MD: U.S. Depart-
ment of Health and Human Services, Public Health
Service, Oce on Smoking and Health, DHHS Pub-
lication No. (PHS) 84-50205, http://proles.nlm.nih.
gov/NN/B/C/C/S/. Date accessed: April 3, 2013.
44 45
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
DHHS [1985]. e health consequences of smoking:
cancer and chronic lung disease in the workplace. A
report of the Surgeon General. Rockville, MD: U.S.
Department of Health and Human Services, Pub-
lic Health Service, Oce on Smoking and Health,
DHHS Publication No. (PHS) 85-50207, http://
proles.nlm.nih.gov/NN/B/C/B/N/. Date accessed:
April 3, 2013.
DHHS [1986a]. e health consequences of using
smokeless tobacco: a report of the advisory com-
mittee to the Surgeon General. Bethesda, MD: U.S.
Department of Health and Human Services, Pub-
lic Health Service, NIH Publication No. 86-2874,
http://proles.nlm.nih.gov/NN/B/B/F/C/. Date ac-
cessed: April 3, 2013.
DHHS [1986b]. e health consequences of involun-
tary smoking: a report of the Surgeon General. Rock-
ville, MD: U.S. Department of Health and Human
Services, Public Health Service, Centers for Disease
Control, Center for Health Promotion and Educa-
tion, Oce on Smoking and Health, DHHS Publica-
tion No. (CDC) 87-8398, http://proles.nlm.nih.gov/
NN/B/C/P/M/. Date accessed: April 3, 2013.
DHHS [1990]. e health benets of smoking ces-
sation: a report of the Surgeon General. Atlanta:
U.S. Department of Health and Human Services,
Public Health Service, Centers for Disease Con-
trol, National Center for Chronic Disease Preven-
tion and Health Promotion, Oce on Smoking and
Health, DHHS Publication No. (CDC) 90-8416,
http://proles.nlm.nih.gov/NN/B/B/C/T/. Date ac-
cessed: April 3, 2013.
DHHS [1996]. Making your workplace smoke-
free: a decision maker’s guide. U.S. Department
of Health and Human Services, Centers for Dis-
ease Control and Prevention, Oce on Smoking
and Health (with Wellness Councils of America
and American Cancer Society), http://libres.uncg.
edu/ir/uncg/f/J_Eddy_Making_1996.pdf. Date ac-
cessed: September 10, 2013.
DHHS [2000]. Reducing tobacco use: a report of
the Surgeon General. Atlanta: U.S. Department of
Health and Human Services, Centers for Disease
Control and Prevention, National Center for Chron-
ic Disease Prevention and Health Promotion, Oce
on Smoking and Health, http://www.cdc.gov/tobac-
co/data_statistics/sgr/2000/complete_report/index.
htm. Date accessed: April 3, 2013.
DHHS [2001]. Women and smoking: a report of
the Surgeon General. Atlanta: U.S. Department
of Health and Human Services, Centers for Dis-
ease Control and Prevention, National Center for
Chronic Disease Prevention and Health Promo-
tion, Oce on Smoking and Health, http://www.
cdc.gov/tobacco/data_statistics/sgr/2001/com-
plete_report/index.htm. Date accessed: December
18, 2013.
DHHS [2004]. e health consequences of smok-
ing: a report of the Surgeon General. Atlanta: U.S.
Department of Health and Human Services, Cen-
ters for Disease Control and Prevention, National
Center for Chronic Disease Prevention and Health
Promotion, Oce on Smoking and Health, http://
www.cdc.gov/tobacco/data_statistics/sgr/2004/in-
dex.htm. Date accessed: 5/1/13.
DHHS [2006]. e health consequences of invol-
untary exposure to tobacco smoke. A report of the
Surgeon General. U.S. Department of Health and
Human Services, Centers for Disease Control and
Prevention, Coordinating Center for Health Pro-
motion, National Center for Chronic Disease Pre-
vention and Health Promotion, Oce on Smoking
and Health, http://www.ncbi.nlm.nih.gov/books/
NBK44324/. Date accessed: May 1, 2013.
DHHS [2010a]. Ending the tobacco epidemic: a
tobacco control strategic action plan for the U.S.
Department of Health and Human Services. Wash-
ington, DC: U.S. Department of Health and Hu-
man Services, Oce of the Assistant Secretary for
Health, November 2010, http://www.hhs.gov/ash/
initiatives/tobacco/tobaccostrategicplan2010.pdf.
Date accessed: April 3, 2013.
DHHS [2010b]. How tobacco smoke causes dis-
ease: the biology and behavioral basis for smoking-
attributable disease. A report of the surgeon gener-
al. Atlanta: U.S. Department of Health and Human
46 47
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Services, Centers for Disease Control and Preven-
tion, National Center for Chronic Disease Preven-
tion and Health Promotion, Oce on Smoking
and Health, http://www.ncbi.nlm.nih.gov/books/
NBK53017/. Date Accessed: December 12, 2013.
DHHS [2012]. Preventing tobacco use among youth
and young adults. A report of the surgeon general.
Atlanta: U.S. Department of Health and Human
Services, Centers for Disease Control and Preven-
tion, National Center for Chronic Disease Preven-
tion and Health Promotion, Oce on Smoking and
Health, http://www.cdc.gov/tobacco/data_statistics/
sgr/2004/index.htm. Date accessed: April 3, 2013.
DHHS [2013]. Healthy People 2020: tobacco use
objectives. U.S. Department of Health and Human
Services, http://www.healthypeople.gov/2020/top-
icsobjectives2020/objectiveslist.aspx?topicId=41.
Date accessed: April 3, 2013.
DHHS [2014]. e health consequences of smok-
ing: 50 years of progress. A report of the surgeon
general. Atlanta: U.S. Department of Health and
Human Services, Centers for Disease Control
and Prevention, National Center for Chronic Dis-
ease Prevention and Health Promotion, Oce on
Smoking and Health, http://www.cdc.gov/tobacco/
data_statistics/sgr/50th-anniversary/index.htm.
Date accessed: January 21, 2014.
Dietz NA, Lee DJ, Fleming LE, LeBlanc WG, Mc-
Collister KE, Arheart KL, Davila EP, Caban-Mar-
tinez AJ [2011]. Trends in smokeless tobacco use
in the US workforce: 1987−2005. Tob Induc Dis
9(1):6, http://doi.org/10.1186/1617-9625-9-6. Date
accessed: April 18, 2013.
Drummond MB, Upson D [2014]. Electronic cig-
arettes: potential harms and benets. Ann Am
orac Soc 11(2):236-242, http://doi.org/10.1513/
AnnalsATS.201311-391FR. Date accessed: May 5,
2014.
Eisner MD, Smith AK, Blanc PD [1998]. Bartend-
ers’ respiratory health aer establishment of smoke-
free bars and taverns. JAMA 280(22):1909−1914,
http://doi.org/10.1001/jama.280.22.1909. Date ac-
cessed: July 5, 2013.
Fabry DA, Davila EP, Arheart KL, Serdar B, Di-
etz NA, Bandiera FC, Lee DL [2011]. Second-
hand smoke exposure and the risk of hearing loss.
Tob Control 20:82−85, http://doi.org/10.1136/
tc.2010.035832. Date accessed: May 10, 2013.
Farsalinos KE, Polosa R [2014]. Safety evalua-
tion and risk assessment of electronic cigarettes
as tobacco cigarette substitutes: a systematic re-
view. er Adv Drug Saf 5(2):67–86, http://doi.
org/10.1177/2042098614524430. Date accessed:
May 5, 2014.
FDA [2009]. Evaluation of e-cigarettes. Memoran-
dum, May 4, 2009. Washington, DC: U.S. Food and
Drug Administration. http://www.fda.gov/down-
loads/drugs/scienceresearch/ucm173250.pdf. Date
accessed: July 29, 2013.
73 Fed. Reg. 77517 [2008]. General Services Ad-
ministration: federal management regulation; FMR
case 2008-102-3, real property policies update –
smoking restrictions, nal rule. To be codied at 45
CFR Part 102. http://www.gpo.gov/fdsys/pkg/FR-
2008-12-19/html/E8-30180.htm. Date accessed:
February 5, 2015.
78 Fed. Reg. 33158 [2013]. Internal Revenue Ser-
vice, Employee Benets Security Administration,
Centers for Medicare and Medicaid Services: in-
centives for nondiscriminatory wellness programs
in group health plans; nal rule. To be codied at
26 CFR Part 54, 29 CFR Part 2590, and 45 CFR
Parts 146 and 147. http://www.gpo.gov/fdsys/
pkg/FR-2013-06-03/pdf/2013-12916.pdf. Date ac-
cessed: July 22, 2014.
FGIRA [2012]. Liquids from e-cigarettes can be
detrimental to health. BfR opinion no. 016/2012.
Berlin: Federal German Institute for Risk Assess-
ment, http://www.bfr.bund.de/cm/349/liquids-
from-e-cigarettes-can-be-detrimental-to-health.
pdf. Date accessed: May 5, 2014.
Fichtenberg CM, Glantz SA [2002]. Eect of smoke-
free workplaces on smoking behaviour: systematic
review. BMJ 325:188−191, http://doi.org/10.1136/
bmj.325.7357.188. Date accessed: July 5, 2013.
46 47
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Flouris AD, Chorti MS, Poulianiti KP, Jamurtas
AZ, Kostikas K, Tzatzarakis MN, Wallace Hayes A,
Tsatsaki AM, Koutedakis Y [2013]. Acute impact
of active and passive electronic cigarette smoking
on serum cotinine and lung function. Inhal Toxicol
25(2):91–101, http://doi.org/10.3109/08958378.201
2.758197. Date accessed: July 23, 2013.
Frost G, Darnton A, Harding AH [2011]. e eect
of smoking on the risk of lung cancer mortality for
asbestos workers in Great Britain (1971−2005). Ann
Occup Hyg 55(3):239−247, http://doi.org/10.1093/
annhyg/meq089. Date accessed: May 1, 2013.
Fujishiro K, Stukovsky KD, Roux AD, Landsbergis P,
Burchel C [2012]. Occupational gradients in smok-
ing behavior and exposure to workplace environ-
mental tobacco smoke: the Multi-Ethnic Study of
Atherosclerosis. Occup Environ Med 54(2):136–145,
http://doi.org/10.1097/JOM.0b013e318244501e.
Date accessed: May 9, 2013.
Gay R [2013]. Banning electronic cigarettes in the
workplace. HR Hero Line, September 11, http://
www.hrhero.com/hl/articles/2013/09/11/banning-
electronic-cigarettes-in-the-workplace/. Date ac-
cessed: September 30, 2014.
GCPS [2005]. Reducing tobacco use and second-
hand smoke exposure: incentives and competitions
to increase smoking cessation among workers.
Guide to Community Preventive Services, June,
http://www.thecommunityguide.org/tobacco/in-
centives.html. Date accessed: July 3, 2013.
GCPS [2012a]. Reducing tobacco use and second-
hand smoke exposure: smoke-free policies. Guide to
Community Preventive Services, November, http://
www.thecommunityguide.org/tobacco/RRsmoke-
freepolicies.html. Date accessed: September 5, 2013.
GCPS [2012b]. Reducing tobacco use and second-
hand smoke exposure: quitline interventions. Guide
to Community Preventive Services, August, http://
www.thecommunityguide.org/tobacco/quitlines.
html. Date accessed: July 3, 2013.
GCPS [2012c]. Reducing tobacco use and second-
hand smoke exposure: reducing out-of-pocket
costs for evidence based tobacco cessation treat-
ments. Guide to Community Preventive Services,
August, http://www.thecommunityguide.org/to-
bacco/outofpocketcosts.html. Date accessed: July
3, 2013.
Gennimata S-A, Palamidas A , Kaltsakas G, Tsi-
krika S, Vakali S, Gratziou C, Koulouris N [2012].
Acute eect of e-cigarette on pulmonary function
in healthy subjects and smokers [abstract for 22
nd
Annual Congress]. Eur Respir J 40(Suppl 56):197s,
http://www.ers-education.org/ersMade/abstract_
print_12/les/Abstract_book_2012.pdf. Date ac-
cessed: May 5, 2014.
Goniewicz ML, Knysak J, Gawron M, Kosmider
L, Sobczak A, Kurek J, Prokopowicz A, Jablons-
ka-Czapla M, Rosik-Dulewska C, Havel C, Jacob
P 3rd, Benowitz N [2014]. Levels of selected car-
cinogens and toxicants in vapour from electronic
cigarettes. Tob Control 23(2):133–139, http://doi.
org/10.1136/tobaccocontrol-2012-050859. Date
accessed: May 5, 2014.
Gra SK [2008]. ere is no constitutional right
to smoke. 2nd ed. St. Paul, MN: Tobacco Control
Legal Consortium, http://publichealthlawcen-
ter.org/resources/there-no-constitutional-right-
smoke-2008. Date accessed: September 2, 2014.
Graham AL, Cobb NK, Raymond L, Sill S, Young
J [2007]. Eectiveness of an Internet-based work-
site smoking cessation intervention at 12 months.
J Occup Environ Med 49(8):821–828, http://doi.
org/10.1097/JOM.0b013e3180d09e6f. Date ac-
cessed: September 26, 2014.
Grana R, Benowitz N, Glantz S [2014]. E-cigarettes:
a scientic review. Circulation 2014 129(19):1972–
1986, http://dx.doi.org/10.1161/CIRCULA-
TIONAHA.114.007667. Data accessed: January 20,
2015.
Hahn EJ [2010]. Smokefree legislation: a review
of health and economic outcomes research. Am
J Prev Med 39(6 Suppl 1):S66−S76, http://doi.
org/10.1016/j.amepre.2010.08.013. Date accessed:
July 5, 2013.
48 49
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Hall JR Jr [2013]. e smoking-material re prob-
lem. Washington, Quincy, MA: National Fire
Protection Association, July, http://www.nfpa.
org/~/media/Files/Research/NFPA%20reports/
Major%20Causes/ossmoking.pdf. Date accessed:
October 3, 2014.
Ham DC, Przybeck T, Strickland JR, Luke DA,
Bierut LJ, Evano BA [2011]. Occupation and work-
place policies predict smoking behaviors: analysis
of national data from the Current Population Sur-
vey. Occup Environ Med 53(11):1337–1345, http://
doi.org/10.1097/JOM.0b013e3182337778. Date ac-
cessed: July 5, 2013.
Hammond SK [1999]. Exposure of U.S. work-
ers to environmental tobacco smoke. Environ
Health Perspect 107(Suppl 2):329–340, http://doi.
org/10.2307/3434425. Date accessed May 9, 2013.
Hammond SK, Sorensen G, Youngstrom R, Ockene
JK [1995]. Occupational exposure to environmen-
tal tobacco smoke. JAMA 274(12):956−960, http://
doi.org/10.1001/jama.1995.03530120048040. Date
accessed: May 10, 2013.
Henneberger PK, Redlich CA, Callahan DB, Har-
ber P, Lemière C, Martin J, Tarlo SM, Vandenplas O,
Torén K; ATS Ad Hoc Committee on Work-Exac-
erbated Asthma [2011]. An ocial American o-
racic Society statement: work-exacerbated asthma.
Am J Respir Crit Care Med 184(3):368−378, http://
doi.org/10.1164/rccm.812011ST. Date accessed
July 31, 2013.
Herman PM, Walsh ME [2011]. Hospital admis-
sions for acute myocardial infarction, angina, stroke,
and asthma aer implementation of Arizona’s
comprehensive statewide smoking ban. Am J Pub
Health 101(3):491–496, http://doi.org/10.2105/
AJPH.2009.179572. Date accessed: December 9, 2013.
Hopkins DP, Razi S, Leeks KD, Priya Kalra G,
Chattopadhyay SK, Soler RE [2010]. Smokefree
policies to reduce tobacco use: a systematic review.
Am J Prev Med 38(2 Suppl):S275–S289, http://doi.
org/10.1016/j.amepre.2009.10.029. Date accessed:
September 5, 2013.
Howard J [2004]. Smoking is an occupational
hazard. Am J Ind Med 46:161–169, http://doi.
org/10.1002/ajim.10364. Date accessed: May 5,
2014.
Howard J, Weissman D, Chosewood C [2010].
Warning: Surgeon General nds that cigarette
smoking is even more dangerous to your health.
NIOSH Science Blog, December 10, http://blogs.
cdc.gov/niosh-science-blog/2010/12/smoking/.
Date accessed: April 3, 2013.
Hughes MC, Yette EM, Hannon PA, Harris JR,
Tran NM, Reid TR [2011]. Promoting tobacco
cessation via the workplace: opportunities for im-
provement. Tob Control 20(4):305−308, http://doi.
org/10.1136/tc.2010.041038. Date accessed: July 5,
2013.
Hymel PA, Loeppke RR, Baase CM, Burton
WN, Hartenbaum NP, Hudson TW, McLellan
RK, Mueller KL, Roberts MA, Yarborough CM,
Konicki DL, Larson PW [2011]. Workplace health
protection and promotion: a new pathway for a
healthier—and safer—workforce. J Occup Envi-
ron Med 53(6):695–702, http://doi.org/10.1097/
JOM.0b013e31822005d0. Date accessed: Septem-
ber 11, 2013.
IARC [2004]. Tobacco smoke and involuntary
smoking. In: IARC Monographs on the Evaluation
of Carcinogenic Risks to Humans. Vol. 83. Lyon,
France: World Health Organization, International
Agency for Research on Cancer, http://mono-
graphs.iarc.fr/ENG/Monographs/vol83/mono83.
pdf. Date accessed: September 19, 2014.
IARC [2009]. Evaluating the eectiveness of
smoke-free policies. In: IARC Handbooks of Can-
cer Prevention, Tobacco Control, Vol. 13. Lyon,
France: World Health Organization, International
Agency for Research on Cancer, http://www.iarc.
fr/en/publications/pdfs-online/prev/handbook13/
handbook13-0.pdf. Date accessed: December 9,
2013.
IARC [2012]. A review of human carcinogens: per-
sonal habits and indoor combustions. In: IARC
48 49
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Monographs on the Evaluation of Carcinogenic
Risks to Humans, Vol. 100E. Lyon, France: World
Health Organization, International Agency for Re-
search on Cancer, http://monographs.iarc.fr/ENG/
Monographs/vol100E/mono100E.pdf. Date ac-
cessed: May 1, 2013.
Ingebrethsen BJ, Cole SK, Alderman SL [2012].
Electronic cigarette aerosol particle size distribu-
tion measurements. Inhal Toxicol 24(14):976–984,
http://doi.org/10.3109/08958378.2012.744781.
Date accessed: July 29, 2013.
IOM (Institute of Medicine) [2010]. Secondhand
Smoke Exposure and Cardiovascular Eects: Mak-
ing Sense of the Evidence. Washington, DC: e
National Academies Press, http://www.nap.edu/
openbook.php?record_id=12649&page=R1. Date
accessed: December 9, 2013.
Kamerow D [2013]. Big Tobacco lights up e-ciga-
rettes. BMJ 346:f3418, http://doi.org/10.1136/bmj.
f3418. Date accessed: July 23, 2013.
Karp G [2007]. Smoking harms nancial health too;
pack-a-day habit can cost $2,000 annually. Chicago
Tribune, February 11, http://articles.chicagotri-
bune.com/2007-02-11/business/0702110019_1_
collateral-spending-public-indoor-places-smok-
ers. Date accessed: September 18, 2013.
King BA, Homa DM, Dube SR, Babb SD [2014].
Exposure to secondhand smoke and attitudes to-
ward smoke-free workplaces among employed U.S.
adults: ndings from the National Adult Tobacco
Survey. Nicotine Tob Res 16(10):1307–1318, http://
doi.org/10.1093/ntr/ntu069. Date accessed: May
27, 2014.
King BA, Patel R, Nguyen K, Dube SR [2015].
Trends in awareness and use of electronic cigarettes
among U.S. Adults, 2010–2013. Nicotine Tob Res
17(2):219–227, http://doi.org/10.1093/ntr/ntu191.
Date accessed: February 5, 2015.
Kofman M, Dunton K, Senkewicz MB [2012]. Im-
plementation of tobacco cessation coverage under
the Aordable Care Act: understanding how private
health insurance policies cover tobacco cessation
treatments. Washington, DC: Georgetown Univer-
sity Health Policy Institute, November 26, http://
www.tobaccofreekids.org/pressoce/2012/george-
town/coveragereport.pdf. Date accessed: Septem-
ber 13, 2013.
Kuempel ED, Wheeler MW, Smith RJ, Vallyathan V,
Green FHY [2009]. Contributions of dust exposure
and cigarette smoking to emphysema severity in
coal miners in the U.S. Am J Respir Crit Care Med
180:257−264, http://doi.org/10.1164/rccm.200806-
840OC. Date accessed: May 10, 2013.
Lee DJ, Fleming LE, Arheart KL, LeBlanc WG, Ca-
ban AJ, Chung-Bridges K, Christ SL, McCollister
KE, Pitman T [2007]. Smoking rate trends in U.S. oc-
cupational groups: the 1987 to 2004 National Health
Interview Survey. J Occup Environ Med 49(1):75–
81, http://doi.org/10.1097/JOM.0b013e31802ec68c.
Date accessed: May 15, 2013.
Lee DJ, LeBlanc W, Fleming LE, Gomez-Marin
O, Pitman T [2004]. Trends in US smoking rates
in occupational groups: the National Health In-
terview Survey 1987–1994. J Occup Environ
Med 46(6):538−548, http://doi.org/10.1097/01.
jom.0000128152.01896.ae. Date accessed: May 14,
2013.
Leistikow BN, Martin DC, Jacobs J, Rocke DM, No-
derer K [2000a]. Smoking as a risk factor for accident
death: a meta-analysis of cohort studies. Accid Anal
Prev 32:397–405, http://doi.org/10.1016/S0001-
4575(99)00034-2. Date accessed: April 18, 2013.
Leistikow BN, Martin DC, Milano CE [2000b].
Fire injuries, disasters, and costs from cigarettes
and cigarette lights: a global overview. Prev Med
31:91–99, http://doi.org/10.1006/pmed.2000.0680.
Date accessed: April 18, 2013.
Lichtenstein E, Zhu S-H, Tedeschi GJ [2010]. Smok-
ing cessation quitlines: an underrecognized inter-
vention success story. Am Psychol 65(4):252–261,
http://doi.org/10.1037/a0018598. Date accessed:
May 28, 2014.
50 51
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Lincoln AE, Smith GS, Amoroso PJ, Bell NS [2003].
e eect of cigarette smoking on musculoskeletal-
related disability. Am J Ind Med 43:337–349, http://
doi.org/10.1002/ajim.10195. Date accessed: April
11, 2013.
Longo DR, Brownson RC, Kruse RL [1995]. Smok-
ing bans in US hospitals: results of a national sur-
vey. JAMA 274(6):488–491, http://doi.org/10.1001/
jama.1995.03530060062035. Date accessed: Sep-
tember 4, 2013.
Mackay D, Haw S, Ayres JG, Fischbacher C, Pell JP
[2010]. Smoke-free legislation and hospitalizations
for childhood asthma. N Engl J Med 363:1139–
1145, http://doi.org/10.1056/NEJMoa1002861.
Date accessed: November 5, 2013.
Madison K, Schmidt H, Volpp KG [2013]. Smok-
ing, obesity, health insurance, and health incentives
in the Aordable Care Act. JAMA 310(2):143–144,
http://doi.org/10.1001/jama.2013.7617. Date ac-
cessed: November 5, 2013.
Madison KM, Volpp KG, Halpern SD [2011]. e
law, policy, and ethics of employers’ use of health
incentives to improve health. J Law Med Ethics
39(3):450–468, http://onlinelibrary.wiley.com/
doi/10.1111/j.1748-720X.2011.00614.x/pdf. Date
accessed: August 20, 2013.
Markowitz SB, Levin SM, Miller A, Morabia A
[2013]. Asbestos, asbestosis, smoking, and lung
cancer: new ndings from the North Ameri-
can insulator cohort. Am J Respir Crit Care Med
188(1):90−96, http://doi.org/10.1164/rccm.201302-
0257OC. Date accessed: July 24, 2013.
McAfee T, Babb S, McNabb S, Fiore MC [2015].
Helping smokers quit—opportunities created by
the Aordable Care Act. N Eng J Med 372:5–7,
http://dx.doi.org/10.1056/NEJMp1411437. Date
accessed: February 5, 2013.
McAuley TR, Hopke PK, Zhao J, Babaian S [2012].
Comparison of the eects of e-cigarette vapor and
cigarette smoke in indoor air quality. Inhal Toxicol
24(12):850−857, http://doi.org/10.3109/08958378.
2012.724728. Date accessed: July 23, 2013.
McGoldrick DE, Boonn AV [2010]. Public policy
to maximize tobacco cessation. Am J Prev Med
38(3 Suppl):S327−S332, http://doi.org/10.1016/j.
amepre.2009.11.017. Date accessed: July 5, 2013.
McVary KT, Carrier S, Wessells H, Subcommittee on
Smoking and Erectile Dysfunction Socioeconomic
Committee, Sexual Medicine Society of North
America [2001]. Smoking and erectile dysfunction:
evidence based analysis. J Urol 166(5):1624–1632,
http://doi.org/10.1016/S0022-5347(05)65641-8.
Date accessed: August 28, 2013.
Mejia AB, Ling PM [2010]. Tobacco industry con-
sumer research on smokeless tobacco users and prod-
uct development. Am J Public Health 100:78−87,
http://doi.org/10.2105/AJPH.2008.152603. Date ac-
cessed: April 18, 2013.
MIFACE [2006]. Young adult female waitress died
from an asthma attack while working at a bar. MI-
FACE (Michigan Fatality Assessment and Con-
trol Evaluation) Investigation #04MI223. Michi-
gan State University, http://www.oem.msu.edu/
MiFace/04MI223v1.pdf. Date accessed: May 7, 2013.
Moore M [2014]. E-cigarettes create burning ques-
tions for employers. Boston Bus J, June 5, http://
www.bizjournals.com/boston/news/2014/06/05/e-
cigarettes-create-burning-questions-for.
html?page=all. Date accessed: September 30, 2014.
MSHA [2000]. Winter’s approach heightens mine
explosion concern. News release no. 2000-1023.
Arlington, VA: U.S. Department of Labor, Mine
Safety and Health Administration, http://www.
msha.gov/MEDIA/PRESS/2000/NR001023.HTM.
Date accessed: April 11, 2013.
NBGH [2013]. Tobacco: the business of quitting—
an employer’s website for tobacco cessation. Wash-
ington, DC: National Business Group on Health,
http://www.businessgrouphealth.org/tobacco/.
Date accessed: September 25, 2013.
Nelson DE, Emont SL, Brackbill RM, Cameron
LL, Peddicord J, Fiore MC [1994]. Cigarette smok-
ing prevalence by occupation in the United States:
50 51
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
a comparison between 1978 to 1980 and 1987 to
1990. J Occup Med 36(5):516−525, http://jour-
nals.lww.com/joem/Abstract/1994/05000/Ciga-
rette_Smoking_Prevalence_by_Occupation_in_
the.9.aspx. Date accessed: April 3, 2013.
NHTSA [2009]. An examination of driver distrac-
tion as recorded in NHTSA databases. Trac safety
facts research note. DOT HS 811 216. Washington,
DC: National Highway Trac Safety Administra-
tion, http://www-nrd.nhtsa.dot.gov/Pubs/811216.
pdf. Date accessed: December 17, 2013.
NIOSH [1972]. Criteria for a recommended stan-
dard: occupational exposure to asbestos. Cincin-
nati, OH: U.S. Department of Health, Education,
and Welfare, Health Services and Mental Health
Administration, National Institute for Occupation-
al Safety and Health, DHHS (NIOSH) Publication
No. HSM 72-10267, http://www.cdc.gov/niosh/
docs/72-10267/pdfs/7210267.pdf. Date accessed:
April 3, 2013.
NIOSH [1979]. NIOSH current intelligence bulle-
tin 31: adverse health eects of smoking and the
occupational environment. Cincinnati, OH: U.S.
Department of Health, Education, and Welfare,
Center for Disease Control, National Institute for
Occupational Safety and Health. DHEW (NIOSH)
Publication Number 79-122, http://www.cdc.gov/
niosh/docs/1970/79122_31.html. Date accessed:
May 1, 2013.
NIOSH [1980]. Workplace exposure to asbestos:
review and recommendations. U.S. Department of
Health, Education, and Welfare, Center for Disease
Control, National Institute for Occupational Safety
and Health, DHHS (NIOSH) Publication No. 81-
103, http://www.cdc.gov/niosh/docs/81-103/. Date
accessed: April 3, 2013.
NIOSH [1991]. Current intelligence bulletin 54: en-
vironmental tobacco smoke in the workplace; lung
cancer and other health eects. Cincinnati, OH:
U.S. Department of Health and Human Services,
Center for Disease Control, National Institute for
Occupational Safety and Health, DHHS (NIOSH)
Publication No. 91-108, http://www.cdc.gov/niosh/
docs/91-108/. Date accessed: April 3, 2013.
NIOSH [2004]. Preventing lung disease in work-
ers who use or make avorings. Cincinnati, OH:
U.S. Department of Health and Human Services,
Centers for Disease Control and Prevention, Na-
tional Institute for Occupational Safety and Health,
DHHS (NIOSH) Publication No. 2004-110, http://
www.cdc.gov/niosh/docs/2004-110/pdfs/2004-
110.pdf. Date accessed: May 28, 2014.
NIOSH [2006]. Criteria for a recommended stan-
dard: occupational exposure to refractory ceramic
bers. Cincinnati, OH: U.S. Department of Health
and Human Services, Centers for Disease Control
and Prevention, National Institute for Occupa-
tional Safety and Health, DHHS (NIOSH) Publi-
cation No. 2006–123, http://www.cdc.gov/niosh/
docs/2006-123/pdfs/2006-123.pdf. Date accessed:
April 3, 2013.
NIOSH [2008a]. Work-related lung disease surveil-
lance report 2007. Cincinnati, OH: U.S. Depart-
ment of Health and Human Services, Centers for
Disease Control and Prevention, National Institute
for Occupational Safety and Health, Division of
Respiratory Disease Studies, DHHS (NIOSH) Pub-
lication No. 2008-143, http://www.cdc.gov/niosh/
docs/2008-143/. Date accessed: May 15, 2013.
NIOSH [2008b]. Essential elements of eective
workplace programs and policies for improving
worker health and wellbeing. Cincinnati, OH: De-
partment of Health and Human Services, Centers
for Disease Control and Prevention, National In-
stitute for Occupational Safety and Health, DHHS
(NIOSH) Publication No. 2010-140, http://www.
cdc.gov/niosh/docs/2010-140/pdfs/2010-140.pdf.
Date Accessed: March 19, 2014.
NIOSH [2012]. Nicotine: systemic agent. In: emer-
gency response safety and health database (ERSH-
DB), http://www.cdc.gov/niosh/ershdb/Emergen-
cyResponseCard_29750028.html. Date accessed:
May 28, 2014.
NIOSH [2013a]. Criteria for a recommended stan-
dard: occupational exposure to hexavalent chro-
mium. Cincinnati, OH: U.S. Department of Health
and Human Services, Centers for Disease Control
52 53
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
and Prevention, National Institute for Occupa-
tional Safety and Health, DHHS (NIOSH) Publi-
cation No. 2013–128, http://www.cdc.gov/niosh/
docs/2013-128/. Date accessed: April 3, 2013.
NIOSH [2013b]. Total Worker Health™, http://
www.cdc.gov/niosh/TWH/totalhealth.html. Date
accessed July 3, 2013.
NIOSH [2014]. Smoking status and tobacco prod-
uct use. In: Work-related Lung Disease Surveillance
System (eWoRLD), http://www2a.cdc.gov/drds/
WorldReportData/SectionDetails.asp?ArchiveID=
1&SectionTitleID=17. Date accessed: May 6, 2014.
Oerman FJ [2014]. e hazards of e-cigarettes.
ASHRAE Journal: June 2014:38–44, http://www.
nxtbook.com/nxtbooks/ashrae/ashraejour-
nal_201406/index.php?startid=38#/46. Date ac-
cessed: February 5, 2015.
O’Hara P, Gerace TA, Elliott LL [1993]. Eective-
ness of self-help smoking cessation guides for re-
ghters. J Occup Med 35(8):795–799, http://doi.
org/10.1097/00043764-199308000-00016. Date ac-
cessed: January 21, 2013.
Orr MS [2014]. Electronic cigarettes in the USA: a
summary of available toxicology data and sugges-
tions for the future. Tob Control 23:ii18–ii22, http://
doi.org/10.1136/tobaccocontrol-2013-051474.
Date accessed: May 5, 2014.
OSHA [1994]. Indoor air quality; proposed rule.
Fed Regist 59(65):15969−16039, https://www.osha.
gov/pls/oshaweb/owadisp.show_document?p_
table=FEDERAL_REGISTER&p_id=13369. Date
accessed: May 9, 2013.
OSHA [2001]. Notice: withdrawal of proposal. Fed
Regist 66:64946, https://www.osha.gov/pls/oshaweb/
owadisp.show_document?p_table=FEDERAL_
REGISTER&p_id=16954. Date accessed: March 18,
2014.
OSHA [2003]. Letter of February 24, 2003, from R.E.
Fairfax, Director, Directorate of Enforcement Pro-
grams, Occupational Safety and Health Administra-
tion, to Regional Administrators and State Plan
Designees, https://www.osha.gov/pls/oshaweb/owadisp.
show_document?p_table=INTERPRETATIONS&p_
id=24602. Date accessed: March 18, 2014.
OSHA [2013a]. Fatality and catastrophe investiga-
tion summaries, http://www.osha.gov/pls/imis/ac-
cidentsearch.html. Date accessed: April 11, 2013.
OSHA [2013b]. Accident 200994770—Employees
injured on a truck when chemicals ignite, http://
www.osha.gov/pls/imis/accidentsearch.accident_
detail?id=200994770. Date accessed: April 11, 2013.
Pacheco SA, Aguiar F, Ruivo P, Proença MC , Se-
kera M, Penque D, Simões T [2012]. Occupational
exposure to environmental tobacco smoke: a study
in Lisbon restaurants. J Tox Env Health Part A–
Current Issues 75(13−15):857−866, http://doi.or
g/10.1080/15287394.2012.690690. Date accessed:
May 10, 2013.
Pan J, Barbeau EM, Levenstein C, Balbach ED
[2005]. Smoke-free airlines and the role of organized
labor: a case study. Am J Public Health 95(3):398–
404, http://doi.org/10.2105/AJPH.2004.040592.
Date accessed: September 4, 2013.
Phillips JA [2014]. Electronic cigarettes: health
risks and workplace policy. Workplace Health
Saf 62(9):396, http://doi.org/10.3928/21650799-
20140815-01. Date accessed: September 30, 2014.
Regan AK, Promo G, Dube SR, Arrazola R [2013].
Electronic nicotine delivery systems: adult use and
awareness of the ‘e-cigarette’ in the USA. Tob Con-
trol 22(1):19–23, http://doi.org/10.1136/tobacco-
control-2011-050044. Date accessed: July 29, 2013.
Ryan J, Zwerling C, Orav, EJ [1992]. Occupational
risks associated with cigarette smoking: a prospec-
tive study. Am J Pub Health 82(1):29–32, http://
dx.doi.org/10.2105/AJPH.82.1.29. Date accessed:
May 1, 2013.
Sacks JJ, Nelson DE [1994]. Smoking and injuries:
an overview. Prev Med 23:515–520, http://doi.
org/10.1006/pmed.1994.1070. Date accessed: April
11, 2013.
52 53
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Sadeu JC, Hughes CL, Agarwal S, Foster WG
[2010]. Alcohol, drugs, caeine, tobacco, and en-
vironmental contaminant exposure: reproductive
health consequences and clinical implications. Crit
Rev Tox 40(7):633–652, http://doi.org/10.3109/104
08444.2010.493552. Date accessed: May 10, 2013.
Schaller K, Ruppert L, Kahnert S, Bethke C, Nair U,
Pötschke-Langer M [2013]. Electronic cigarettes:
an overview. In: German Cancer Research Center,
ed. Red Series: Tobacco Prevention and Tobacco
Control, Vol. 19, http://www.dkfz.de/en/presse/
download/RS-Vol19-E-Cigarettes-EN.pdf. Date
accessed: May 5, 2014.
Schill AL, Chosewood LC [2013]. e NIOSH To-
tal Worker Health
TM
Program: an overview. J Oc-
cup Environ Med 559(12 Supp):S8–S11, http://
doi.org/10.1097/JOM.0000000000000037. Date ac-
cessed: December 17, 2013.
Schmidt H, Voigt K, Emanuel EJ [2013]. e ethics
of not hiring smokers. N Engl J Med 368:1369−1371,
http://doi.org/10.1056/NEJMp1301951. Date ac-
cessed: July 5, 2013.
Schober W, Szendrei K, Matzen W, Osiander-Fuchs
H, Heitmann D, Schettgen T, Jörres RA, Fromme
H [2014]. Use of electronic cigarettes (e-cigarettes)
impairs indoor air quality and increases FeNO
levels of e-cigarette consumers. Int J Hyg Environ
Health 217(6):628–637, http://doi.org/10.1016/j.
ijheh.2013.11.003. Date accessed: May 5, 2014.
Schraufnagel DE, Blasi F, Drummond MB, Lam
DC, Latif E, Rosen MJ, Sansores R, Van Zyl-Smit R,
on behalf of the Forum of International Respiratory
Societies [2014]. Electronic cigarettes: a position
statement of the Forum of International Respiratory
Societies. Am J Respir Crit Care Med 190(6):611–
618, http://doi.org/10.1164/rccm.201407-1198PP.
Date accessed: July 15, 2014.
Schripp T, Markewitz D, Uhde E, Salthammer T
[2013]. Does e-cigarette consumption cause pas-
sive vaping? Indoor Air 23(1):25−31, http://doi.
org/10.1111/j.1600-0668.2012.00792.x. Date ac-
cessed: July 23, 2013.
Shopland DR, Anderson CM, Burns DM, Gerlach
KK [2004]. Disparities in smoke-free workplace
policies among food service workers. J Occup Envi-
ron Med 46(4):347–356, http://doi.org/10.1097/01.
jom.0000121129.78510.be. Date accessed: Decem-
ber 9, 2013.
Slavit WI [2011]. Fact sheet: what employers need
to know about electronic cigarettes. September. Na-
tional Business Group on Health, http://www.ctri.
wisc.edu/Smokers/ecigs/bgh.pdf. Date accessed:
September 30, 2014.
Soares SR, Melo MA [2008]. Cigarette smok-
ing and reproductive function. Curr Opin Ob-
stet Gynecol 20(3):281–291, http://doi.org/10.1097/
GCO.0b013e3282fc9c1e. Date accessed: May 5, 2013.
Sorensen LT [2012]. Wound healing and in-
fection in surgery: the pathophysiological im-
pact of smoking, smoking cessation, and nico-
tine replacement therapy: a systematic review.
Ann Surg 255:1069−1079, http://doi.org/10.1097/
SLA.0b013e31824f632d. Date accessed: September
17, 2013.
Sorensen G, Stoddard AM, LaMontagne AD, Em-
mons K, Hunt MK, Youngstrom R, McLellan D,
Christiani DC [2003]. A comprehensive worksite
cancer prevention intervention: behavior change
results from a randomized controlled trial (United
States). J Public Health Policy 24(1):5–25, http://
doi.org/10.2307/3343174. Date accessed: July 5,
2013.
Stanbury M, Chester D, Hanna EA, Rosenman
KD [2008]. How many deaths will it take? A death
from asthma associated with work-related environ-
mental tobacco smoke. Am J Ind Med 51:111−116,
http://doi.org/10.1002/ajim.20538. Date accessed:
May 1, 2013.
Stayner L, Bena J, Sasco AJ, Smith R, Steenland K,
Kreuzer M, Straif K [2007]. Lung cancer risk and
workplace exposure to environmental tobacco
smoke. Am J Public Health 97(3):545–551, http://
doi.org/10.2105/AJPH.2004.061275. Date ac-
cessed: December 11, 2013.
54 55
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Stead LF, Hartmann-Boyce J, Perera R, Lancaster
T [2013]. Telephone counselling for smoking ces-
sation. Cochrane Database Syst Rev 8:CD002850,
http://doi.org/10.1002/14651858.CD002850.pub3.
Date accessed: September 17, 2014.
Stellman SD, Boetta P, Garnkel L [1988]. Smoking
habits of 800,000 American men and women in rela-
tion to their occupations. Am J Ind Med 13(1):43−58,
http://doi.org/10.1002/ajim.4700130104. Date ac-
cessed: May 10, 2013.
Stepanov I, Jensen J, Hatsukami D, Hecht SS
[2008]. New and traditional smokeless tobacco:
comparison of toxicant and carcinogen levels.
Nicotine Tob Res 10(12):1773–1782, http://doi.
org/10.1080/14622200802443544. Date accessed:
September 20, 2014.
Sterling TD, Weinkam JJ [1976]. Smoking char-
acteristics by type of employment. J Occup Med
18(11):743−754, http://ovidsp.ovid.com/ovidweb.
cgi?T=JS&MODE=ovid&PAGE=fulltext&D=ovf
t&AN=00005122-197611000-00011&NEWS=n.
Date accessed: May 10, 2013.
Tan CE, Glantz SA [2012]. Association between
smoke-free legislation and hospitalizations for car-
diac, cerebrovascular, and respiratory diseases: a me-
ta-analysis. Circulation 126:2177–2183, http://doi.
org/10.1161/CIRCULATIONAHA.112.121301.
Date accessed: December 10, 2013.
Tao L, Davis R, Heyer N, Yang Q, Qiu W, Zhu L,
Li N, Zhang H, Zeng L, Zhao Y [2013]. Eect of
cigarette smoking on noise-induced hearing loss
in workers exposed to occupational noise in Chi-
na. Noise Health 15:67−72, http://www.noiseand-
health.org/text.asp?2013/15/62/67/107159. Date
accessed: May 10, 2013.
Task Force on Community Preventive Services
[2010]. Recommendations for worksite-based
interventions to improve workers’ health. Am
J Prev Med 38(2 Suppl):S232–S236, http://doi.
org/10.1016/j.amepre.2009.10.033. Date accessed:
September 5, 2013.
omas D, Pogoda J, Langholz B, Mack W [1994].
Temporal modiers of the radon-smoking inter-
action. Health Phys 66(3):257–262, http://doi.
org/10.1097/00004032-199403000-00004. Date ac-
cessed: September 19, 2014.
Toland B [2013]. UPMC smoking ban to include
break time. Pittsburgh Post-Gazette, July 11, http://
www.post-gazette.com/stories/business/news/upmc-
smoking-ban-to-include-break-time-694959/. Date
accessed: September 5, 2013.
Towers Watson/National Business Group on
Health [2011]. e road ahead: shaping health care
strategy in a post-reform environment. 16th An-
nual Towers Watson/National Business Group on
Health Employer Survey on Purchasing Value in
Health Care. Atlanta: Towers Watson, http://www.
thehortongroup.com/Files/41c8e753-70d4-b602-
38db-15481ad7e12d.pdf. Date accessed: Septem-
ber 13, 2013.
Tsikrika S, Vakali S, Gennimata SA, Palamidas A,
Kaltsakas G, Koulouris N, Gratziou C [2014]. Short
term use of an e-cig: inuence on clinical symp-
toms, vital signs and eCO levels [abstract]. Tob
Induc Dis 12(Suppl 1):A30, http://tobaccoinduced-
diseases.com/content/12/S1/A30. Date accessed:
September 22, 2014.
University of Maryland Francis King Carey School
of Law Legal Resource Center [2014]. Maryland
business guide: creating a tobacco free campus. Bal-
timore, MD: University of Maryland Francis King
Carey School of Law, http://www.law.umaryland.
edu/programs/publichealth/documents/smoke-
free_bus_tookit.pdf. Date accessed: September 22,
2014.
U.S. Department of Labor [2014]: FAQs about
Aordable Care Act implementation (Part XIX),
http://www.dol.gov/ebsa/faqs/faq-aca19.html.
Date accessed: May 28, 2014.
Volpp KG, Troxel AB, Pauly MV, Glick HA, Puig
A, Asch DA, Galvin R, Zhu J, Wan F, DeGuz-
man J, Corbett E, Weiner J, Audrain-McGovern J
[2009]. A randomized, controlled trial of nancial
54 55
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
incentives for smoking cessation. N Engl J Med
360(7):699−709, http://doi.org/10.1056/NEJM-
sa0806819. Date accessed: July 5, 2013.
Wagener TL, Siegel M, Borrelli B [2012]. Electronic
cigarettes: achieving a balanced perspective. Addic-
tion 107(9):1545–1548, http://doi.org/10.1111/j.1360-
0443.2012.03826.x. Date accessed: May 5, 2014.
Welch WM [2014]. Vaporizers, e-cigs of the pot world,
are booming. USA Today, March 17, http://www.
usatoday.com/story/money/business/2014/03/15/
marijuana-vaporizer-gains/6042675/. Date ac-
cessed: February 5, 2015.
WHO, World Health Organization Study Group on
Tobacco Product Regulation [2009]. Report on the
scientic basis of tobacco product regulation: third
report of a WHO Study Group. World Health Or-
ganization Technical Report Series no. 955. Gene-
va: World Health Organization, http://whqlibdoc.
who.int/publications/2009/9789241209557_eng.
pdf. Date accessed: May 5, 2014.
WHO, Conference of the Parties to the World
Health Organization Framework Convention on
Tobacco Control [2014]. Electronic nicotine deliv-
ery systems. Provisional agenda item 4.4.2 FCTC/
COP/6/10, July, http://apps.who.int/gb/fctc/PDF/
cop6/FCTC_COP6_10-en.pdf?ua=1. Date ac-
cessed: August 28, 2014.
Whittaker R, McRobbie H, Bullen C, Borland R, Rog-
ers A, Gu Y [2012]. Mobile phone-based interven-
tions for smoking cessation. Cochrane Database Syst
Rev 11:CD006611, http://doi.org/10.1002/14651858.
CD006611.pub3. Date accessed: February 4, 2015.
Wraith D, Mengersen K [2007]. Assessing the
combined eect of asbestos exposure and smok-
ing on lung cancer: a Bayesian approach. Stat Med
26:1150−1169, http://doi.org/10.1002/sim.2602.
Date accessed: May 13, 2013.
Yong LC, Luckhaupt SE, Li J, Calvert GM [2014].
Quit interest, quit attempt and recent cigarette
smoking cessation in the US working population,
2010. Occup Environ Med 71:405–414, http://doi.
org/10.1136/oemed-2013-101852. Date accessed:
February 12, 2014.
Young K, Regan M, Hammer M [2003]. Driver dis-
traction: a review of the literature. Report No. 206.
Victoria, Australia: Monash University Accident
Research Centre, Victoria, Australi, http://www.
monash.edu.au/miri/research/reports/muarc206.
pdf]. Date accessed: January 14, 2014.
Zellers L, omas MA, Ashe M [2007]. Legal risks
to employers who allow smoking in the workplace.
Am J Public Health 97(8):1376–1382, http://doi.
org/10.2105/AJPH.2006.094102. Date accessed:
September 4, 201.Marte aberesto catri ered pra
is page intentionally le blank.

APPENDIX

58 59
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Table A-1. Previous NIOSH Current Intelligence Bulletins on Tobacco Use
Publication (year) Findings Recommendations
Current Intelligence
Bulletin 31
Smoking and the
Occupational
Environment (1979)
Smoking and/or tobacco products dened as cigarettes, cigars,
pipe tobacco, chewing tobacco, and any by-products resulting
from their burning and/or use.
Identied six ways smoking and/or other tobacco use can
interact with workplace exposures to worsen occupational
disease and injury:
1. Certain toxic agents present in some workplaces may also
be present in tobacco smoke, increasing exposure to
those agents.
2. Some workplace chemicals can be transformed into more
harmful agents by smoking—specically by the heat
generated by burning tobacco.
3. Tobacco products can become contaminated with toxic
agents present in the workplace, thus facilitating entry of
the agent into the body by inhalation, ingestion, and/or
skin absorption.
4. Smoking can cause adverse health eects comparable to
those caused by exposure to toxic agents present in some
workplaces, thus causing additive eects.
5. Smoking can act synergistically with toxic agents present
in some workplaces to cause a much more profound eect
than anticipated simply from the separate inuences of the
occupational exposure and smoking.
6. Smoking can contribute to accidents in the workplace.
Use of and/or carrying of tobacco products into the
workplace should be curtailed in situations where employees
may be exposed to physical or chemical substances that may
interact with tobacco products.
Curtailment of the use of tobacco products in the workplace
should be accompanied by simultaneous control of worker
exposure to hazardous physical and chemical agents.
See footnotes at end of table. (Continued)

58 59
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Table A-1. Previous NIOSH Current Intelligence Bulletins on Tobacco Use (Continued)
Publication (year) Findings Recommendations
Current Intelligence
Bulletin 54
Environmental
Tobacco Smoke in
the Workplace: Lung
Cancer and Other
Eects* (1991)
Main conclusion: “NIOSH has determined that the collective
weight of evidence … is sucient to conclude that [SHS]* poses
an increased risk of lung cancer and possibly heart disease to
occupationally exposed workers.”
Conclusions and recommendations based on:
• Reports of Surgeon General on health eects of tobacco
smoke.
• Comparison of chemical compositions of SHS and main-
stream smoke.
• Results from recent epidemiologic studies of nonsmokers
exposed
to SHS.
• Methods for controlling involuntary workplace exposures to
ETS.*
Risk of developing cancer should be decreased by
minimizing exposure to SHS.
Workers should not be involuntarily exposed to tobacco
smoke.
Employers should … assess conditions that may result in
worker exposure to SHS and take steps to reduce exposures
to the lowest feasible concentration.
Best method for controlling worker exposure to SHS is
to eliminate tobacco use from the workplace and begin a
smoking cessation program.
Management and labor should work together to develop
nonsmoking policies:
• Prohibit smoking at the workplace; post signs at workplace
entrances.
• Distribute information about health promotion and harm-
ful eects
of smoking.
• Oer smoking-cessation classes to all workers.
• Establish incentives to encourage workers to stop smoking.
Pending complete elimination of tobacco smoking in the
workplace, smoking should be isolated to clearly posted,
enclosed areas, with separate ventilation exhausted directly
to the outside without recirculation.
*e 1991 document used the term “environmental tobacco smoke” (ETS) to refer to what this CIB calls “secondhand smoke” (SHS).

60 61
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Table A-2. Other NIOSH Publications with Policy Recommendations Relating to Tobacco Use
Year Agent/Process Tobacco-related Recommendation(s) Selected Additional Content
Criteria Documents
1972 Asbestos Smoking cessation (as medical management for
exposed workers who smoke).
1972 Carbon monoxide Medical exams, which could provide “opportunity
to conduct anti-smoking programs for high-risk
employees.”
1973 Inorganic mercury No smoking in designated areas; wash before
smoking.*
1975 Inorganic uorides No smoking in designated areas; wash before
smoking/chewing*; no carrying tobacco products in
contaminated clothing.
1976 Boron triuoride No smoking or uncovered smoking materials in
designated areas.
1976 Cadmium No smoking or carrying uncovered tobacco
products in designated areas.
1976 Carbaryl No smoking in designated areas; wash before
smoking.*
1976 Formaldehyde No smoking in designated areas; wash before
smoking.*
1976 Methyl parathion No smoking or carrying tobacco products in
designated areas; wash before smoking*; post “No
smoking” signs; provide area free of contamination
for storing tobacco products.
1976 Organotin compounds No smoking in designated areas.
1976 Parathion No smoking or carrying tobacco products in
designated areas; wash before smoking*; post “No
smoking” signs; provide area free of contamination
for storing tobacco products.
See footnotes at end of table. (Continued)

60 61
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Year Agent/Process Tobacco-related Recommendation(s) Selected Additional Content
1978 Dinitro-ortho-cresol No smoking in designated areas.
1976 Carbon tetrachloride No smoking in designated areas; wash before
smoking.*
1979 Chloroform No smoking in designated areas; wash before
smoking.*
1988 Welding, brazing, and
thermal cutting
No use or storage of tobacco products in designated
areas; wash before smoking*; counsel smokers
about how smoking may enhance adverse eects of
occupational hazards.
2006 Refractory ceramic
bers
No smoking in workplace; collect smoking histories
as part of the medical monitoring program; counsel
workers who smoke tobacco products about
increased risk of adverse respiratory eects induced
by RCF; disseminate information about health
promotion and the harmful eects of smoking;
establish and oer smoking cessation programs to
workers at no cost; all workers who smoke and are
potentially exposed to RCFs should participate in
smoking cessation program.
Entire sections (1.13and 9.6) devoted to smoking cessation.
NIOSH recognizes a synergistic eect of smoking and
exposure to RCFs, increasing risk of adverse respiratory health
eects induced by RCFs. Interactive eect of tobacco smoking
and exposure to airborne bers previously documented.
RCF-associated decreases in pulmonary function limited to
current and former smokers.
Finding consistent with studies of workers exposed to airborne
contaminants, in which combined smoking and exposures to
various airborne dusts results on increased risk of occupational
respiratory diseases, including chronic bronchitis, emphysema,
and lung cancer.
2013 Hexavalent chromium Prohibit smoking in all areas of any workplaces in
which workers are exposed to Cr(VI) compounds;
as part of a comprehensive safety and health
program, oer a no-cost smoking cessation
program that informs workers about the hazards
of cigarette smoking and provides assistance and
encouragement for workers who want to quit
smoking; all workers who smoke participate.
Entire section (8.7) devoted to smoking cessation
ese elements, in combination with eorts to maintain
airborne Cr(VI) concentrations below the REL and prevent
dermal contact with Cr(VI) compounds, will further protect
the health of workers.
[A]ssociation of skin disease and/or smoking habit with
elevated urinary Cr levels in cement workers.
See footnotes at end of table. (Continued)
Table A-2 (Continued). Other NIOSH Publications with Policy Recommendations Relating to Tobacco Use
62 63
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Year Agent/Process Tobacco-related Recommendation(s) Selected Additional Content
Current Intelligence Bulletins
1978 Tetrachloroethylene
(perchloroethylene)
Workers who handle liquid tetrachloroethylene
should wash hands thoroughly before smoking.
1986 Methylene chloride Smoking should not be permitted in areas where
methylene chloride is manufactured, stored, or
used.
1986 4,4’-methylenedianiline
(MDA)
A smoking cessation program should be provided,
because cigarette smoking is a well-established risk
factor for bladder cancer
2013 Carbon nanotubes and
nanobers
Encourage workers to wash hands before eating,
smoking.
Alerts
1984 Carbon monoxide
hazard in aircra
refueling operations
Workers engaged in fueling operations should
be encouraged to refrain from smoking because
smoking elevates blood levels of carbon monoxide
enough to reduce margin of safety.
1991 Lead poisoning in
construction
No use or carrying of tobacco products in
designated area(s); wash before smoking.*
1992 Silicosis from
sandblasting
No use of tobacco products in blasting area; wash
before smoking.*
1992 Silicosis in rock drillers No use of tobacco products in blasting area; wash
before smoking.*
1996 Asthma from
diisocyanate
Wash before smoking outside work area.
1996 Silicosis in construction No use of tobacco products in dusty areas; wash
before smoking.*
See footnotes at end of table. (Continued)
Table A-2 (Continued). Other NIOSH Publications with Policy Recommendations Relating to Tobacco Use

62 63
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
See footnotes at end of table. (Continued)
Table A-2 (Continued). Other NIOSH Publications with Policy Recommendations Relating to Tobacco Use
Year Agent/Process Tobacco-related Recommendation(s) Selected Additional Content
1999 Phosphine poisoning
and explosions during
fumigation
Wash before smoking.*
2006 Asthma from MDI
exposure during spray-
on truck bed liner and
related applications
Wash before smoking.*
2007 Explosions in industrial
ethylene oxide
sterilization facilities
No smoking where EtO is handled, used, or stored.
2007 Fire ghter fatalities
due to heart attacks
and other sudden
cardiovascular events
Prohibit smoking in all re stations and other re
department facilities; include a smoking cessation
program in any wellness program.
Because not all re stations are smoke-free, involuntary
exposure to tobacco smoke continues to present cardiovascular
risks for re ghters.
Unrecognized sources of carbon monoxide exposure for re
ghters include environmental tobacco smoke; diesel exhaust in
rehouse; diesel exhaust from re engine operating at re scene.
2011 Sensitization and
disease from beryllium
exposure
No storage or use of tobacco products in beryllium
work areas.
Fact Sheets
2003 Asbestos associated
with vermiculite from
Libby, MT
Workers who have been exposed and currently
smoke should quit smoking; employers can assist
them by oering smoking cessation programs.
Workplace Solutions
2007 Handling Micotil 300® No smoking in designated area.
Infosheets
2012 Cleaning chemicals Wash before smoking.*

64 65
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Year Agent/Process Tobacco-related Recommendation(s) Selected Additional Content
Updates
1993 Silicosis deaths No use of tobacco products in designated area; wash
before smoking.*
Proposed National Strategies
1989 Proposed National
Strategy for the
Prevention of
Occupational Lung
Diseases
Management and labor should work together to
develop smoking policies:
• Prohibit smoking at the workplace.
• Distribute information about health promotion
and harmful eects of smoking.
• Oer no-cost smoking-cessation classes to all
workers.
• Establish incentives to encourage workers to stop
smoking.
• Post appropriate signs at workplace entrances.
Smoking is strongly associated with many lung diseases.
Smoking has an additive eect on the risk of chronic bronchitis
in workers exposed to coal mine and other dusts, and it acts
synergistically with asbestos to increase the risk of lung cancer.
Evidence indicates adverse eects on those who are exposed to
the smoke of others.
Because of the overwhelming evidence of the health
consequences from smoking and the number of workers
aected, a focus on smoking is an important component of an
eective prevention strategy.
Elimination of smoking in the workplace is an eective
strategy.
See footnotes at end of table. (Continued)
Table A-2 (Continued). Other NIOSH Publications With Policy Recommendations Relating to Tobacco Use

64 65
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Year Agent/Process Tobacco-related Recommendation(s) Selected Additional Content
1989 Proposed National
Strategy for the
Prevention of
Occupational
Cardiovascular Diseases
Identify groups of workers at high risk of
cardiovascular and other diseases based on
exposure in the workplace and personal risk factors;
to ensure that workers have full and eective
access, implement programs for health promotion
and disease prevention at the worksite whenever
possible or practical; programs should include
eorts to reduce personal, modiable risk factors
for cardiovascular disease, including smoking
In an ideal situation, when occupational factors increase the
risk of cardiovascular disease, both occupational and personal
risks would be addressed at the workplace.
Encouraging workers to quit smoking is particularly important
because smoking contributes not only to several cardiovascular
diseases but to other diseases as well.
Increasing the availability of health promotion programs in the
workplace requires the cooperation of industry, labor unions,
community and voluntary groups, and the government.
Most programs will be conducted in the private sector, but
governmental agencies can play important roles in stimulating
the development of eective programs and in evaluating them.
*“Wash” in this context means wash hands and face.
To access individual documents, see NIOSH Publications and Products website, http://www.cdc.gov/niosh/pubs/default.html. Disclaimer: Table is not necessarily
comprehensive. NOTE: Table does not include NIOSH recommendations focused solely on tobacco use (see Table A-1) or, for example, tobacco-related
recommendations included in agent-specic guidance included in NIOSH/OSHA Occupational Health Guidelines for Chemical Hazards (DHHS NIOSH Publication No.
81-123).
Table A-2 (Continued). Other NIOSH Publications With Policy Recommendations Relating to Tobacco Use
66 67
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Table A-3. OSHA and MSHA Regulations With Provisions Relating to Tobacco Use
Hazard Category and Provisions Agent/Process Industry Regulation CFR
Fire/Explosion
For designated area(s):
• Smoking prohibitions.
and (in most listed regulations)
• ‘No-smoking’ placard requirements.
and (in some listed regulations)
• Program to assure that no smoking
materials are carried.
and (in some listed regulations)
• Smoking history required in
medical surveillance.
Hydrogen
Hydrogen or hydrogen sealing
systems
General Industry
Electric Power Generation, Transmission,
and Distribution
1910.103
1910.269
Oxygen
General Industry
Surface metal/nonmetal mines
Underground metal/nonmetal mines
1910.104
56.7805
57.7805
Flammable liquids General Industry
Shipyards
Marine Terminals Construction
Construction
Surface metal/nonmetal mines
Underground metal/nonmetal mines
1910.106
1915.36
1917.156
1926.152
56.4100
56.4101
57.4100
57.4101
Spray nishing using ammable
and combustible materials
General Industry
Marine Terminals
1910.107
1917.153
Explosives and blasting agents General Industry
Surface metal/nonmetal mines
Underground metal/nonmetal mines
Underground coal mines
1910.109
1926.900
1926.902
1926.904
56.6904
57.6904
75.1702
75.1721
Storage and handling of liqueed
petroleum gases
General Industry 1910.110
See footnotes at end of table. (Continued)

66 67
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
See footnotes at end of table. (Continued)
Hazard Category and Provisions Agent/Process Industry Regulation CFR
Dipping and coating operations
that use ammable liquids or
liquids with ashpoints greater
than 199.4 ˚F (93 ˚C)
General Industry 1910.125
Battery-charging/changing areas General Industry
Surface metal/nonmetal mines
Underground metal/nonmetal mines
Marine Terminals
Longshoring
1910.178
56.4502
57.4502
1917.157
1918.1
Grain handling facilities General Industry 1910.272
Permit-required Conned Spaces General Industry 1910.146
Underground lines Power Transmission and Distribution 1926.956
Benzene General Industry
Shipyards
Construction
1910.1028
1915.1028
1926.1128
Acrylonitrile General Industry
Construction
1910.1045
1926.1145
Ethylene oxide General Industry
Construction
1910.1047
1926.1147
Formaldehyde General Industry
Shipyards
Construction
1910.1048
1915.1048
1926.1148
Gassy operations Underground Construction Caissons, Coerdams,
and Compressed Air
Underground metal/nonmetal mines
1926.800
57.22102
57.22105
Table A-3. OSHA and MSHA Regulations With Provisions Relating to Tobacco Use (Continued)

68 69
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Hazard Category and Provisions Agent/Process Industry Regulation CFR
General Fire Prevention Construction
Underground metal/nonmetal mines
Underground coal mines
1926.151
57.4100
57.4101
57.6904
57.7805
57.22101
57.22102
77.1102
77.1711
Record-keeping areas Underground metal/nonmetal mines 57.5041
Ingestion/absorption of toxic agent
For designated area(s):
• Prohibitions on smoking, storage of
smoking materials, tobacco prod-
ucts (including chewing tobacco),
and chewing of such products.
and
• Requirements for washing prior to
smoking/eating.
and (in most listed regulations)
• Requirements to post
“No-smoking” placards.
Asbestos General Industry
Shipyards
Construction
1910.1001
1915.1001
1926.1101
13 specied carcinogens
(4-Nitrobiphenyl, etc.)
General Industry
Shipyards
Construction
1910.1003
1915.1003
1926.1103
Inorganic arsenic General Industry
Shipyards
Construction
1910.1018
1915.1018
1926.1118
Lead General Industry
Shipyards
Construction
1910.1025
1915.1025
1926.62
Table A-3. OSHA and MSHA Regulations With Provisions Relating to Tobacco Use (Continued)
See footnotes at end of table. (Continued)

68 69
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Hazard Category and Provisions Agent/Process Industry Regulation CFR
Chromium (VI) General Industry
Shipyards
Longshoring
Construction
1910.1026
1915.1026
1918.1
1926.1126
Cadmium General Industry
Shipyards
Construction
Agriculture
1910.1027
1915.1027
1926.1127
1928.1027
Benzene General Industry
Shipyards
Construction
1910.1028
1915.1028
1926.1128
Coke oven emissions General Industry
Construction
1910.1029
1926.1129
Bloodborne pathogens General Industry
Shipyards
1910.1030
1915.1030
1,2-dibromo-3-chloropropane General Industry
Shipyards
Construction
1910.1044
1915.1044
1926.1144
Acrylonitrile General Industry
Construction
1910.1045
1926.1145
Ethylene oxide General Industry
Construction
1910.1047
1926.1147
Ethylene oxide General Industry
Shipyards
1910.1047
1915.1047
Formaldehyde General Industry
Shipyards
Construction
1910.1048
1915.1048
1926.1148
Table A-3. OSHA and MSHA Regulations With Provisions Relating to Tobacco Use (Continued)
See footnotes at end of table. (Continued)

70 71
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Hazard Category and Provisions Agent/Process Industry Regulation CFR
Methylenedianiline General Industry
Shipyards
Construction
1910.1050
1915.1050
1926.60
1,3-Butadiene General Industry 1910.1051
Methylene chloride General Industry
Shipyards
Construction
1910.1052
1915.1052
1926.1152
Hazardous chemicals in
laboratories
General Industry
Shipyards
1910.1450
1915.1450
General/Field Sanitation Shipyards
Agriculture
1915.88
1928.110
Misc.
• Personal Protective Equipment
Standard: requires a 15-minute
no-smoking period prior to Bitrex
t-testing of respirators.
• Cotton Dust Standard: required
medical questionnaire asks about
smoking.
• Hazard Communication Standard:
Appendices invoke smoking history
in the assessment of evidence used
to categorize substances as respira-
tory sensitizers, and detail require-
ments for “No smoking” warning
labels.
Personal Protective Equipment General Industry
Shipyards
Marine Terminals
Longshoring
Construction
1910.134
1915.154
1917.92
1918.102
1926.103
Cotton Dust General Industry 1910.1043
Hazard Communication General Industry
Shipyards
Construction
1910.1200
1915.1200
1926.59
Specic requirements of OSHA and MSHA regulations should be determined by directly consulting those regulations. Disclaimer: Table is not necessarily comprehensive
and is not intended to be used for compliance purposes. NOTE: Table does not include OSHA regulations that require retention of Department of Transportation
markings, placards, and labels relating to ammability/explosivity (e.g., 1910.1201, 1915.88, 1917.29, 1926.61). Nor does it include OSHA “model standards” for
carcinogens (1990.151; 1990.152), which include a provision prohibiting smoking/chewing/tobacco.
Table A-3. OSHA and MSHA Regulations With Provisions Relating to Tobacco Use (Continued)

70 71
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Figure A-1a. Cigarette smoking among working adults, by industry—United States, 2004–2010

72 73
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Figure A-1b. Cigarette smoking among working adults, by occupation—United States, 2004–2010

72 73
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Figure A-2a. Smokeless tobacco use among working adults, by industry—United States, 2010

74 75
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Figure A-2b. Smokeless tobacco use among working adults, by occupation—United States, 2010

74 75
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Figure A-3a. Dual use of tobacco: Proportion of cigarette smokers who also use smokeless tobacco
among working adults, by industry—United States, 2010
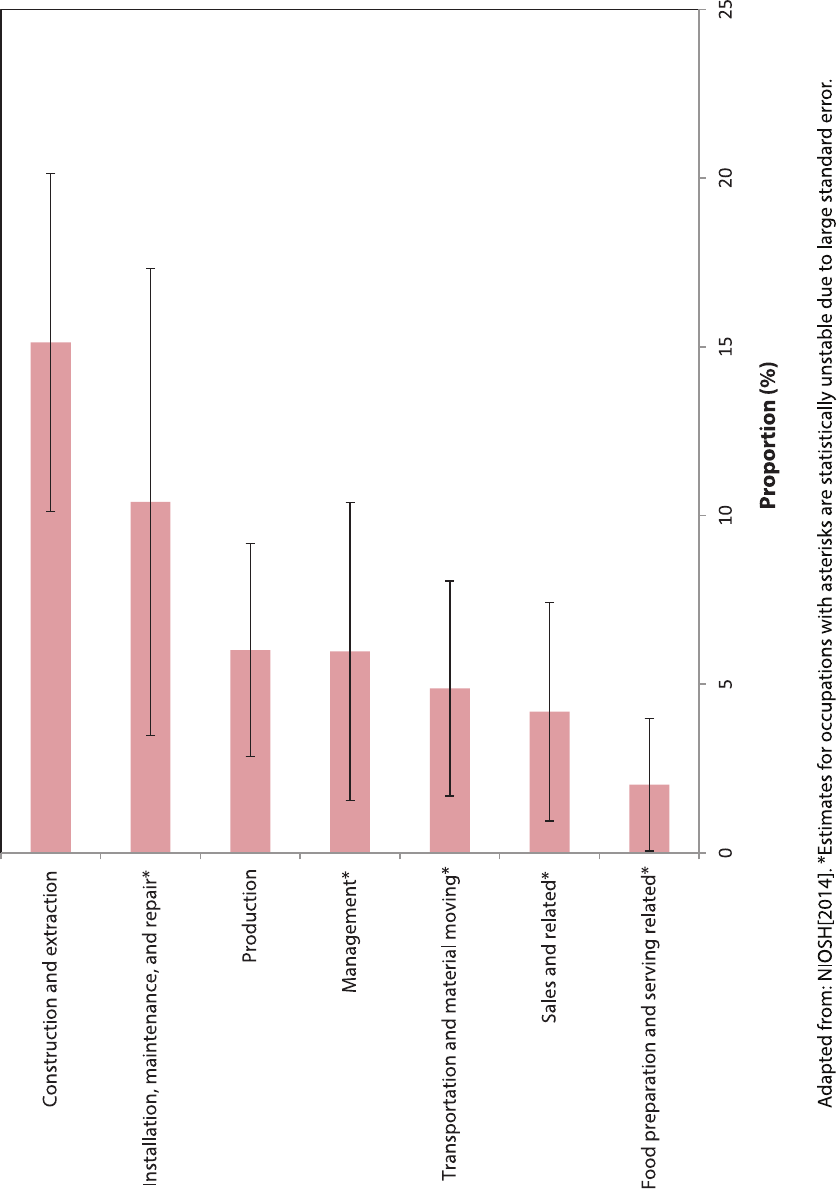
76 77
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Figure A-3b. Dual use of tobacco: Proportion of cigarette smokers who also use smokeless tobacco
among working adults, by occupation—United States, 2010
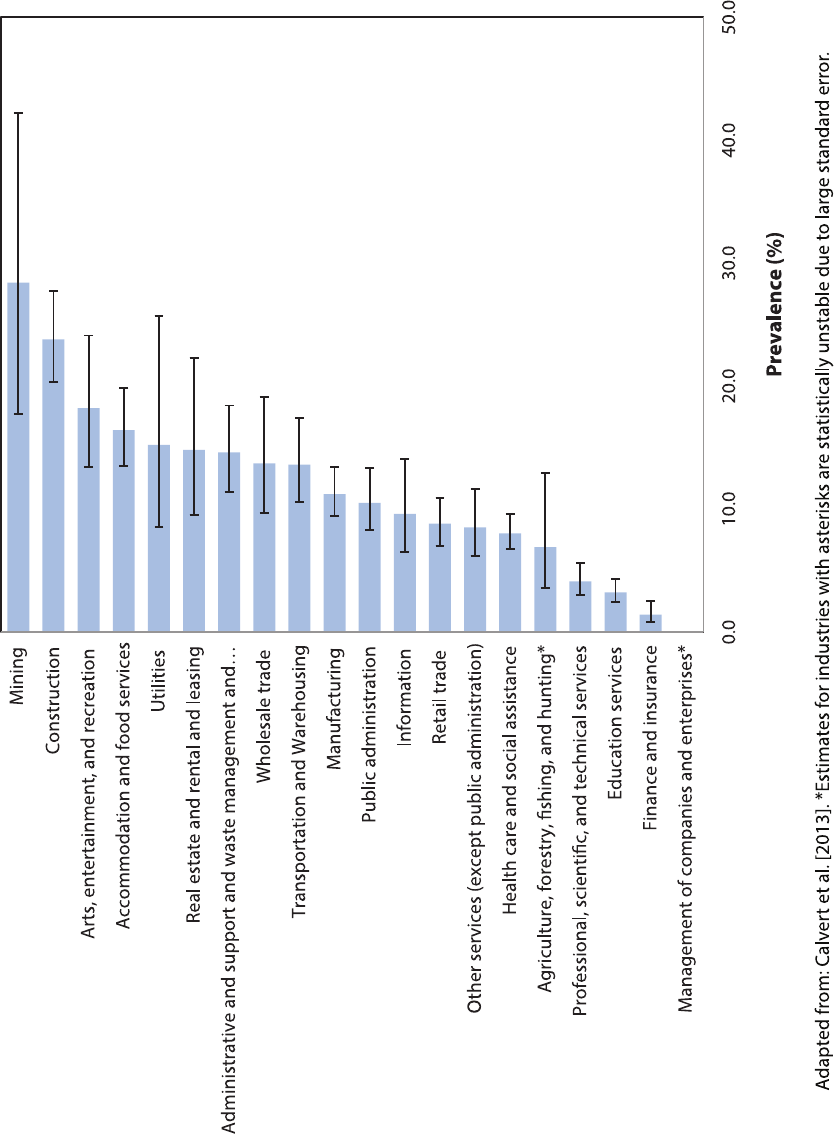
76 77
NIOSH CIB 67
•
Workplace Tobacco Policies NIOSH CIB 67
•
Workplace Tobacco Policies
Figure A-4a. Prevalence of frequent exposure to SHS at work among nonsmoking adults
who worked in the past 12 months, by industry—United States, 2010

78
NIOSH CIB 67
•
Workplace Tobacco Policies
Figure A-4b. Prevalence of frequent exposure to SHS at work among nonsmoking adults
who worked in the past 12 months, by occupation—United States, 2010
is page intentionally le blank.

To receive NIOSH documents or more information about
occupational safety and health topics, contact NIOSH at
1–800–CDC–INFO (1–800–232–4636)
TTY: 1–888–232–6348
CDC -INFO: www.cdc.gov/info
or visit the NIOSH Website at www.cdc.gov/niosh.
For a monthly update on news at NIOSH, subscribe to
NIOSH eNews by visiting www.cdc.gov/niosh/eNews.
DHHS (NIOSH) Publication No. 2015–113
safer • healthier • people
tm
Delivering on the Nation’s promise:
safety and health at work for all people
through research and prevention
