IN THE UNITED STATES DISTRICT COURT
FOR THE SOUTHERN DISTRICT OF TEXAS, CORPUS CHRISTI DIVISION
DIAGNOSTIC AFFILIATES OF §
NORTHEAST HOU, LLC D/B/A § CIVIL ACTION NUMBER
24 HOUR COVIDRT-PCR §
LABORATORY §
§ _______________________
vs. §
§
UNITED HEALTH GROUP, INC.; §
UNITED HEALTHCARE SERVICES, §
INC.; §
UNITED HEALTHCARE BENEFITS §
OF TEXAS, INC.; §
UNITED HEALTHCARE OF TEXAS, §
INC.; §
UMR, INC.; §
OPTUMHEALTH CARE SOLUTIONS, §
INC.; §
AMERICAN INTERNATIONAL §
GROUP, INC. MEDICAL PLAN; §
ANADARKO PETROLEUM CORP. §
HEALTH BENEFIT PLAN; §
APPLE INC. HEALTH AND WELFARE §
BENEFIT PLAN; §
GROUP HEALTH AND WELFARE §
PLANS(ARAMARK UNIFROM SERVICES); §
AT&T UMBRELLA BENEFIT §
PLAN NO. 1; §
AT&T UMBRELLA BENEFIT §
PLAN NO. 3; §
BAKER HUGHES, A GE COMPANY §
WELFARE BENEFITS PLAN; §
BAYLOR COLLEGE OF MEDICINE §
HEALTH AND WELFARE BENEFITS §
PLAN; §
BROOKDALE SENIOR LIVING, INC. §
WELFARE PLAN; §
C.H ROBINSON COMPANY GROUP §
HEALTH MAJOR MEDICAL PLAN; §
CALPINE CORPORATION §
EMPLOYEE BENEFIT PLAN; §
CATERPILLAR INC. GROUP §
INSURANCE MASTER TRUST; §
2:21-cv-131
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 1 of 89

Page 2 of 89
CELANESE HEALTH AND WELFARE §
BENEFITS PROGRAM; §
CENTERPOINT ENERGY GROUP §
WELFARE BENEFITS PLAN FOR §
RETIREES; §
CITGO PETROLEUM CORPORATION §
DEFINED CONTRIBUTION §
MASTER TRUST; §
DELTA ACCOUNT BASED §
HEALTHCARE PLAN; §
ENVISION HEALTHCARE §
CORPORATION WELFARE §
BENEFITS PLAN; §
H&E EQUIPMENT SERVICES INC. §
BENEFIT PLAN; §
FLOUR EMPLOYEE BENEFIT §
TRUST PLAN; §
FRESENIUS MEDICAL CARE §
TRAVELLING NURSES HEALTH AND §
WELFARE BENEFITS PLAN; §
GEICO CORP. CONSOLIDATED §
WELFARE BENEFITS PROGRAM; §
GEOSPACE TECHNOLOGIES §
WELFARE BENEFIT PLAN; §
HUDSON GROUP (HG) INC. §
EMPLOYEE BENEFITS PLAN; §
IQOR HEALTH AND §
WELFARE PLAN; §
JONES LANG LASALLE GROUP §
BENEFITS PLAN; §
KELLOGG BROWN & ROOT, INC, §
WELFARE BENEFITS PLAN; §
KINDER MORGAN, INC. MASTER §
EMPLOYEE WELFARE PLAN; §
LEXICON PHARMACEUTICALS INC. §
COMPREHENSIVE WELFARE §
BENEFITS PLAN; §
LINEAGE LOGISTICS LLC §
BENEFITS PLAN; §
LOCKTON, INC. WELFARE §
BENEFITS PLAN; §
M/I HOMES, INC. HEALTH, LIFE AND §
DENTAL WELFARE PLAN; §
MAERSK INC. ACTIVE NONUNION §
HEALTH AND WELFARE PLAN; §
THE MALLINCKRODT §
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 2 of 89
Page 3 of 89
PHARMACEUTICALS WELFARE §
BENEFIT PLAN; §
MOTIVA ENTERPRISES LLC §
HEALTHAND WELLNESS BENEFIT §
PLAN; §
NOVO NORDISK INC. WELFARE §
BENEFIT PLAN; §
PETSMART SMARTCHOICES §
BENEFIT PLAN; §
PROCTER AND GAMBLE RETIREE §
WELFARE BENEFITS PLAN; §
RAILROAD EMPLOYEES NATIONAL §
HEALTH FLEXIBLE SPENDING §
ACCOUNT PLAN; §
RAISING CANES USA HEALTH AND §
WELFARE BENEFITS WRAP PLAN; §
REPUBLIC SERVICES INC. §
EMPLOYEE BENEFIT PLAN; §
REPUBLIC NATIONAL DISTRIBUTING §
COMPANY, LLC WELFARE §
BENEFITS PLAN; §
SAIA MOTOR FREIGHT LINE LLC §
EMPLOYEE PREFERRED §
PROVIDER PLAN; §
SIEMENS CORPORATION GROUP §
INSURANCE AND FLEXIBLE §
BENEFITS PROGRAM; §
SKADDEN, ARPS, SLATE, MEAGHER §
& FLOM PARTNERS’ WELFARE §
BENEFITS PLAN; §
SKYWEST INC. CAFETERIA PLAN; §
SOUTHWEST AIRLINES CO. §
WELFARE BENEFIT PLAN; §
SPIRIT AIRLINES INC. HEALTH §
AND WELFARE BENEFITS PLAN; §
SWISSPORT NORTH AMERICA §
HOLDINGS, INC. HEALTH & §
WELFARE PLAN; §
TARGA RESOURCES LLC WELFARE §
BENEFITS PLAN; §
TEXAS CAPITAL BANCSHARES §
INC. EMPLOYEE BENEFIT PLAN; §
TEXTRON NON-BARGAINED §
WELFARE BENEFITS PLAN; §
ADECCO, INC WELFARE §
BENEFITS PLAN; §
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 3 of 89
Page 4 of 89
T-MOBILE USA, INC. EMPLOYEE §
BENEFIT PLAN; §
TRANSOCEAN GROUP WELFARE §
BENEFIT PLAN; §
UHS WELFARE BENEFITS PLAN; §
UNITEDHEALTH GROUP §
VENTURES, LLC HEALTH AND §
WELFARE BENEFIT PLAN; §
VALERO ENERGY CORPORATION §
RETIREE BENEFITS PLAN; §
VALMONT INDUSTRIES INC. §
WELFARE BENEFIT PLAN; §
WALGREENS HEALTH AND §
WELFARE PLAN; §
WCA MANAGEMENT COMPANY, §
LP WELFARE BENEFIT PLAN; §
WEBBER, LLC WELFARE §
BENEFIT PLAN; §
WINSTEAD PC FLEXIBLE §
BENEFIT PLAN; §
GROUP BENEFITS PLAN FOR §
EMPLOYEES OF WORLEYPARSONS §
CORPORATION §
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 4 of 89

Page 5 of 89
ORIGINAL COMPLAINT AND JURY DEMAND
Plaintiff Diagnostic Affiliates of Northeast Hou, LLC d/b/a 24 Hour Covid RT-PCR
Laboratory (“24 Hour Covid” or “Plaintiff”), by and through its attorneys, bring its Original
Complaint against United
1
and the Employer Plans
2
, and allege as follows:
INTRODUCTION
1. Plaintiff brings this action against United and the Employer Plans that United
administers because United has unjustifiably engaged in unconscionable and fraudulent conduct
during the COVID-19 public health emergency period in order to evade and circumvent its
obligations to fully cover all United Plan and Employer Plan members’ COVID-19 diagnostic
1
“United” refers to United Health Group, Inc., United Healthcare Services, Inc., United Healthcare Benefits of Texas,
Inc., United Healthcare of Texas, Inc., UMR, Inc., United Healthcare Services, Inc., OptumHealth Care Solutions,
Inc.
2
“Employer Plans” refer to American International Group, Inc. Medical Plan; Anadarko Petroleum Corp. Health
Benefit Plan; Apple Inc. Health And Welfare Benefit Plan; Group Health And Welfare Plans (Aramark Uniform
Services); AT&T Umbrella Benefit Plan No. 1; AT&T Umbrella Benefit Plan No. 3; Baker Hughes, A GE Company
Welfare Benefits Plan; Baylor College Of Medicine Health And Welfare Benefits Plan; Brookdale Senior Living, Inc.
Welfare Plan; C.H Robinson Company Group Health Major Medical Plan; Calpine Corporation Employee Benefit
Plan; Caterpillar Inc. Group Insurance Master Trust; Celanese Health And Welfare Benefits Program; Centerpoint
Energy Group Welfare Benefits Plan For Retirees; Citgo Petroleum Corporation Defined Contribution Master Trust;
Delta Account Based Healthcare Plan; Envision Healthcare Corporation Welfare Benefits Plan; H&E Equipment
Services Inc. Benefit Plan; Flour Employee Benefit Trust Plan; Fresenius Medical Care Travelling Nurses Health And
Welfare Benefits Plan; Geico Corp. Consolidated Welfare Benefits Program; Geospace Technologies Welfare Benefit
Plan; Hudson Group (HG) Inc. Employee Benefits Plan; IQOR Health And Welfare Plan; Jones Lang Lasalle Group
Benefits Plan; Kellogg Brown & Root, Inc, Welfare Benefits Plan; Kinder Morgan, Inc. Master Employee Welfare
Plan; Lexicon Pharmaceuticals Inc. Comprehensive Welfare Benefits Plan; Lineage Logistics LLC Benefits Plan;
Lockton, Inc. Welfare Benefits Plan; M/I Homes, Inc. Health, Life And Dental Welfare Plan; Maersk Inc. Active
Nonunion Health And Welfare Plan; The Mallinckrodt Pharmaceuticals Welfare Benefit Plan; Motiva Enterprises
LLC Health and Wellness Benefit Plan; Novo Nordisk Inc. Welfare Benefit Plan Petsmart Smartchoices Benefit Plan;
Procter And Gamble Retiree Welfare Benefits Plan; Railroad Employees National Health Flexible Spending Account
Plan; Raising Canes USA Health And Welfare Benefits Wrap Plan; Republic Services Inc. Employee Benefit Plan;
Republic National Distributing Company, LLC Welfare Benefits Plan; Saia Motor Freight Line LLC Employee
Preferred Provider Plan; Siemens Corporation Group Insurance And Flexible Benefits Program; Skadden, Arps, Slate,
Meagher & Flom Partners’ Welfare Benefits Plan; Skywest Inc. Cafeteria Plan; Southwest Airlines Co. Welfare
Benefit Plan; Spirit Airlines Inc. Health And Welfare Benefits Plan; Swissport North America Holdings, Inc. Health
& Welfare Plan; Targa Resources LLC Welfare Benefits Plan; Texas Capital Bancshares Inc. Employee Benefit Plan;
Textron Non-Bargained Welfare Benefits Plan; Adecco, Inc Welfare Benefits Plan; T-Mobile USA, Inc. Employee
Benefit Plan; Transocean Group Welfare Benefit Plan; UHS Welfare Benefits Plan; UnitedHealth Group Ventures,
LLC Health And Welfare Benefit Plan; Valero Energy Corporation Retiree Benefits Plan; Valmont Industries Inc.
Welfare Benefit Plan; Walgreens Health And Welfare Plan; WCA Management Company, LP Welfare Benefit Plan;
Webber, LLC Welfare Benefit Plan; Winstead PC Flexible Benefit Plan; Group Benefits Plan For Employees Of
Worleyparsons Corporation.
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 5 of 89
Page 6 of 89
testing (“Covid Testing”) services and to reimburse Plaintiff, an out-of-network (“OON”)
laboratory, for bona fide Covid Testing services offered to these same members in accordance with
a Congressionally set methodology established and supported by the Families First Coronavirus
Response Act (the “FFCRA”), the Coronavirus Aid, Relief, Economic Security Act (the “CARES
Act”), Texas Department of Insurance Commissioner’s Bulletin B-0017-20, and other Federal and
Texas authorities and guidance.
2. The importance of Covid Testing during a worldwide pandemic cannot be
overlooked as it is the best mitigation mechanism in place to identify and curtail the spread of the
COVID-19 virus. Due to the urgent need to facilitate the nation’s response to the public health
emergency posed by COVID-19, Congress passed the FFCRA and the CARES Act to, amongst
other things, address issues pertaining to the costs of and access to Covid Testing during the
COVID-19 pandemic.
3. United and the Employer Plans’ conduct (or lack thereof as it pertains to the
Employer Plans) has undermined national efforts made to mitigate the spread of the COVID-19
virus as it has caused Plaintiff, and other similarly situated OON providers, to shutter specimen
collection and testing locations and to potentially stop offering Covid Testing services altogether.
United’s misprocessing and denials of Covid Testing claims is nearing an insurmountable financial
loss for Plaintiff and has caused Plaintiff to hemorrhage its own funds to cover such financial
losses.
4. United has not only mis-adjudicated almost every single Covid Testing claim
submitted by Plaintiff on behalf of members of United Plans and Employer Plans administered by
United, but has, in fact, denied the vast majority of Covid Testing claims that Plaintiff has
submitted, the reasons for which are to be detailed throughout the course of this Original
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 6 of 89
Page 7 of 89
Complaint.
5. United’s fraudulent behavior, in its capacity as an insurer and third-party claims
administrator, and the Employer Plans’ failures to oversee and regulate United’s behavior (despite
being provided with notice and an opportunity to remedy United’s behavior) has had a material
adverse effect on the nation’s response to the COVID-19 pandemic as it has largely diminished
access to testing, shifted financial responsibility for the cost of Covid Testing to the members of
United Plans and Employer Plans, and, in the event of any future pandemics requiring the
cooperation and the joint efforts of licensed medical facilities and professionals (e.g. Plaintiff),
providers who have fallen victim to United’s predatory practices will be hesitant and less likely to
participate in any such future Federal and/or State efforts, in turn, jeopardizing any future
pandemic responses.
6. Plaintiff has incessantly attempted to contact United to inform it of its unlawful
practices, has attempted to negotiate an agreed amount/rate to be reimbursed for Covid Testing
services with United, and has provided notice to all Employer Plans of United’s unlawful practices.
However, all attempts by Plaintiff to amicably resolve this matter have failed, and Plaintiff is now
left with no other option than to file this lawsuit against all Defendants.
7. By way of this lawsuit, Plaintiff seeks to: (i) hold United accountable for its
fraudulent and unlawful practices, and Employer Plans responsible for their failures to monitor
and check United on its practices despite being provided with notice of such misconduct; (ii)
ensure Plaintiff is properly reimbursed for its efforts to provide a public service in response to the
COVID-19 public health emergency; and (iii) act as a safeguard against future unlawful practices
instituted by United, Employer Plans, and other insurers and health plans in the event of other
national public health emergencies.
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 7 of 89

Page 8 of 89
NATURE OF THE CLAIMS
8. Plaintiff is a CLIA certified high complexity laboratory that has requested
emergency use authorization under Section 564 of the Federal Food, Drug, and Cosmetic Act;
therefore, has all authorizations and/or approvals necessary to render and be reimbursed for Covid
Testing services.
3
At the height of the pandemic Plaintiff operated seven specimen collection sites
located across the States of Texas and Louisiana, and partnered with employers and independent
school districts across Texas to render Covid Testing services to employees, teachers, students,
and other staff members.
4
9. United provides health insurance and/or benefits to members of United Plans
pursuant to a variety of health benefit plans and policies of insurance, including employer-
sponsored benefit plans and individual health benefit plans.
10. United also serves in the trusted role of third-party claims administrator for self-
funded health plans, including the Employer Plans that are named as Defendants in this Original
Complaint.
11. Under ordinary circumstances, not all health plans insured or administered by
United offer its members with access to OON providers and facilities. However, pursuant to
Section 6001 of the FFCRA, as amended by Section 3201 of the CARES Act, all group health
plans and health insurance issuers offering group or individual health insurance coverage are
required to provide benefits for certain items and services related to diagnostic testing for the
detection or diagnosis of COVID-19 without the imposition of cost-sharing, prior authorization,
3
See 21 U.S.C. § 360bbb–3.
4
Humble ISD Expands Options for Student Covid Testing (https://www humbleisd net/covid19studenttesting);
Humble ISD expands free COVID-19 testing options to provide easier access for students
(https://communityimpact.com/houston/lake-houston-humble-kingwood/education/2021/01/07/humble-isd-expands-
free-covid-19-testing-options-to-provide-easier-access-for-students/).
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 8 of 89

Page 9 of 89
or other medical management requirements when such items or services are furnished on or after
March 18, 2020, for the duration of the COVID-19 public health emergency regardless of whether
the Covid Testing provider is an in-network or OON provider.
5
12. Furthermore, Section 3202(a) of the CARES Act provides that all group health
plans and health insurance issuers covering Covid Testing items and services, as described in
Section 6001 of the FFCRA must reimburse OON providers in an amount that equals the cash
price for such Covid Testing services as listed by the OON provider on its public internet website
or to negotiate a rate/amount to be paid that is less than the publicized cash price.
13. United has intentionally disregarded its obligations to comply with its requirements
to cover Covid Testing services without the imposition of cost-sharing and other medical
management requirements pursuant to Section 6001 of the FFCRA and, in the instances Plaintiff
is reimbursed for its Covid Testing services, has failed to reimburse Plaintiff in accordance with
Section 3202(a) of the CARES Act. These violations are made to financially benefit United and,
by acting in its own self-interests, has also caused the Employer Plans to be in violation of the
FFCRA, the CARES Act, Employee Retirement Income Security Act of 1974 (“ERISA”)
6
, and
applicable State law.
14. United has set up complex processes and procedures: (i) to deny or underpay claims
for arbitrary reasons; (ii) to force Plaintiff into a paperwork war of attrition in hopes of wearing
down Plaintiff to the point of collapse through continuous inundation of Plaintiff’s financial and
operational resources; (iii) that have turned United’s internal administrative appeals procedures
into a kangaroo court where facts and law have no relevance, thus, rendering the administrative
appeals process functionally meritless; (iv) to disinform its members, the Employer Plans and other
5
See CMS FAQ Parts 42, 43, and 44, The FFCRA and the CARES Act.
6
29 U.S.C. § 1001 et seq.
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 9 of 89

Page 10 of 89
self-funded health plans that it administers, Plaintiff and other similarly situated OON providers,
the general public, and Federal and State regulators of its obligations to adjudicate Covid Testing
claims in accordance with the FFCRA and the CARES Act; and (v) to ultimately engage in
unscrupulous and fraudulent conduct for its own financial benefit during this public health
emergency.
15. United’s schemes and misconduct also violate the Racketeer Influenced and
Corrupt Organizations Act, 18 U.S.C. §§ 1961-1968 (“RICO”). United has engaged in a pattern of
racketeering activity that includes, but may not be limited to, the embezzlement and/or conversion
of welfare funds and the repeated and continuous use of mails and wires in the furtherance of
multiple schemes to defraud as detailed through this Original Complaint.
16. Furthermore, because Employer Plans have contracted with United to act as their
third-party claims administrator, the Employer Plans, through their silence and inaction, are dually
liable for United’s violations of the FFCRA, the CARES Act, and ERISA pursuant to 29 U.S.C.
§ 1105(a).
PARTIES
17. Plaintiff Diagnostic Affiliates of Northeast Hou, LLC d/b/a 24 Hour Covid RT-
PCR Laboratory is a limited liability company organized under the laws of the State of Texas, with
its company headquarters located at 22751 Professional Drive, Kingwood, Texas 77339. Plaintiff
has lawful standing to bring in all claims asserted herein.
18. Defendant UnitedHealth Group, Inc. is a publicly traded Delaware corporation with
its principal place of business in Minneapolis, Minnesota. It issues health insurance and
administers group health plans nationally through its various wholly-owned and controlled
subsidiaries, including but not limited to United Healthcare Services, Inc. UnitedHealth Group,
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 10 of 89
Page 11 of 89
Inc. may be served with process by serving its registered agent for service The Corporation Trust
Company, 1209 Orange Street, Wilmington, Delaware 19801.
19. Defendant United Healthcare Services, Inc. is a corporation organized under the
laws of the State of Minnesota, with its principal place of business in Minnetonka, Minnesota. It
is a foreign for-profit corporation operating in the State of Texas, and it issues health insurance
and administers plans that are funded by plan sponsors in Texas. It is a wholly-owned subsidiary
of UnitedHealth Group, Inc. United Healthcare Services, Inc. may be served with process by
serving its registered agent for service CT Corporation System, 1010 Dale Street N, St. Paul,
Minnesota, 55117-5603.
20. Defendant United Healthcare Benefits of Texas, Inc. is a corporation organized
under the laws of the State of Texas, with its principal place of business in Austin, Texas. It is a
for-profit corporation operating in the State of Texas, and its issues health insurance and
administers plans that are funded by plan sponsors in Texas. It is a wholly-owned subsidiary of
UnitedHealth Group, Inc. United Healthcare Benefits of Texas, Inc. may be served with process
by serving its registered agent for service CT Corporation System, 350 North St. Paul Street, Dallas
Texas 75201.
21. Defendant UnitedHealthcare of Texas, Inc. is a corporation organized under the
laws of the State of Texas, with its principal place of business in Austin, Texas. It is a for-profit
corporation operating in the State of Texas, and its issues health insurance and administers plans
that are funded by plan sponsors in Texas. It is a wholly-owned subsidiary of UnitedHealth Group,
Inc. UnitedHealthcare of Texas, Inc. may be served with process by serving its registered agent
for service CT Corporation System, 350 North St. Paul Street, Dallas Texas 75201.
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 11 of 89
Page 12 of 89
22. Defendant UMR, Inc. is a corporation organized under the laws of the State of
Wisconsin, with its principal place of business in Wausau, Wisconsin. It is a foreign for-profit
corporation operating in the State of Texas and administers plans that are funded by plan sponsors
in Texas. It is a wholly-owned subsidiary of UnitedHealth Group, Inc. UMR, Inc. may be served
with process by serving its registered agent for service Commissioner of Insurance, 333 Guadalupe
Street, Austin, Texas 78701.
24. Defendant OptumHealth Care Solutions, Inc. is a corporation organized under the
laws of the State of Minnesota, with its principal place of business in Eden Prairie, Minnesota. It
is a foreign for-profit corporation operating in the State of Texas and administers plans that are
funded by plan sponsors in Texas. It is a wholly-owned subsidiary of UnitedHealth Group, Inc.
OptumHealth Care Solutions, Inc. may be served with process by serving its registered agent for
service Commissioner of Insurance, 333 Guadalupe Street, Austin, Texas 78701.
25. Defendant American International Group, Inc. Medical Plan (the “AIG Plan”) is
a self-funded health plan subject to ERISA. The AIG Plan may be served with process by serving
its Plan Administrator, Justin Orlando and/or Megan Moran, at 175 Water Street, 21
st
Floor, New
York, New York 10038.
26. Defendant Anadarko Petroleum Corp. Health Benefits Plan (the “Anadarko” Plan)
is a self-funded health plan subject to ERISA. The Anadarko Plan may be served with process by
serving its Plan Administrator, Madeline N. Pfahler, at Human Resources Department 5 Greenway
Plaza, Suite 110 Houston, TX 77046-0521.
27. Defendant Apple Inc. Health and Welfare Benefit Plan (the “Apple Plan”) is a self-
funded health plan subject to ERISA. The Apple Plan may be served with process by serving its
Plan Administrator, Grace Gippetti Munson, at One Apple Park Way Cupertino, CA 95014.
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 12 of 89
Page 13 of 89
28. Defendant Group Health and Welfare Plans (Aramark Unifrom Services) (the
“Aramark plan”) is a self-funded health plan subject to ERISA. The Aramark Plan may be served
with process by serving its Plan Administrator, Cheryl Heimer, at 115 N First St Burbank, CA
91502-1856.
29. Defendant AT&T Umbrella Benefit Plan No. 1 (the “AT&T No. 1 Plan”) is a self-
funded health plan subject to ERISA. The AT&T Plan may be served with process by serving its
Plan Administrator, Paul W. Stephens, at Po Box 132160 Dallas, TX 75313-2160.
30. Defendant AT&T Umbrella Benefit Plan No. 3 (the “AT&T No. 3 Plan”) is a self-
funded health plan subject to ERISA. The AT&T Plan may be served with process by serving its
Plan Administrator, Paul W. Stephens, at Po Box 132160 Dallas, TX 75313-2160.
31. Defendant Baker Hughes, A GE Company Welfare Benefits Plan (the “Baker
Hughes Plan”) is a self-funded health plan subject to ERISA. The Baker Hughes Plan may be
served with process by serving its Plan Administrator, Bernard Casey Makel, at 17021 Aldine
Westfield Houston, TX 77073.
32. Defendant Baylor College of Medicine Health and Welfare Benefits Plan (the
“Baylor Plan”) is a self-funded health plan subject to ERISA. The Baylor Plan may be served with
process by serving its Plan Administrator, Angela Garcia and/or Tamara Norris, at C/O Accounting
One Baylor Plaza Bcm200 Houston, TX 77030.
33. Defendant Brookdale Senior Living, Inc. Welfare Plan (the “Brookdale Plan”) is a
self-funded health plan subject to ERISA. The Brookdale Plan may be served with process by
serving its Plan Administrator, Diane Johnson May, at 6737 W Washington Street Suite 2300
Milwaukee, WI 53214.
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 13 of 89
Page 14 of 89
34. Defendant C.H Robinson Company Group Health Major Medical Plan (the
“Robinson Plan”) is a self-funded health plan subject to ERISA. The Robinson Plan may be served
with process by serving its Plan Administrator, John Donovan, at 14701 Charlson Rd, Eden Prairie,
Mn 55347-5076.
35. Defendant Calpine Corporation Employee Benefit Plan (the “Calpine Plan”) is a
self-funded health plan subject to ERISA. The Calpine Plan may be served with process by
serving its Plan Administrator, Tonja Benjamin, at 717 Texas Ave. Suite 1000 Houston, TX 77002.
36. Defendant Caterpillar Inc. Group Insurance Master Trust (the “Caterpillar Plan”)
is a self-funded health plan subject to ERISA. The Caterpillar Plan may be served with process
by serving its Plan Administrator, Todd Bisping, at 510 Lake Cook Road Deerfield, IL 60015.
37. Defendant Celanese Health and Welfare Benefits Program (the “Celanese Plan”)
is a self-funded health plan subject to ERISA. The Celanese Plan may be served with process by
serving its Plan Administrator, Jose A Motta, at 222 West Las Colinas Boulevard Suite 900N
Irving, TX 75039.
38. Defendant Centerpoint Energy Group Welfare Benefits Plan for Retirees (the
“Centerpoint Plan”) is a self-funded health plan subject to ERISA. The Centerpoint Plan may be
served with process by serving its Plan Administrator, Carla A. Kneipp, at 1111 Louisiana Street
Houston, TX 77002-5230.
39. Defendant Citgo Petroleum Corporation Defined Contribution Master Trust (the
“Citco Plan”) is a self-funded health plan subject to ERISA. The Citco Plan may be served with
process by serving its Plan Administrator, James R. Shoemaker, at Po Box 4689 Houston, TX
77210-4689.
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 14 of 89
Page 15 of 89
40. Defendant Delta Account Based Healthcare Plan (the “Delta Plan”) is a self- funded
health plan subject to ERISA. The Delta Plan may be served with process by serving its Plan
Administrator, Greg Tahvonen, at 1030 Delta Boulevard Atlanta, GA 30354.
41. Defendant Envision Healthcare Corporation Welfare Benefits Plan (the “Envision
Plan”) is a self-funded health plan subject to ERISA. The Envision Plan may be served with
process by serving its Plan Administrator, Donald King, at 1A Burton Hills Boulevard Nashville,
TN 37215.
42. Defendant H&E Equipment Services Inc. Benefit Plan (the “H&E Plan”) is a self-
funded health plan subject to ERISA. The H&E Plan may be served with process by serving its
Plan Administrator, Angela Broocks, at 7500 Pecue Ln Baton Rouge, LA 70809-5107.
43. Defendant Flour Employee Benefit Trust Plan (the “Flour Plan”) is a self-funded
health plan subject to ERISA. The Flour Plan may be served with process by serving its Plan
Administrator, Stacy Dillow, at 6700 Las Colinas Boulevard Irving, TX 75039.
44. Defendant Fresenius Medical Care Travelling Nurses Health and Welfare Benefits
Plan (the “Fresenius Plan”) is a self-funded health plan subject to ERISA. The Fresenius Plan may
be served with process by serving its Plan Administrator, Steven Covino, at 920 Winter Street
Waltham, MA 02451.
45. Defendant Geico Corp. Consolidated Welfare Benefits Program (the “Geico
Plan”) is a self-funded health plan subject to ERISA. The Geico Plan may be served with process
by serving its Plan Administrator, H. A. White and/or J.C Stewart, at C/O Corporation Tax
Division One Geico Plaza Washington, DC 20076.
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 15 of 89
Page 16 of 89
46. Defendant Geospace Technologies Welfare Benefit Plan (the “Geospace Plan”) is
a self-funded health plan subject to ERISA. The Geospace Plan may be served with process by
serving its Plan Administrator, Lacey Rice, at 7007 Pinemont Dr Houston, TX 77040-6601.
47. Defendant Hudson Group (HG) Inc. Employee Benefits Plan (the “Hudson Plan”)
is a self-funded health plan subject to ERISA. The Hudson Plan may be served with process by
serving its Plan Administrator, William Wolf, at One Meadowlands Plaza, 6th Floor East
Rutherford, NJ 07073.
48. Defendant IQOR Health and Welfare Plan (the “IQOR Plan”) is a self-funded
health plan subject to ERISA. The IQOR Plan may be served with process by serving its Plan
Administrator, Ian Carroll, at 200 Central Ave 7th Fl St Petersburg, FL 33701-3566.
49. Defendant Jones Lang Lasalle Group Benefits Plan (the “JLL Plan”) is a self-
funded health plan subject to ERISA. The JLL Plan may be served with process by serving its Plan
Administrator, Tim Quitmeyer, at 200 East Randolph Street Chicago, IL 60601.
50. Defendant Kellogg Brown & Root, Inc, Welfare Benefits Plan (the “KBR Plan”)
is a self-funded health plan subject to ERISA. The KBR Plan may be served with process by
serving its Plan Administrator, Valerie Hulse, at 601 Jefferson Street, Suite 2916 Houston, TX
77002.
51. Defendant Kinder Morgan, Inc. Master Employee Welfare Plan (the “Kinder
Morgan Plan”) is a self-funded health plan subject to ERISA. The Kinder Morgan Plan may be
served with process by serving its Plan Administrator, T. Mark Smith, at 1001 Louisiana Street,
Suite 1000, Houston, TX 77002.
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 16 of 89
Page 17 of 89
52. Defendant Lexicon Pharmaceuticals Inc. Comprehensive Welfare Benefits Plan
(the “Lexicon Plan”) is a self-funded health plan subject to ERISA. The Lexicon Plan may be
served with process by serving its Plan Administrator, Jefferey L. Wade, at 8800 Technology
Forest Pl the Woodlands, TX 77381-1160.
53. Defendant Lineage Logistics LLC Benefits Plan (the “Lineage Plan”) is a self-
funded health plan subject to ERISA. The Lineage Plan may be served with process by serving
its Plan Administrator, Sean Vanderelzen, at 17911 Von Karman, Suite 400 Irvine, CA 92614.
54. Defendant Lockton, Inc. Welfare Benefits Plan (the “Lockton Plan”) is a self-
funded health plan subject to ERISA. The Lockton Plan may be served with process by serving its
Plan Administrator, Janet O’Connor, at 444 w. 47th Street Suite 900 Kansas City, MO 64112.
55. Defendant M/I Homes, Inc. Health, Life and Dental Welfare Plan (the “M/I
Homes Plan”) is a self-funded health plan subject to ERISA. The M/I Homes Plan may be served
with process by serving its Plan Administrator, Karla Cupp, at 4131 Worth Avenue Columbus,
OH 43219.
56. Defendant Maersk Inc. Active Nonunion Health and Welfare Plan (the “Maersk
Plan”) is a self-funded health plan subject to ERISA. The Maersk Plan may be served with process
by serving its Plan Administrator, Jennifer M. Swartz, at 180 Park Avenue Florham Park, NJ 07932.
57. Defendant the Mallinckrodt Pharmaceuticals Welfare Benefit Plan (the
“Mallinckrodt Plan”) is a self-funded health plan subject to ERISA. The Mallinckrodt Plan may
be served with process by serving its Plan Administrator, Cathryn Beisel, at 675 Mcdonnell
Boulevard Hazelwood, MO 63042.
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 17 of 89
Page 18 of 89
58. Defendant Motiva Enterprises LLC Health and Wellness Benefit Plan (the
“Motiva Plan”) is a self-funded health plan subject to ERISA. The Motiva Plan may be served
with process by serving its Plan Administrator, Dennis Fox, at 500 Dallas St 4th Fl Houston, TX
77002-4800.
59. Defendant Novo Nordisk Inc. Welfare Benefit Plan (the “Novo Plan”) is a self-
funded health plan subject to ERISA. The Novo Plan may be served with process by serving its
Plan Administrator, Pamela Gottlieb, at 800 Scudders Mill Road Plainsboro, NJ 08536.
60. Defendant Petsmart Smartchoices Benefit Plan (the “Petsmart Plan”) is a self-
funded health plan subject to ERISA. The Petsmart Plan may be served with process by serving
its Plan Administrator, Chris Stillman, at 19601 North 27th Avenue Phoenix, AZ 85027.
61. Defendant Procter and Gamble Retiree Welfare Benefits Plan (the “Proctor and
Gamble Plan”) is a self-funded health plan subject to ERISA. The Proctor and Gamble Plan may
be served with process by serving its Plan Administrator, Kyle Schiedler, at Procter and Gamble
Tax Division P.O. Box 599 Cincinnati, OH 45201.
62. Defendant Railroad Employees National Health Flexible Spending Account Plan
(the “Railroad Plan”) is a self-funded health plan subject to ERISA. The Railroad Plan may be
served with process by serving its Plan Administrator, Brendan M. Brandon, 251 - 18TH Street,
South, Suite 750, Arlington, VA 22202.
63. Defendant Raising Canes USA Health and Welfare Benefits Wrap Plan (the
“Raising Canes Plan”) is a self-funded health plan subject to ERISA. The Raising Canes Plan may
be served with process by serving its Plan Administrator, Ashlee Glock, 6800 Bishop Road Plano,
TX 75024.
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 18 of 89
Page 19 of 89
64. Defendant Republic Services Inc. Employee Benefit Plan (the “Republic
Services Plan”) is a self-funded health plan subject to ERISA. The Republic Services Plan may be
served with process by serving its Plan Administrator, Ann Reed, 18500 North Allied Way
Phoenix, AZ 85054.
65. Defendant Republic National Distributing Company, LLC Welfare Benefits Plan
(the “Republic National Plan”) is a self-funded health plan subject to ERISA. The Republic
National Plan may be served with process by serving its Plan Administrator, Shannon Dacus,
One National Drive, S.W. Atlanta, GA 30336.
66. Defendant Saia Motor Freight Line LLC Employee Preferred Provider Plan (the
“Saia Plan”) is a self-funded health plan subject to ERISA. The Saia Plan may be served with
process by serving its Plan Administrator, Kristy Roger, 11465 Johns Creek Parkway Suite 400
Johns Creek, GA 30097.
67. Defendant Siemens Corporation Group Insurance and Flexible Benefits Program
(the “Siemens Plan”) is a self-funded health plan subject to ERISA. The Siemens Plan may be
served with process by serving its Plan Administrator, Ewout Naarding, 170 Wood Ave. South
Iselin, NJ 08830.
68. Defendant Skadden, Arps, Slate, Meagher & Flom Partners’ Welfare Benefits Plan
(the “Skadden Plan”) is a self-funded health plan subject to ERISA. The Skadden Plan may be
served with process by serving its Plan Administrator, Joseph M. Penko, Lisa Gross, One
Manhattan West New York, NY 10001-8602.
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 19 of 89
Page 20 of 89
69. Defendant Skywest Inc. Cafeteria Plan (the “Skywest Plan”) is a self-funded
health plan subject to ERISA. The Skywest Plan may be served with process by serving its Plan
Administrator, Robert J. Simmons, 444 South River Road St. George, UT 84790.
70. Defendant Southwest Airlines Co. Welfare Benefit Plan (the “Southwest Plan”) is
a self-funded health plan subject to ERISA. The Southwest Plan may be served with process by
serving its Plan Administrator, Julie Weber, 2702 Love Field Drive, Hdq-6tx Dallas, TX 75235.
71. Defendant Spirit Airlines Inc. Health and Welfare Benefits Plan (the “Spirit Plan”)
is a self-funded health plan subject to ERISA. The Spirit Plan may be served with process by
serving its Plan Administrator, Carolyn Hernandez, 2800 Executive Way Miramar, FL 33025.
72. Defendant Swissport North America Holdings, Inc. Health & Welfare Plan (the
“Swissport Plan”) is a self-funded health plan subject to ERISA. The Swissport Plan may be served
with process by serving its Plan Administrator, Giancarlo Ladaga, 45025 Aviation Drive Dulles,
VA 20166.
73. Defendant Targa Resources LLC Welfare Benefits Plan (the “Targa Plan”) is a self-
funded health plan subject to ERISA. The Targa Plan may be served with process by serving its
Plan Administrator, Jennifer Kneale, 811 Louisiana St. Suite 2100 Houston, TX 77002.
74. Defendant Texas Capital Bancshares Inc. Employee Benefit Plan (the “Texas
Capital Plan”) is a self-funded health plan subject to ERISA. The Texas Capital Plan may be served
with process by serving its Plan Administrator, Mandy Barrera, 2000 Mckinney Ave Ste 700
Dallas, TX 75201.
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 20 of 89
Page 21 of 89
75. Defendant Textron Non-Bargained Welfare Benefits Plan (the “Textron Plan”) is a
self-funded health plan subject to ERISA. The Textron Plan may be served with process by serving
its Plan Administrator, Joyce Lafond, 40 Westminster Street Providence, RI 02903.
76. Defendant Adecco, Inc Welfare Benefits Plan (the “Adecco Plan”) is a self-funded
health plan subject to ERISA. The Adecco Plan may be served with process by serving its Plan
Administrator, Brian P. Evans, 10151 Deerwood Park Blvd Building 200, Suite 400 Jacksonville,
FL 32256.
77. Defendant T-Mobile USA, Inc. Employee Benefit Plan (the “T-Mobile Plan”) is a
self-funded health plan subject to ERISA. The T-Mobile Plan may be served with process by
serving its Plan Administrator, Kate Blaylock, 12920 Se 38th Street Bellevue, WA 98006.
78. Defendant Transocean Group Welfare Benefits Plan (the “Transocean Plan”) is a
self-funded health plan subject to ERISA. The Transocean Plan may be served with process by
serving its Plan Administrator, Nathaniel Peneguy, P.O. Box 10342, 36C Dr. Roy's Drive Bermuda
House, 4th Floor Cayman Islands, Grand Cayman 1-1003 KY KY.
79. Defendant UHS Welfare Benefit Plan (the “UHS Welfare Plan”) is a self-funded
health plan subject to ERISA. The UHS Welfare Plan may be served with process by serving its
Plan Administrator, Virginia Cullinan, 367 South Gulph Road King of Prussia, PA 19406.
80. Defendant UnitedHealth Group Ventures, LLC Health and Welfare Benefit Plan
(the “UnitedHealth Group Plan”) is a self-funded health plan subject to ERISA. The UnitedHealth
Group Plan may be served with process by serving its Plan Administrator, Rob Webb, 9900 Bren
Road East Mn008-B217 Minnetonka, MN 55343.
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 21 of 89
Page 22 of 89
81. Defendant Valero Energy Corporation Retiree Benefits Plan (the “Valero Plan”) is
a self-funded health plan subject to ERISA. The Valero Plan may be served with process by serving
its Plan Administrator, Christina Jennings, P.O. Box 696000 San Antonio, TX 78269, One Valero
Way MS E1T San Antonio, TX 78249.
82. Defendant Valmont Industries Inc. Welfare Benefit Plan (the “Valmont Plan”) is a
self-funded health plan subject to ERISA. The Valmont Plan may be served with process by
serving its Plan Administrator, Jennifer Paisley, One Valmont Plaza Omaha, NE 68154.
83. Defendant Walgreen Health and Welfare Plan (the “Walgreen Plan”) is a self-
funded health plan subject to ERISA. The Walgreen Plan may be served with process by serving
its Plan Administrator, Todd Bajek, 102 Wilmot Road MS#122H Deerfield, IL 60015
84. Defendant WCA Management Company, LP Welfare Benefit Plan (the “WCA
Plan”) is a self-funded health plan subject to ERISA. The WCA Plan may be served with process
by serving its Plan Administrator, Joe Saad, 1330 Post Oak Boulevard, 7th Floor Houston, TX
77056.
85. Defendant Webber, LLC Welfare Benefit Plan (the “Webber Plan”) is a self-
funded health plan subject to ERISA. The Webber Plan may be served with process by serving
its Plan Administrator, Jared Branch, 1725 Hughes Landing Blvd Suite 1200 The Woodlands, TX
77380.
86. Defendant Winstead PC Flexible Benefit Plan (the “Winstead Plan”) is a self-
funded health plan subject to ERISA. The Winstead Plan may be served with process by serving
its Plan Administrator, Lydia Dillon, 2728 N Harwood Street Suite 500 Dallas, TX 75201.
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 22 of 89

Page 23 of 89
87. Defendant Group Benefits Plan for Employees of Worleyparsons Corporation (the
“Worleyparsons Plan”) is a self-funded health plan subject to ERISA. The Worleyparsons Plan
may be served with process by serving its Plan Administrator, Jennifer Miller, 2675 Morganton
Road, Reading, PA 19607-9676.
JURISDICTION ANE VENUE
88. This Court has federal question subject matter jurisdiction over this matter pursuant
to 28 U.S.C. § 1131, as Plaintiff asserts federal claims against United and Employer Plans in
Counts I, II, and III, under the FFCRA, the CARES Act, and ERISA.
89. This Court also has federal question subject matter jurisdiction over this matter
pursuant to 28 U.S.C. § 1131, as Plaintiff asserts federal claims against United in Count IV, under
RICO.
90. This Court also has supplemental jurisdiction over Plaintiff’s state law claims
against United, in Counts V, VI, VII, VIII, and IX because these claims are so related to Plaintiff’s
federal claims that the state law claims form a part of the same case or controversy under Article
III of the United States Constitution. The Court has supplemental jurisdiction over these claims
pursuant to 28 U.S.C. § 1367(a).
91. Venue is appropriate in this Court under 28 U.S.C. § 1391(b)(2) because a
substantial portion of the events giving rise to this action arose in this District.
[INTENTIONALLY LEFT BLANK]
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 23 of 89

Page 24 of 89
BACKGROUND AS TO THE FFCRA AND THE CARES ACT
92. Pursuant to Section 319 of the Public Health Service Act, on January 31, 2020, the
Secretary of Health and Human Services (“HHS”) issued a determination that a Public Health
Emergency exists and has existed as of January 27, 2020, due to confirmed cases of COVID-19
being identified in this country.
7
93. On March 13, 2020, the President issued Proclamation 9994 declaring a National
Emergency concerning the COVID-19 outbreak with a determination that a national emergency
exists nationwide, pursuant to Section 501(b) of the Robert T. Stafford Disaster Relief and
Emergency Assistance Act.
94. To facilitate the nation’s response to the COVID-19 pandemic, Congress passed
the FFCRA and the CARES Act to, amongst other things, require group health plans and health
insurance issuers offering group or individual health insurance coverage to: (i) provide benefits
for certain items and services related to diagnostic testing for the detection or diagnosis of COVID-
19 without the imposition of any cost-sharing requirements (i.e. deductibles, copayments, and
coinsurance) or prior authorization or other medical management requirements;
8
and (ii) to
reimburse any provider for COVID-19 diagnostic testing an amount that equals the negotiated rate
or, if the plan or issuer does not have a negotiated rate with the provider (e.g. Plaintiff), the cash
price for such service that is listed by the provider on its public website in accordance with 45 CFR
§ 182.40.
9
95. To further clarify to issuers and health plans their legal expectations when
processing a claim for Covid Testing in accordance with the FFCRA and the CARES Act, the
7
See https://www.phe.gov/emergency/news/healthactions/phe/Pages/2019-nCoV.aspx (Determination that a Public
Health Emergency Exists).
8
Pub. L. No. 116-127 (2020).
9
Pub. L. No. 116-136 (2020).
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 24 of 89

Page 25 of 89
Department of Labor (“DOL”), the Department of Health and Human Services (“HHS”), and the
Department of the Treasury (the “Treasury”) (collectively, the “Departments”) jointly prepared
and issued a series of Frequently Asked Questions (“FAQs”) to address any stakeholder questions
or concerns pertaining to the proper adjudication of Covid Testing claims. The following FAQs
summarize the health plan and issuers’ obligations as it pertains to covering and paying for Covid
Testing services during the public health emergency:
The Departments FAQ, Part 42, Q1: Which types of group health plans and health insurance
coverage are subject to section 6001 of the FFCRA, as amended by section 3201 of the CARES
Act?
Section 6001 of the FFCRA, as amended by section 3201 of the CARES Act, applies to group
health plans and health insurance issuers offering group or individual health insurance coverage
(including grandfathered health plans as defined in section 1251(e) of the Patient Protection and
Affordable Care). The term “group health plan” includes both insured and self-insured group health
plans. It includes private employment-based group health plans (ERISA plans), non-federal
governmental plans (such as plans sponsored by states and local governments), and church plans.
“Individual health insurance coverage” includes coverage offered in the individual market through
or outside of an Exchange, as well as student health insurance coverage (as defined in 45 CFR
147.145).
10
The Departments FAQ, Part 42, Q3: What items and services must plans and issuers provide
benefits for under section 6001 of the FFCRA?
Section 6001(a) of the FFCRA, as amended by Section 3201 of the CARES Act, requires plans and
issuers to provide coverage for the following items and services:
(1) An in vitro diagnostic test as defined in section 809.3 of the title 21, Code of Federal
Regulations, (or its successor regulations) for the detection of SARS-CoV-2 or the diagnosis of
COVID-19, and the administration of such a test, that - …
B. The developer has requested, or intends to request, emergency use authorization
under section564 of the Federal Food, Drug, and Cosmetic Act (21 U.S.C. 360bbb-3), unless and
until the emergency use authorization request under such section 564 has been denied or the
developer of such test does not submit a request under such section within a reasonable
timeframe;…
11
10
See https://www.cms.gov/files/document/FFCRA-Part-42-FAQs.pdf.
11
Id.
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 25 of 89

Page 26 of 89
The Departments FAQ, Part 42, Q6: May a plan or issuer impose any cost-sharing requirements,
prior authorization requirements, or other medical management requirements for benefits that
must be provided under section 6001(a) of the FFCRA, as amended by section 3201 of the CARES
Act?
No. Section 6001(a) of the FFCRA provides that plans and issuers shall not impose any cost-sharing
requirements (including deductibles, copayments, and coinsurance), prior authorization
requirements, or other medical management requirements for these items and services. These items
and services must be covered without cost sharing when medically appropriate for the individual,
as determined by the individual’s attending healthcare provider in accordance with accepted
standards of current medical practice.
12
The Departments FAQ, Part 42, Q7: Are plans and issuers required to provide coverage for
items and services that are furnished by providers that have not agreed to accept a negotiated rate
as payment in full (i.e., out-of-network providers)?
Yes. Section 3202(a) of the CARES Act provides that a plan or issuer providing coverage of items
and services described in section 6001(a) of the FFCRA shall reimburse the provider of the
diagnostic testing as follows: …
2. If the plan or issuer does not have a negotiated rater with such provider, the plan or issuer
shall reimburse the provider in an amount that equals the cash price for such service as listed by
the provider on a public internet website, or the plan or issuer may negotiate a rate with the provider
for less than such cash price…
13
The Departments FAQ, Part 43, Q9: Does Section 3202 of the CARES Act protect participants,
beneficiaries, and enrollees from balance billing for a COVID-19 diagnostic test?
The Departments read the requirement to provide coverage without cost sharing in section 6001 of
the FFCRA, together with section 3202(a) of the CARES Act establishing a process for setting
reimbursement rates, as intended to protect participants, beneficiaries, and enrollees from being
balance billed for an applicable COVID-19 test. Section 3202(a) contemplates that a provider of
COVID-19 testing will be reimbursed either a negotiated rate or an amount that equals the cash
price for such service that is listed by the provider on a public website. In either case, the amount
the plan or issuer reimburses the provider constitutes payment in full for the test, with no cost
sharing to the individual or other balance due. Therefore, the statute generally precludes balance
billing for COVID-19 testing. However, section 3202(a) of the CARES Act does not preclude
balance billing for items and services not subject to section 3202(a), although balance billing may
be prohibited by applicable state law and other applicable contractual agreements.
14
12
Id.
13
Id.
14
See https://www.cms.gov/files/document/FFCRA-Part-43-FAQs.pdf; See also FAQ Part 43 Q12: … Because the
Departments interpret the provisions of section 3202 of the CARES Act as specifying a rate that generally protects
participants, beneficiaries, and enrollees from balance billing for a COVID-19 test (see Q9 above), the requirement to
pay the greatest of three amounts under the regulations implementing section 2719A of the PHS Act is superseded by
the requirements of section 3202(a) of the CARES Act with regard to COVID-19 diagnostic tests that are out-of-
network emergency services. For these services, the plan or issuer must reimburse an out-of-network provider of
COVID-19 testing an amount that equals the cash price for such service that is listed by the provider on a public
website, or the plan or issuer may negotiate a rate that is lower than the cash price.
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 26 of 89

Page 27 of 89
The Departments FAQ, Part 44, Q1: Under the FFCRA, can plans and issuers use medical
screening criteria to deny (or impose cost sharing on) a claim for COVID-19 diagnostic testing for
an asymptomatic person who has no known or suspected exposure to COVID-19?
No. The FFCRA prohibits plans and issuers from imposing medical management, including
specific medical screening criteria, on coverage of COVID-19 diagnostic testing. Plans and issuers
cannot require the presence of symptoms or a recent known or suspected exposure, or otherwise
impose medical screening criteria on coverage of tests.
When an individual seeks and receives a COVID-19 diagnostic test from a licensed or authorized
health care provider, or when a licensed or authorized health care provider refers an individual for
a COVID-19 diagnostic test, plans and issuers generally must assume that the receipt of the test
reflects an “individualized clinical assessment” and the test should be covered without cost sharing,
prior authorization, or other medical management requirements.
15
The Departments FAQ, Part 44, Q3: Under the FFCRA, are plans and issuers required to cover
COVID-19 diagnostic tests provided through state- or locality-administered testing sites?
Yes. As stated in FAQs Part 43, Q3, any health care provider acting within the scope of their license
or authorization can make an individualized clinical assessment regarding COVID-19 diagnostic
testing. If an individual seeks and receives a COVID-19 diagnostic test from a licensed or
authorized provider, including from a state- or locality-administered site, a “drivethrough” site,
and/or a site that does not require appointments, plans and issuers generally must assume that the
receipt of the test reflects an “individualized clinical assessment.”
16
The Departments FAQ, Part 44, Q5: What items and services are plans and issuers required to
cover associated with COVID-19 diagnostic testing? What steps should plans and issuers take to
help ensure compliance with these requirements?
… Plans and issuers should maintain their claims processing and other information technology
systems in ways that protect participants, beneficiaries, and enrollees from inappropriate cost
sharing and should document any steps that they are taking to do so…
17
96. To supplement the FAQs publicized by the Departments, the Internal Revenue
Service (the “IRS”) issued Notice 2020-15 pertaining to high deductible health plans (“HDHPs”)
and expenses related to COVID-19 to provide members of HDHPs (including those HDHPs
insured or administered by United) the confidence that Covid Testing will be covered, in full, by
their HDHP. Notice 2020-15 states as follows:
15
See https://www.cms.gov/files/document/faqs-part-44.pdf.
16
Id.
17
Id.
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 27 of 89

Page 28 of 89
[d]ue to the unprecedented public health emergency posed by COVID-19, and the
need to eliminate potential administrative and financial barriers to testing for and
treatment of COVID-19 [emphasis added], a health plan that otherwise satisfies the
requirements to be an HDHP under section 223(c)(2)(A) will not fail to be an
HDHP merely because the health plan provides medical care services and items
purchased related to testing for and treatment of COVID-19 prior to the satisfaction
of the applicable minimum deductible.
97. In addition to the federal guidance publicized by the Departments, the Texas
Department of Insurance (“TDI”) issued Commissioner’s Bulletin # B-0017-20, which also
pertains to coverage for COVID-19 testing and network adequacy. In this Bulletin, TDI mandates
exclusive provider networks (“EPOs”) and health maintenance organizations (“HMOs”) to comply
with the Covid Testing adjudication requirements of the FFCRA and the CARES Act, and
“instructs health plans to pay a provider’s negotiated rate or, if a health plan does not have a
negotiated rate with the provider, pay the provider’s publicly available cash price for testing
[emphasis added].”
18
[INTENTIONALLY LEFT BLANK]
18
In an inquiry posed by Plaintiff to TDI pertaining to the applicability of Commissioner’s Bulletin #B-0017-20 to
PPO and POS plans, TDI states the following: “Yes, it is TDI’s position that PPO and POS plans must also comply
with FFCRA and the ‘CARES Act’ … Commissioner’s Bulletin #B-0017-20 made it expressly clear that in-network
based plans, “insurers offering exclusive provider networks (EPOs) and health maintenance organizations (HMOs)…
fall within the federal definitions for group health plans or health insurance issuers offering group or individual health
insurance coverage.” Presumably, the purpose of the bulletin was to expressly clarify for network-based plans such as
EPOs and gated HMO plans our expectation to protect consumers regardless of network affiliation, as contemplated
by the CARES Act and by Texas’ laws. PPO and EPO issuers are subject to but not limited to Texas Insurance Code
(TIC) Chapter 1301. HMOs may issue POS plans as required under TIC Chapter 1273. As PPO and POS plans are
captured under the terms “issuer”, “HMO”, “group health plans”, “health insurance issuers”, and “individual health
insurance coverage”; PPO and POS plans are not excluded from compliance.”
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 28 of 89

Page 29 of 89
UNITED’S PUBLIC-FACING REPRESENTATIONS REGARDING COMPLIANCE
WITH THE FFCRA, THE CARES ACT, AND OTHER APPLICABLE AUTHORITIES
98. Since the start of the public health emergency and Congress’s passing of the
FFCRA and the CARES Act, United has consistently made public-facing representations
regarding its obligations to comply with the requirements of the FFCRA and the CARES Act and
to process Covid Testing claims accordingly. These representations can be found on United’s
websites and other publications.
99. The following are public-facing statements made by United on its websites and
other publications regarding its obligations to process Covid Testing service claims in accordance
with the FFCRA and the CARES Act:
Our Response to COVID-19
19
[INTENTIONALLY LEFT BLANK]
19
https://www.uhc.com/health-and-wellness/health-topics/covid-19/our-response (June 16, 2021).
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 29 of 89

Page 30 of 89
COVID-19 Testing and Cost Share Guidance
20
COVID-19 Testing, Treatment, Coding & Reimbursement
21
20
https://www.uhcprovider.com/en/resource-library/news/Novel-Coronavirus-COVID-19/covid19-testing/covid19-
testing-guidance.html (June 16, 2021).
21
https://www.uhcprovider.com/en/resource-library/news/Novel-Coronavirus-COVID-19/covid19-testing.html
(June 16, 2021).
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 30 of 89

Page 31 of 89
United Healthcare COVID-19 Billing Guide
22
Your Questions Answered
23
COVID-19 Temporary Provisions
24
22
https://www.uhcprovider.com/content/dam/provider/docs/public/resources/news/2020/covid19/UHC-COVID-19-
Provider-Billing-Guidance.pdf (June 16, 2021).
23
https://www.uhc.com/health-and-wellness/health-topics/covid-19/your-questions-answered (June 16, 2021).
24
https://www.uhcprovider.com/content/dam/provider/docs/public/resources/news/2020/covid19/COVID-19-Date-
Provision-Guide.pdf (June 16, 2021).
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 31 of 89

Page 32 of 89
Understanding COVID-19 Testing and Treatment Coverage
25
United FAQ Regarding All Savers
26
[INTENTIONALLY LEFT BLANK]
25
https://www.uhc.com/health-and-wellness/health-topics/covid-19/coverage-and-resources (June 16, 2021).
26
https://www.uhc.com/content/dam/uhcdotcom/en/B2B-Newsletters/b2b-pdf/covid-19/faqs-all savers.pdf (June 16,
2021).
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 32 of 89

Page 33 of 89
United FAQ Regarding Federal Guidance
27
United FAQ Regarding ASO – Business Disruption and Stop Loss Support
28
27
https://www.uhc.com/content/dam/uhcdotcom/en/B2B-Newsletters/b2b-pdf/covid-19/faqs-federal guidance.pdf
(June 16, 2021).
28
https://www.uhc.com/content/dam/uhcdotcom/en/B2B-Newsletters/b2b-pdf/covid-19/faqs
aso business disruption and stop loss.pdf (June 16, 2021).
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 33 of 89

Page 34 of 89
United FAQ Regarding Products and Programs
29
[INTENTIONALLY LEFT BLANK]
29
https://www.uhc.com/content/dam/uhcdotcom/en/B2B-Newsletters/b2b-pdf/covid-19/faqs-
programs and products.pdf (June 16, 2021).
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 34 of 89

Page 35 of 89
United FAQ Regarding Testing
30
30
https://www.uhc.com/content/dam/uhcdotcom/en/B2B-Newsletters/b2b-pdf/covid-19/faqs-testing.pdf (June 16,
2021).
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 35 of 89

Page 36 of 89
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 36 of 89

Page 37 of 89
31
United FAQ Regarding Claims and Appeals
32
100. Despite these numerous public-facing representations directed towards its
members, to health plans that it administers (including the Employer Plans), and providers of
Covid Testing services (e.g., Plaintiff), United’s actions and conduct, to be detailed below, shows
its intentional disregard for complying with all applicable authorities.
31
The CDC’s Covid Testing provider/laboratory search function identifies Plaintiff as an eligible lab and testing site
to receive Covid Testing. Further, United’s Covid Testing provider/laboratory search functions also lead to Plaintiff’s
laboratory and testing locations.
32
https://www.uhc.com/content/dam/uhcdotcom/en/B2B-Newsletters/b2b-pdf/covid-19/faqs-claims.pdf (June 16,
2021).
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 37 of 89

Page 38 of 89
FACTUAL ALLEGATIONS COMMON TO ALL COUNTS
a. The Improper Record Request Scheme and the Imposition of Prohibited Medical
Management Requirements
101. As explained above, Section 6001 of the FFCRA expressly prohibits the imposition
of medical management requirements as a condition of coverage and reimbursement for Covid
Testing services regardless of whether the testing provider is in-network or OON.
102. However, despite this prohibition, United implemented an unlawful scheme that
consists of improper, irrelevant, and burdensome medical record requests to Plaintiff for the sole
purpose of denying as many claims for bona fide Covid Testing services submitted by Plaintiff as
possible (the “Improper Record Request Scheme”). The details of United’s Improper Record
Request Scheme are set forth below.
i. Details of United’s Improper Record Request Scheme
103. Regardless of the fact that Plaintiff is a CLIA certified high complexity laboratory,
holds all proper FDA emergency use authorizations and approvals necessary, and is identified by
the CDC and Texas Department of State Health Services Covid Testing locator functions as a
qualified laboratory to render Covid Testing services, United deployed its Improper Record
Request Scheme against Plaintiff with the intended purpose of placing barriers and denying Covid
Testing claims for its own financial benefit.
104. Since the time Plaintiff commenced with submitting Covid Testing claims to
United for reimbursement, United almost immediately responded with sending identical pre-
payment record request letters to Plaintiff for the following materials:
• Physician’s orders for the laboratory test, including any standing orders and/or
provider custom panel orders, whether for the ordering provider or all referring
providers;
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 38 of 89

Page 39 of 89
• Laboratory testing method, specimen type, and test results related to all billed
services;
• CLIA Documentation (certificates, licenses, permits, etc.);
• Manufacturer and model number of the testing equipment used for billed
services; and
• Manufacturer and brand information for all test supplies used for billed
services.
105. United’s request for the aforementioned records for almost every claim submitted
conflicts with the presumption created by FFCRA, the CARES Act, and supportive guidance that
all Covid Testing claims submitted to issuers or health plans for reimbursement are medically
appropriate, ordered by a licensed medical professional, and that the receipt of the test reflects an
“individualized clinical assessment”.
33
These record requests conflict with this presumption and is
an overly burdensome and improper condition of payment to Plaintiff.
106. Of important note, aside from a copy of a signed order form from a medical
professional establishing the need for Covid Testing, the rest of the records/materials requested by
United on almost every single claim are not unique to that particular Covid Testing claim. Instead,
requests for laboratory testing methods, CLIA documentation, and testing equipment and supplies
information should be directly made to the provider of such services and should not be used to
expand the scope by which pre-payment record request denials may be made by United on a claim-
by-claim basis.
33
The Departments FAQ, Part 44, Q3: Under the FFCRA, are plans and issuers required to cover COVID-19
diagnostic tests provided through state- or locality-administered testing sites?
Yes. As stated in FAQs Part 43, Q3, any health care provider acting within the scope of their license or authorization
can make an individualized clinical assessment regarding COVID-19 diagnostic testing. If an individual seeks and
receives a COVID-19 diagnostic test from a licensed or authorized provider, including from a state- or locality-
administered site, a “drivethrough” site, and/or a site that does not require appointments, plans and issuers generally
must assume that the receipt of the test reflects an “individualized clinical assessment.”
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 39 of 89

Page 40 of 89
107. Furthermore, when United made medical record requests on a claim-by-claim basis
to Plaintiff, United’s Special Investigations Unit (the “SIU”) simultaneously made the same record
requests directly to Plaintiff on October 8, 2020, and November 16, 2020, for the purpose of
“confirming the logistics and the capability of the laboratory to provide services to UHC [United]
patients.”
34
As part of United SIU’s investigation, the following information and materials were
requested:
• Laboratory Identification Information (e.g., Name, NPI, EIN, Address);
• CLIA Certification Information and Scope of Laboratory Services;
• Laboratory Director and Other Personnel Information;
• Premises and Security Information; and
• Laboratory Equipment and Supplies Information.
108. The requested information and materials were provided to United on November 17,
2020.
35
Since this date, United has not contacted Plaintiff regarding any supplemental or
subsequent requests, made any additional inquiries regarding the legitimacy of Plaintiff, expressed
any concerns about Plaintiff and its ability to render Covid Testing services, nor informed Plaintiff
about the status of its investigation. In fact, Plaintiff inquired with United’s SIU regarding the
status of the investigation and notified United’s SIU that if no response was received within a set
time period, the SIU investigation shall be de facto closed.
36
United’s SIU did not respond.
109. Given that United’s claim-by-claim record requests and United’s SIU record
request both commenced in October 2020, Plaintiff reasonably assumed, as would any reasonably
prudent person, that the purpose of the requests were to confirm that Plaintiff is a qualified lab
34
See Exhibit A (United SIU Record Request Letters dated October 8, 2020, and November 16, 2020).
35
See Exhibit B (United SIU Record Request Proof of Submission on November 17, 2020).
36
See Exhibit C (Plaintiff Email to United re the Status of SIU Investigation dated May 19, 2021).
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 40 of 89

Page 41 of 89
capable of rendering Covid Testing services. Therefore, Plaintiff complied with both the claim-
by-claim and UHC SIU requests. However, even though Plaintiff directly provided United’s SIU
with the information and materials that were requested and provided substantially similar materials
on the claim-by-claim requests, United unreasonably continued with making the same generic
requests for information by the thousands which leads Plaintiff to believe that United has not even
reviewed the materials provided and is purposefully leading Plaintiff along.
110. The thousands upon thousands of requests for the same information and materials
specific to the qualifications and abilities of Plaintiff has overwhelmed and inundated Plaintiff;
thus, allowing United to deny thousands of claims on the technicality that Plaintiff did not provide
the requested records within the time period prescribed by United despite the same materials and
information being provided to United and its SIU nearly 2,000 times.
111. Furthermore, even when Plaintiff does submit records to United on claim-specific
requests, United has created arbitrary criteria to review records that are inconsistently applied for
the purpose of denying or substantially underpaying on the majority of Covid Testing claims that
Plaintiff has provided requested records for. The arbitrary records review process in furtherance
of the Improper Record Request Scheme is explained below.
ii. United’s Arbitrary and Inconsistent Review of Requested Records
112. Because Plaintiff only provides Covid Testing services and no other laboratory
services, Plaintiff is in the unique position that all claims being electronically submitted to United
via the HCFA-1500 forms are uniformly constructed and submitted. Given the uniformity of the
Covid Testing services and the electronic claims being submitted to United coupled with the
Federal and State mandates that require United to process Covid Testing claims submitted by OON
providers in a very singular fashion, Plaintiff’s very reasonable expectation was that all Covid
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 41 of 89

Page 42 of 89
Testing claims should be paid at Plaintiff’s cash price since United, to date, has not even attempted
to negotiate an amount to be paid despite Plaintiff’s good faith attempts to do so.
113. Leaving aside the unlawful and burdensome nature of United’s Improper Record
Request Scheme, Plaintiff also assumed that compliance with United’s claim-by-claim record
requests would lead to a consistent review and adjudication of Plaintiff’s Covid Testing claims
since all Covid Testing claims and requested records submitted to United are the same or
substantially similar. That is far from the case.
114. By way of example, below are two Covid Testing claims submitted to United where
United also requested records from Plaintiff for that particular claim. Despite the same Covid
Testing services being provided to these two patients, who are members of health plans either
insured or administered by United and the same records being submitted to United on behalf of
these two members’ claims, United’s adjudication of these claims had two different outcomes.
115. Patient JF received Covid Testing services from Plaintiff on July 31, 2020, and is a
member of an HMO plan that is fully-insured by United and subject to the jurisdiction of TDI;
therefore, this particular Covid Testing claim should be adjudicated in accordance with TDI
Commissioner’s Bulletin No. B-0017-20 which mandates compliance with the FFCRA and the
CARES Act. A copy of Patient JF’s electronic HCFA-1500 claims form is copied below:
[INTENTIONALLY LEFT BLANK]
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 42 of 89

Page 43 of 89
116. Upon receipt of Patient JF’s claim, United requested records from Plaintiff, and
those records were submitted to United on November 6, 2020.
37
Surprisingly, United allowed and
paid the full cash price on this claim; however, for the Covid Testing claim detailed below, the
37
See Exhibit D (Medical Records Submitted to United on Patient JF’s Claim).
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 43 of 89
Page 44 of 89
outcome of the record review is completely different despite the fact that the HCFA 1500 forms
and the records submitted to United being the same.
117. Patient MM also received Covid Testing services from Plaintiff on July 31, 2020,
and is a member of an PPO plan that is fully-insured by United and subject to the jurisdiction of
TDI; therefore, like Patient JF’s claim, this particular Covid Testing claim should also be
adjudicated in accordance with TDI Commissioner’s Bulletin No. B-0017-20 which mandates
compliance with the FFCRA and the CARES Act. A copy of Patient MM’s electronic HCFA-1500
claims form is copied below:
[INTENTIONALLY LEFT BLANK]
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 44 of 89

Page 45 of 89
118. Upon receipt of Patient MM’s claim, United requested records from Plaintiff and
those records were submitted to United on November 12, 2020.
38
Instead of adjudicating Patient
MM’s Covid Testing claim in the same manner as Patient JF’s claim, United denied the claim for
38
See Exhibit E (Medical Records Submitted to United on Patient MM’s Claim).
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 45 of 89

Page 46 of 89
the following reasons:
119. It is clear that Patient MM’s claim does not lack information or billing errors, and
the records provided to United are not incomplete or deficient because Patient JF’s claim did not
lack information or have any billing errors, nor did the records submitted to United on Patient JF’s
claim lack any information or were deficient in any way.
120. In furtherance of its Improper Record Request Scheme, United makes the following
misrepresentations to Patient MM and other United members’ whose claims are denied for the
same or similar reasons:
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 46 of 89
Page 47 of 89
121. United makes these misrepresentations to Patient MM and other United members,
whose claims are denied for the same or similar reasons, despite knowing that these comments are
categorically false. These misrepresentations are meant to make a scapegoat of Plaintiff to United
members and to health plans that United administers (e.g. Employee Plans) when members’ claims
are denied for purported issues or deficiencies with claim submissions and/or Plaintiff’s medical
records.
122. Plaintiff contacted United on May 21, 2021, specifically regarding the
inconsistency of how Patient JF and Patient MM’s Covid Testing claims were adjudicated. By the
United representative’s own admission, there are no differences between Patient JF and Patient
MM’s claim, and Patient MM’s claim should have been adjudicated in the same manner as Patient
JF’s claim.
123. The United representative informed Plaintiff that the Patient MM’s claim would be
reprocessed and paid in accordance with Patient JF’s claim within 15 days from the date of the
call, but, as of the date of this Original Complaint, Patient MM’s claim remains denied.
124. The United representative further explains that claims and the records provided in
response to each record request may not be reviewed under one singular approach, and, if reviewed
under one singular approach, that each United representative tasked with reviewing the Covid
Testing claims has different learning curves. Therefore, no level of consistency in the adjudication
of Covid Testing claims can be achieved, even if those same claims are identical to one another.
125. United’s failures to provide proper training, policies, and instructions to its
representatives tasked with the review of Covid Testing claims and/or records relevant to the Covid
Testing claims is an intentional institutional failure meant to further perpetuate its Improper Record
Request Scheme.
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 47 of 89

Page 48 of 89
iii. Inquiries to United Pertaining to the Improper Record Request Scheme
126. In addition to Plaintiff’s call to United regarding Patient JF and Patient MM’s
claims, Plaintiff has made many other attempts to solicit a response from United regarding the
Improper Record Request Scheme, but United has ducked and weaved through all of Plaintiff’s
attempts.
127. In one particular email exchange with Optum’s Head of Regulatory Affairs,
Plaintiff clearly and unequivocally pressed United to respond to the following inquiries: (i) why
United does not consider its Improper Record Request Scheme to be a prohibited medical
management requirement; (ii) why Covid Testing claims and records provided in response to
Covid Testing claims are reviewed and adjudicated inconsistently; (iii) why Covid Testing claims
submitted by Plaintiff continue to be denied, despite providing United with all of Plaintiff’s
credentialing materials; and (iv) why United feels that its conduct does not constitute violations of
the FFCRA, the CARES Act, and other applicable Federal and State authorities.
39
128. Neither Optum’s Head of Regulatory Affairs nor any other representative from
United ever responded to Plaintiff’s concerns and grievances despite Plaintiff’s multiple attempts
to follow-up on its inquiries.
129. Additionally, included with each patient record produced to United in response to
United’s claim-by-claim record requests, Plaintiff also includes a supporting letter notifying
United of the: (i) legitimacy of Plaintiff and its credentials to render Covid Testing services to its
members; (ii) United’s obligations to process its members’ Covid Testing claims in accordance
with the FFCRA and CARES Act; (iii) the improper and burdensome nature of United’s Improper
Record Request Scheme (iv) and that the Improper Record Request Scheme constitutes as an
39
Exhibit F (Plaintiff’s Email Exchange with United’s Head of Regulatory Affairs Commencing on April 15, 2021).
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 48 of 89

Page 49 of 89
improper medical management requirement that is prohibited by Section 6001 of the FFCRA.
40
130. Despite Plaintiff’s inclusion of the supporting letters with each members’ records
produced to United, United pressed forward with its Improper Record Request Scheme and failed
to provide a single response to address Plaintiff’s concerns.
131. Ultimately, United’s Improper Record Request Scheme has an adverse financial
impact on United members whose claims are denied. The financial responsibility of the Covid
Testing services shifts from United and the Employer Plans to becoming the responsibility of the
member. Section 6001 of the FFCRA and Section 3202(a) of the CARES Act were passed by
Congress to protect against this shifting of financial responsibility.
b. The Inconsistent Adjudication of Covid Testing Claims
132. As touched on above, United not only fails to apply a consistent criteria for its
representatives to review records submitted by Plaintiff and other similarly situated OON
providers of Covid Testing services, but United has also failed to adjudicate Covid Testing claims
that have not been subject to United’s Improper Record Request Scheme.
i. Inconsistent Adjudication of Covid Testing Claims of Members of the Same
Self-Funded Health Plan Subject to ERISA
133. On July 23, 2020, Plaintiff provided Covid Testing services to a family of eight, all
belonging to the same self-funded health plan that United administers (Health Plan Group Number
917201) that is subject to ERISA. Even though the family members are all members of the same
self-funded health plan, all received Covid Testing services on the same day, and their Covid
Testing claims are all subject to the same applicable laws, the claims submitted by Plaintiff on
behalf of the eight family members were adjudicated by United to have five different outcomes.
41
40
Exhibit G (Plaintiff’s Supporting Letter Accompanying Patient Records Produced to United in Response to United’s
Improper Record Request Scheme).
41
All eight of the family members’ Covid Testing service claims were submitted using the same HCFA 1500 claims
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 49 of 89

Page 50 of 89
134. By way of example, below are high level overviews of how each of the eight claims
were adjudicated by United:
• Patient EEG is the primary subscriber to this self-funded health plan. Upon
review of Patient EEG’s records, United denied the actual Covid Testing
service (CPT Code U0004) because the claim lacked information or had
submission or billing errors, but reimbursed Plaintiff its cash price for its
specimen collection services (CPT Code G2023).
42
• Patient JP is the spouse of Patient EEG and Patient JJR and Patient KR are both
dependents of Patient EEG. Upon initial review of the records of Patient JP,
Patient JJR, and Patient KR, all three claims were fully denied by United.
However, each claim was reprocessed by United and Plaintiff was reimbursed
the full cash price for these services.
43
• Patient JNG and Patient IAR are both dependents of Patient EEG. Upon initial
review of the records of Patient JNG and Patient IAR, both claims were fully
denied by United. Neither claim has been reprocessed as United has denied
Plaintiff’s attempts to appeal United’s denials.
44
• Patient ER is a dependent of Patient EEG. Upon initial review of Patient ER’s
records, the claim was fully denied by United. The claim was reprocessed by
United at an in-network rate arbitrarily and unilaterally determined by United
even though Plaintiff is an OON provider. However, after reprocessing the
claim and paying Plaintiff an in-network rate that conflicts with the health
plan’s reimbursement requirements, United made an overpayment
determination on this claim in the full amount of the in-network rate Plaintiff
was reimbursed because the records previously provided lacked information or
had submission billing errors.
45
• Patient JEG is a dependent of Patient EEG. Upon initial review of Patient JEG’s
records, the claim was fully denied by United. Patient JEG’s claim was
reprocessed by United and Plaintiff was reimbursed the full cash price for its
services. However, after reprocessing the claim and paying Plaintiff the full
cash price, United then made an overpayment determination on this claim in the
full amount that Plaintiff was reimbursed because the records previously
provided lacked information or had submission billing errors.
46
form that is uniformly completed by Plaintiff and the same records were produced to United on each claim in response
to United’s claim-by-claim record requests.
42
See Exhibit H (Patient EEG’s Full Administrative Covid Testing Claims File).
43
See Exhibit I (Patient JP, Patient JJR, and Patient KR’s Full Administrative Covid Testing Claims Files).
44
See Exhibit J (Patient JNG and Patient IAR’s Full Administrative Covid Testing Claims Files).
45
See Exhibit K (Patient ER’s Full Administrative Covid Testing Claims File).
46
See Exhibit L (Patient JEG’s Full Administrative Covid Testing Claims File).
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 50 of 89

Page 51 of 89
135. Five of this family’s eight Covid Testing claims were not adjudicated in accordance
with the requirements of the FFCRA and the CARES Act, and, even for two of the claims that
Plaintiff did receive full or partial reimbursement for, United unilaterally and arbitrarily
determined that it had overpaid on those claims for conflicting and inconsistent reasons. So even
if Plaintiff is paid any amount for Covid Testing services from the funds of self-funded health
plans (e.g. Employer Plans), Plaintiff remains at risk as United may at any time unilaterally and
arbitrarily determine that it overpaid Plaintiff and engage in suspect offsetting and recovery
practices with no benefit to the self-funded health plans or their members
136. Section 6001 of the FFCRA and Section 3202(a) of the CARES Act were passed
by Congress to protect Patient EEG and his family from any financial responsibility for Covid
Testing. However, because United failed to reimburse Plaintiff either at its cash price or a
negotiated amount, Patient EEG and the rest of his family are now financially responsible for the
balance of what was unpaid by (or recouped by) United on behalf of the self-funded health plans
it administers. United is not adjudicating the claims it is charged to administer, through self-funded
health plans, in the best interests of its members.
ii. Inconsistent Adjudication of Covid Testing Claims of Members of the Same
Fully-Insured Health Plan Subject to the Texas Insurance Code
137. Plaintiff provided Covid Testing services to three members of the same EPO health
plan that is fully-insured by United (Health Plan Group Number 2U7557) and is subject to the
Texas Insurance Code. Each of the three members are all members of the same fully-insured EPO
health plan, all received Covid Testing services in the same benefit plan year, and their Covid
Testing claims are all subject to the same applicable laws. However, these three members’ claims
were adjudicated by United to have three different outcomes.
47
47
All three of the members’ Covid Testing service claims were submitted using the same HCFA 1500 claims form
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 51 of 89

Page 52 of 89
138. By way of example, below are high level overviews of how each of the three claims
were adjudicated by United:
• Patient GBG is a member of United’s EPO health plan with Group Number
2U7557. Upon review of Patient GBG’s records, United denied the actual
Covid Testing service (CPT Code U0004) because the claim lacked information
or had submission or billing errors, but allowed for Plaintiff to be reimbursed
its cash price for its specimen collection services (CPT Code G2023). However,
no amount for specimen collection services were ever paid to Plaintiff as it was
recouped by United to make itself whole for an overpayment determination
unilaterally and arbitrarily made on a different Covid Testing claim.
48
• Patient KLH is a member of United’s EPO health plan with Group Number
2U7557. Upon initial review of Patient KLH’s records, the claim was fully
denied by United. However, Patient KLH’s claim was reprocessed by United
and Plaintiff was reimbursed the full cash price for these services.
49
• Patient SM is a member of United’s EPO health plan with Group Number
2U7557. Upon initial review of Patient SM’s records, the claim was fully
denied by United. Patient SM’s claim has not been reprocessed.
50
139. Two of the three Covid Testing claims were not adjudicated in accordance with the
requirements of the FFCRA and the CARES Act that TDI Commissioner’s Bulletin B-0017-20
demands insurers of EPO health plans comply with, and, even for the two claims Plaintiff did
receive full or partial reimbursement for, United may unilaterally and arbitrarily determine that it
has overpaid on those claims for conflicting and inconsistent reasons. So even if Plaintiff is paid
any amount for Covid Testing services from United’s funds, Plaintiff remains at risk as United
may at any time unilaterally and arbitrarily determine that it overpaid Plaintiff and engage in
suspect offsetting and recovery practices to detriment of its members.
that is uniformly completed by Plaintiff and the same records were produced to United on each claim in response to
United’s record requests.
48
See Exhibit M (Patient GBG’s Full Administrative Covid Testing Claims File).
49
See Exhibit N (Patient KLH’s Full Administrative Covid Testing Claims File).
50
See Exhibit O (Patient SM’s Full Administrative Covid Testing Claims File).
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 52 of 89

Page 53 of 89
140. TDI Commissioner’s Bulletin B-0017-20 was issued by TDI to reinforce to insurers
that Section 6001 of the FFCRA and Section 3202(a) of the CARES Act were passed by Congress
to protect Patient GBG and Patient SM from any financial responsibility for Covid Testing.
However, because United failed to reimburse Plaintiff either at its cash price or a negotiated
amount, Patient GBG and Patient SM are now financially responsible for the balance of what was
unpaid by United as the insurer for this EPO health plan. United is not adjudicating the claims it
fully insures in the best interests of its members.
c. Meritless Internal Administrative Appeals Process
i. Inconsistent and Arbitrary Appeal Outcomes
141. Looking back to Patient JF’s claim that was used as an example to support
Plaintiff’s allegations of United’s inconsistent and arbitrary records review criteria, this same claim
also evidences United’s failures to provide a full review of appealed Covid Testing claims that
have been denied or otherwise improperly adjudicated.
51
142. Patient JF received Covid Testing services from Plaintiff on July 31, 2020, and
records were requested and provided. Upon initial review of Patient JF’s records, the claim was
fully denied by United for the following reasons:
[INTENTIONALLY LEFT BLANK]
51
See Exhibit P (Patient JF’s Full Administrative Covid Testing Claims File).
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 53 of 89

Page 54 of 89
143. Plaintiff submitted a level 1 appeal to contest the denial of Patient JF’s Covid
Testing claim on the basis that this claim was processed in violation of the FFCRA and the CARES
Act and should be re-adjudicated accordingly. On appeal, this claim was reconsidered by United
and the full cash price for Patient JF’s Covid Testing service was paid to Plaintiff.
52
144. Though, on appeal, Patient JF’s claim was reconsidered and paid at the full cash
price, the vast majority of appeals submitted by Plaintiff to contest United’s adverse benefit
determinations have been denied and largely ignored. By way of example, below is the
adjudication details of Patient MG’s Covid Testing claim. United initially denied Patient MG’s
claim for the following reasons:
[INTENTIONALLY LEFT BLANK]
52
Id.
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 54 of 89
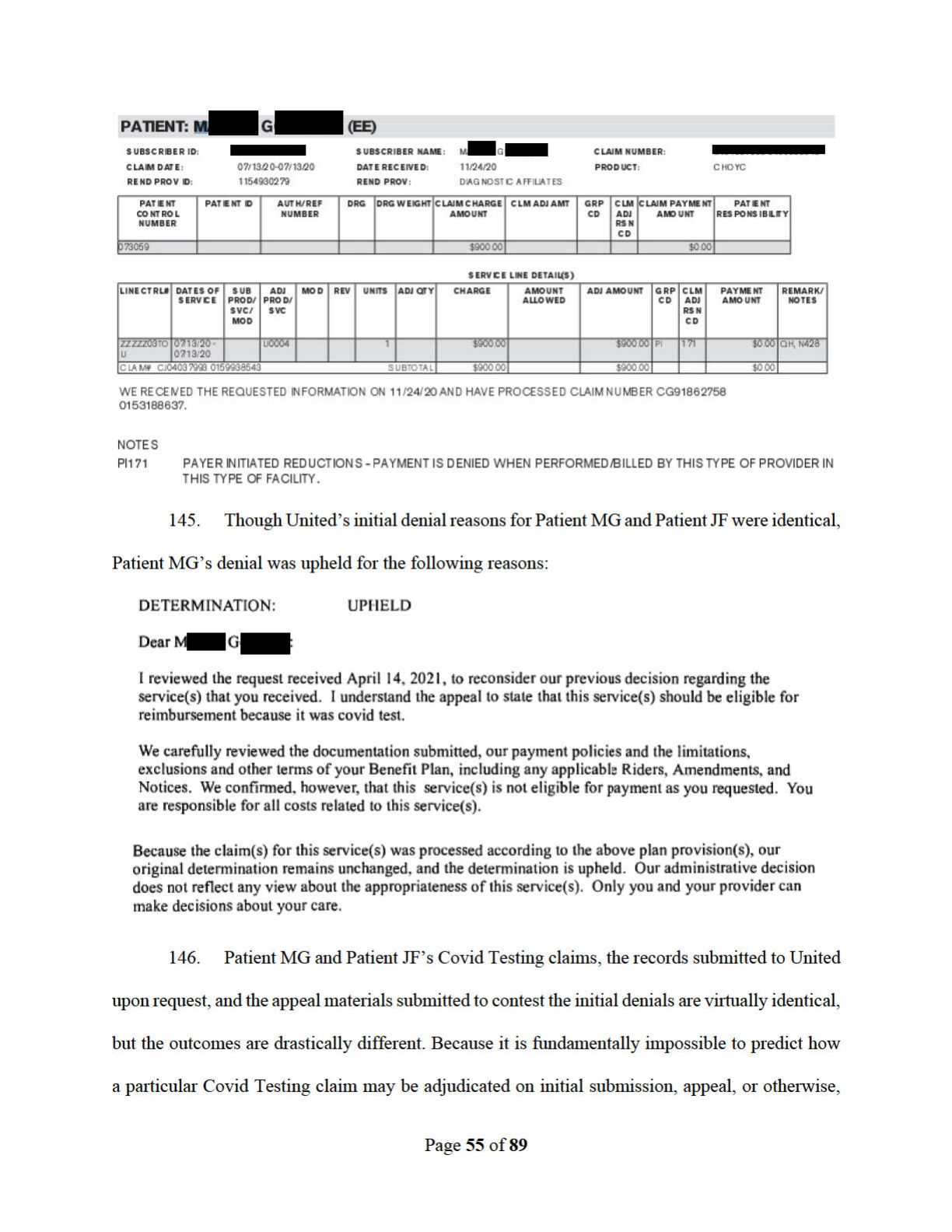
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 55 of 89

Page 56 of 89
especially when the purpose of such applicable laws and guidance were to create a level of
predictability for all stakeholders on how Covid Testing claims should be adjudicated, United’s
claim submission and internal administrative appeals process have no merit.
ii. Failure to Provide Requested Materials to Plaintiff and United Members
147. On all appeal letters submitted to contest United’s adverse benefit determinations,
Plaintiff explicitly requests the following materials that are relevant to adjudication of the Covid
Testing claims:
148. Despite Plaintiff’s request for any and all records relevant to the adjudication of
Covid Testing claims, United has failed to provide any materials in response to Plaintiff’s request
even though United expects Plaintiff to comply with each and every one of its record requests.
149. United is also denying members of its health plans materials they are legally
obligated to disclose to its members upon request.
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 56 of 89

Page 57 of 89
150. Patient VE is a member of a self-funded health plan subject to ERISA. Patient VE
and her three children all received Covid Testing services from Plaintiff and all four Covid Testing
claims were not processed in accordance with the requirements of the FFCRA and the CARES
Act. As a result, Patient VE, in accordance with her rights, personally filed appeals with United on
all four claims, and, as part of her appeal, made the following requests:
53
151. The requested materials were never provided to Patient VE even though the
explanation of benefits and summary plan description outline that she is entitled to such materials.
The explanation of benefits and summary plan description states the following:
Patient VE Explanation of Benefits
Patient VE’s Summary Plan Description
152. Of important note, not only were the requested materials never provided to Patient
VE, but her appeals, mailed to United in March of 2021, have yet to be responded to despite
53
See Exhibit Q (Patient VE’s Level 1 Appeal Letters Submitted to United to Contest the Adverse Benefit
Determinations of Her and Her Children’s’ Covid Testing claims).
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 57 of 89

Page 58 of 89
United’s legal obligations to respond to appeals within 30-45 days.
153. Lastly, Patient MO’s claim to United for Covid Testing services was adjudicated
incorrectly. On or about April 23, 2021, Patient MO contacted United to contest his adverse benefit
determination for fear that he may be balance billed by Plaintiff for Covid Testing services.
154. During the course of his call, Patient MO was informed of useful information
relevant to the adjudication of his Covid Testing claim and was informed that he may request a
copy of the recording and/or transcript of his call for his records. Patient MO sent a request to
United for a copy of the recording and/or transcript of the call to utilize as supporting materials to
include in his appeal to United; however, United did not provide Patient with the specific materials
that he requested, thus, unfairly prejudicing Patient MO before even attempting to file a personal
appeal.
54
155. Not only is Plaintiff reeling from the effects of United’s Improper Record Request
Scheme and its inconsistent and arbitrary claims adjudication and appeals practices, but United is
also denying Plaintiff and its members all relevant documents and materials needed to engage in
and properly contest United’s unlawful practices through United’s internal administrative appeals
processes. Without these materials, Plaintiff and United members are denied their rights to a full
and fair review of their Covid Testing claims in contravention of ERISA, the Affordable Care Act,
and other applicable federal and state laws; therefore, United’s internal administrative appeals
process is functionally meritless.
54
See Exhibit R (Patient MO’s Request for a Transcript and Recording of Conversation dated April 23, 2021).
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 58 of 89

Page 59 of 89
iii. Deemed Exhaustion of Internal Administrative Appeals Process Due to
Violations of the FFCRA, the CARES Act, and Internal Administrative
Appeals Requirements
156. United’s internal administrative appeals process has no merit.
157. This kangaroo court either intentionally created by United or created through its
intentional disregard of its obligations to maintain a just and fair internal administrative appeals
process should be made an example of.
158. Pursuant to 29 C.F.R. § 2560.503-1(l) and 45 C.F.R. §§ 147.136(b)(2)(ii)(F)(1),
(b)(3)(ii)(F)(1), United and the Employer Plans’ internal claims and appeals processes failed to
comply with or strictly adhere to the minimum requirements of the internal claims and appeals
processes as prescribed by 29 C.F.R. § 2560.503-1 and/or 45 C.F.R. § 147.136; therefore, the
internal claims and appeals processes available under each United Plan and Employer Plans are
deemed to have been exhausted, allowing Plaintiff to pursue any available remedies under Section
502(a) of ERISA or under State law on the basis that United and the Employer Plans have failed
to provide a reasonable claims procedure that would yield a decision on the merits of the Covid
Testing claims at issue.
159. Additionally, pursuant to 45 C.F.R. §§ 147.136(b)(2)(ii)(F)(2), (b)(3)(ii)(F)(2),
United, in its capacity as an insurer and third-party claims administrator, failed to respond to
Plaintiff’s written request for a written explanation of United and the Employer Plans’ patterns
and practices of violations as alleged and detailed in this Original Complaint within ten (10) days
of Plaintiff’s specific written request to United; therefore, the internal claims and appeals processes
available under each United Plan and Employer Plans are further deemed to have been exhausted.
55
55
A specific written request for a detailed explanation of United and the Employer Plans’ numerous violations was
made by Plaintiff to United on May 3, 2021, but not response was ever provided. Despite United’s failure to respond
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 59 of 89

Page 60 of 89
d. Financial Incentives and Benefits for United to Unlawfully Adjudicate Covid
Testing Claims
i. Health Plans Fully-Insured by United
160. Individuals and employers that pay premiums directly to an insurer are typically
members of fully-insured health plans, and the members’ medical costs are paid using the funds
of the insurer. Because the medical costs are paid using the funds of the insurance company, the
insurer assumes all the risk of providing health coverage for insured members. As a result, the
more of its own funds an insurer must utilize to cover medically necessary services, the less
revenue an insurance company has to distribute internally to its stakeholders and investors and to
utilize for itself.
161. United is at risk and financially responsible for reimbursing Plaintiff for Covid
Testing claims submitted by Plaintiff on behalf of members of United’s fully-insured health plans.
United’s Improper Record Request Scheme, meritless claims and administrative review processes,
and blatant disregard of its obligations to comply with the requirements of the FFCRA, the CARES
Act, and TDI guidance are done by United to drastically limit funds United has a fiduciary
obligation to pay to providers of Covid Testing services so that it may financially benefit from
such adverse benefit determinations.
ii. Self-Funded Health Plans Administered by United
162. By contrast, many larger employers (e.g. Employer Plans) choose to assume the
risk for payment of medical claims by sponsoring a benefits plan that forms a specific fund for that
purpose, and is funded by the employer and/or employees who contribute premium payments to
the fund. Employers that elect to have a self-funded health plan generally contract with insurance
to Plaintiff within ten (10) days of the Plaintiff’s written request, Plaintiff attempted to again solicit a written
explanation from United on two (2) subsequent occasions – May 5 and May 20, 2021.
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 60 of 89

Page 61 of 89
companies to act in the capacity of a third-party claims administrator to oversee the claims and
appeals processing and other administrative services.
163. Employer Plans have contracted with United to act as their self-funded health plans’
third-party claims administrator, and United is duly compensated by Employer Plans for providing
such administrative services.
164. United’s compensation is made up of a number of administration and access fees
that are charged to the Employer Plans, which include, but are not limited to, cost reduction
services aimed at generating savings on claims when the primary network is not utilized. As part
of these cost reduction services offered by United is known as its CRS Benchmark Program, United
takes for itself anywhere between 20% to 35% of the “savings” it is able to manufacture for itself
through this program.
165. For example, Patient MM received Covid Testing services from Plaintiff on July
10, 2020, and rather than pay Plaintiff the full cash price or negotiate an amount less than the cash
price to pay, United pushed this claim into its CRS Benchmark Program and arbitrarily and
unilaterally determined an amount to be paid. By subjecting this claim to the CRS Benchmark
Program, United is able to pocket up to 35% of the difference between the charge amount and the
payment amount shown below:
[INTENTIONALLY LEFT BLANK]
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 61 of 89

Page 62 of 89
166. Though Plaintiff was paid $185.19 on Patient MM’s claim, United was able to
pocket up to $294.00 for itself. The amount United has paid itself is more than what United has
paid to Plaintiff for providing bona fide Covid Testing services to Patient MM.
167. Because of the CRS Benchmark Program, United has no incentive to comply with
the CARES Act and to reimburse Plaintiff the cash price for its Covid Testing services or to
negotiate an in-network agreement or an amount to be paid on Covid Testing claims despite
Plaintiff’s numerous attempts to enter into good faith negotiations.
168. United has had hundreds, if not thousands, of Covid Testing claims placed into the
CRS Benchmark Program, unilaterally and arbitrarily set a price to be paid on the Covid Testing
claims, paid such claims using the proceeds of the self-funded health plans United administers,
then has pocketed anywhere between 20% to 35% of the “savings” between Plaintiff’s cash price
and the amount actually reimbursed.
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 62 of 89

Page 63 of 89
169. From the perspective of the self-funded health plans, it has and remains financially
prudent for United to negotiate an amount to be paid on Covid Testing claims with Plaintiff.
However, rather than act in the best financial interests of its clients and in the best interests of the
clients’ employees, United chose its own best interest.
170. United has used unlawful and willful conduct to abstract and convert the assets and
funds of self-funded health plans to the benefit of its own financial interest in violation of 18.
U.S.C. § 664.
iii. HRSA COVID-19 Uninsured Program Partnership with United
171. As part of the national effort to combat the COVID-19 pandemic, the Health
Resources & Services Administration (“HRSA”) instituted the HRSA COVID-19 Uninsured
Program to provide reimbursements on a rolling basis directly to eligible providers for claims
attributed to the testing, treatment, or vaccine administration for COVID-19 for uninsured
individuals. HRSA has contracted with United to administer this program, but reimbursement for
COVID-19 related services is made from the Provider Relief Fund and the American Rescue Plan
Act of 2021.
56
172. Because United is not at risk for paying Covid Testing claims on behalf of the
uninsured and cannot subject claims billed by Plaintiff to the HRSA COVID-19 Uninsured
Program to its CRS Benchmark Program, virtually none of these claims have been subject to
United’s Improper Record Request Program, been denied for technical billing issues, nor
otherwise denied in the same manner as the Covid Testing claims submitted to plans United insures
or administers. This is not a coincidence.
56
https://www.hrsa.gov/coviduninsuredclaim/frequently-asked-questions
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 63 of 89

Page 64 of 89
e. United’s Disinformation Campaign
i. Misrepresentations to Plan Sponsors and Administrators of Health Plans
United Administers
173. In an effort to amicably resolve all issues Plaintiff has detailed in this Original
Complaint, Plaintiff sent notice letters to the Employer Plans and other self-funded health plans to
inform the health plans of United’s misconduct and to implore the health plans to take action.
Some health plans were responsive, but the majority were not.
174. One responsive health plan directly inquired with United as to why its members’
Covid Testing claims were not being adjudicated, and United provided these initial responses:
175. When presented with the language of the FFCRA and the CARES Act and the
FAQs issued by the Departments, United again misrepresented its obligations:
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 64 of 89

Page 65 of 89
176. Lastly, when informed by the health plan that Plaintiff’s billed rates are the cash
price, that Plaintiff has appealed a substantial portion of the adverse benefit determinations and
has included its cash price in the appeal letters, and United has not even attempted to negotiate a
rate to be paid on Covid Testing claims, despite Plaintiff’s efforts to negotiate, United fell silent
and has failed to respond to this health plan’s concern.
57
177. This communication between the health plan and United is representative of the
misrepresentations that United directly makes to self-funded health plans, including the Employer
Plans. Moreover, these misrepresentations directly conflict and contradict with the information
and materials available on United’s website, and with all applicable Federal and State laws and
guidance.
ii. Misrepresentations to Members of Health Plans Insured and Administered
by United
178. In the event of any adverse benefit determination, Federal and State laws pertaining
to the internal claims and appeals processes require issuers and health plans to inform its members
57
Exhibit S (Self-Funded Health Plan Communications with United Regarding the FFCRA and the CARES Act).
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 65 of 89
Page 66 of 89
of the outcome of how their particular medical claims are adjudicated and to provide the specific
reasons for the adverse benefit determination. Members are provided these notices by mail and/or
through an electronic medium.
179. Through these communications to its members, United has consistently
misrepresented its obligations as to how Covid Testing claims should be adjudicated. Not only do
the representations to the members contradict with the applicable authorities, but the explanations
and remarks also conflict with the representations made on United’s website, made to self-funded
plans it administers, and to Plaintiff.
180. In a series of communications, between a United member and multiple United
representatives, pertaining to the improper adjudication of the member and his child’s Covid
Testing Claims, United informs the member that his claims were adjudicated correctly, but were
unwilling to provide any internal materials or policies that support United’s adjudication of the
claims. Furthermore, when inquiring why his and his child’s claims were adjudicated differently,
United was unable to provide an explanation.
181. Patient RB, a member of a self-funded health plan administered by United, obtained
Covid Testing services from Plaintiff on December 18, 2020. Patient RB’s child, a dependent of
Patient RB, also obtained services from Plaintiff on December 14, 2020. In contravention of the
FFCRA and the CARES Act, both claims were mis-adjudicated by United and also had different
outcomes, and when inquiring about his concerns, Patient RB was consistently misled by United
of United’s obligations.
[INTENTIONALLY LEFT BLANK]
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 66 of 89

Page 67 of 89
Patient RB’s First Call with United (52 Minutes, 57 seconds)
• Upon receipt of his initial explanation of benefits informing him of his denied
Covid Testing claim, Patient RB placed a call to United on April 20, 2021, to further
inquire about the outcome of his claim. The claim representative (“UHC
Representative 1”) informed Patient RB that his claim was denied because, under
the terms of Patient RB’s health plan, Patient RB did not have OON benefits;
therefore, all services received from OON providers, regardless of whether the
services were COVID-19 related, are to be denied.
58
• Patient RB requested that this call be escalated as UHC Representative 1’s
explanation conflicted with his understanding of how Covid Testing claims should
be adjudicated. The call was escalated to a second United representative (“UHC
Representative 2”). While UHC Representative 2 researched Patient RB’s
concerns, UHC Representative 1 informed Patient RB that it is difficult to provide
a clear answer on how Covid Testing claims should be adjudicated as United is
consistently changing its internal policies and requirements on a daily basis. For
example, UHC Representative 1 states that under the terms of Patient RB’s health
plan, OON Covid Testing services were covered until approximately the end of
2020, but, effective January 2021, OON Covid Testing services are no longer to be
covered.
• UHC Representative 2 informed Patient RB that his health plan does cover OON
Covid Testing services, but only up to 100% of eligible charges, and those eligible
charges are determined by a federal mandate. Additionally, because there would be
a difference between what United pays due to eligible charges/federal mandate and
the billed amount/cash price for the Covid Testing services, the OON provider
would be able to bill Patient RB for the balance bill.
59
Patient RB requested that he
be provided with materials detailing the federal mandate but was informed that it
was an internal document that could not be provided to him.
60
58
This is a flagrant misrepresentation of United’s obligations to cover Covid Testing services. Section 6001 of the
FFCRA, as amended by section 3201 of the CARES Act, applies to group health plans and health insurance issuers
offering group or individual health insurance coverage (including grandfathered health plans as defined in section
1251(e) of the Patient Protection and Affordable Care). The term “group health plan” includes both insured and self-
insured group health plans. It includes private employment-based group health plans (ERISA plans), non-federal
governmental plans (such as plans sponsored by states and local governments), and church plans.
59
The Departments read the requirement to provide coverage without cost sharing in section 6001 of the FFCRA,
together with section 3202(a) of the CARES Act establishing a process for setting reimbursement rates, as intended
to protect participants, beneficiaries, and enrollees from being balance billed for an applicable COVID-19 test. Section
3202(a) contemplates that a provider of COVID-19 testing will be reimbursed either a negotiated rate or an amount
that equals the cash price for such service that is listed by the provider on a public website. In either case, the amount
the plan or issuer reimburses the provider constitutes payment in full for the test, with no cost sharing to the individual
or other balance due. Therefore, the statute generally precludes balance billing for COVID-19 testing. However,
section 3202(a) of the CARES Act does not preclude balance billing for items and services not subject to section
3202(a), although balance billing may be prohibited by applicable state law and other applicable contractual
agreements.
60
Patient RB’s initial explanation of benefits states, “An internal rule, guideline, protocol, or other similar criterion
was referenced in making this possible adverse benefit determination. A copy of the rule, guideline, protocol, or other
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 67 of 89

Page 68 of 89
• Patient RB inquired with UHC Representative 2 as to why his Covid Testing claim
was not initially adjudicated in accordance with United’s federal mandate/internal
policies. UHC Representative 2 stated that he was uncertain but if he had reviewed
the claim that it would have been processed in accordance with his explanation.
UHC Representative 2 goes on to state that even though United’s internal policies
provide for a federal mandate for Covid Testing claims, United may also pay an
OON provider an amount higher than the federal mandate.
• Patient RB also made reference to the Departments’ FAQ guidance as well which
states that OON providers are to be paid either their cash price or a negotiate
amount, but UHC Representative 2 again stated that he is only permitted to process
Patient RB’s claim in accordance with internal policies. The internal policy relied
upon was last updated on April 13, 2021. Updates to the internal policy are
regularly circulated.
Patient RB’s Second Call with United (1 Hour, 18 Minutes, 59 Seconds)
• Patient RB’s claim was reprocessed and paid in accordance with UHC
Representative 2’s explanation; however, the second explanation of benefits
provides that the OON provider cannot balance bill Patient RB, which contradicts
UHC Representative 2’s explanation regarding an OON provider’s right to balance
bill.
• In a call with a third United Representative (“UHC Representative 3”) on April 30,
2021, Patient RB was informed that Plaintiff was prohibited from balance billing
Patient RB on this claim.
61
Patient RB also requested that he be provided the federal
and state emergency guidance materials that United relied upon when adjudicating
his claim, but UHC Representative 3 informed him that he is only entitled to his
explanation of benefits and nothing else.
62
• During the call with Patient RB, UHC Representative 3 contacted Plaintiff to
discuss Patient RB’s claim. After UHC Representative 3’s call with Plaintiff,
Patient RB was informed that he is not financially responsible for the claim and that
additional materials on why Patient RB is not responsible for the difference will be
provided to Plaintiff.
63
• Patient RB requested that the call be escalated, and Patient RB then spoke with a
fourth United representative (“UHC Representative 4”). UHC Representative 4
informed Patient RB that the adjudication of his claim was correct since it was
processed in accordance with Medicare guidelines, and read the internal policy to
similar criterion may be requested free of charge [emphasis added].”
61
Supra Footnote 14
62
Patient RB’s second explanation of benefits states, “An internal rule, guideline, protocol, or other similar criterion
was referenced in making this possible adverse benefit determination. A copy of the rule, guideline, protocol, or other
similar criterion may be requested free of charge [emphasis added].”
63
Patient RB has not been provided with any materials as of the date of this Original Complaint.
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 68 of 89

Page 69 of 89
Patient RB. Patient RB again inquired whether the internal policy and materials
could be provided, but UHC Representative 4 was not able to provide the
materials.
64
Patient RB’s Third Call with United (26 Minutes, 2 Seconds)
• A fifth United representative (“UHC Representative 5”) called Patient RB to
discuss his Covid Testing claim. When Patient RB requested clarification on
whether United is obligated to pay Plaintiff’s cash price or a negotiated amount,
but UHC Representative 5 did not provide an explanation.
• Patient RB again inquired as to whether he is entitled to access to policies and
materials used or relied upon in the adjudication of his Covid Testing claim, and
UHC Representative 5 informed Patient RB that he may be able to obtain the
materials from the claims processing department.
65
• Patient RB also inquired about his child’s Covid Testing claim that was also
adjudicated and paid at a different amount than Patient RB’s claim. UHC
Representative 5 was unable to provide a response, and informed Patient RB that
she would investigate the matter and call him with her findings.
Patient RB’s Fourth Call with United (16 Minutes, 51 Second)
• UHC Representative 5 called Patient RB to inform him of her findings. Patient RB
was informed that the re-adjudication of his Covid Testing claims was actually
incorrect because United overpaid Plaintiff on Patient RB’s claim and that an
overpayment notice will be issued to Plaintiff for a refund to United.
• Patient RB explained to UHC Representative 5 that a prior United representative
informed him that United’s internal policy required OON providers of Covid
Testing to be reimbursed at a fixed federally mandated amount, but UHC
Representative 5 provided no additional insight or comments.
• UHC Representative 5 did not provide any comment on the Covid Testing claim
for Patient RB’s child.
• Patient RB was transferred to a sixth United representative (“UHC Representative
6”) to discuss the adjudication of his Covid Testing claim. After summarizing his
experiences with multiple United representatives, Patient RB again requested all
materials involved in the review of his claim. UHC Representative 6 denied Patient
RB’s request for materials and informed him that he needs to send a written request.
64
Supra Footnote 62
65
Patient RB had previously requested the United claims department to provide him with materials relevant to the
adjudication of his claim, but a representative from the United claims department informed him that they are unable
to provide the materials to him.
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 69 of 89

Page 70 of 89
• Patient RB further inquired about UHC Representative 6’s understanding of the
CARES Act and its requirement for United to either pay the cash price or a lower
agreed upon amount. UHC Representative 6 stated that OON providers are paid at
a usual and customary rate, not in accordance with the CARES Act.
• During the call, UHC Representative 6 also noticed that Patient RB’s claim was
processed as in-network because it was a Covid Testing claim even though Plaintiff
is an OON laboratory.
• UHC Representative 6 then informs Patient RB that if he wants to continue to
contest the claims, he should file an appeal to dispute the adjudication of the claims.
182. For nearly three hours, Patient RB was misled by multiple United representatives
as to United’s obligations to process Covid Testing claims in accordance with FFCRA and the
CARES Act, denied materials that he is entitled to, and given non-answers regarding his specific
inquiries/concerns. Additionally, over the course of his call, Patient RB’s Covid Testing claim was
adjudicated three different times, with the final outcome of his claim conflicting with UHC
Representative 2’s explanation.
183. Below are additional examples that are representative of the types of contradictory
and conflicting representations United makes to members who have received Covid Testing
services from Plaintiff and whose claims were not adjudicated in accordance with the requirements
of the FFCRA and the CARES Act:
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 70 of 89

Page 71 of 89
184. Clearly, these statements and remarks made by United to its members regarding the
adjudication of their Covid Testing claims misrepresent United’s obligations to process Covid
Testing Claims in accordance with the FFCRA and the CARES Act. Furthermore, the contents of
these remarks conflict with the explanations provided to Patient RB by the multiple United
representatives he spoke with.
iii. Misrepresentations to Plaintiff and Other Similarly Situated OON Providers
185. Plaintiff has endeavored to address these issues directly with United, but United
has largely remained silent on these issues.
186. Furthermore, Plaintiff’s billing and collection representatives have confronted and
pressed United representatives as to why Covid Testing claims are not being processed in
accordance with the requirements prescribed by the FFCRA and the CARES Act, but United
representatives make contradictory and conflicting representations similar to the statements United
makes to its members and self-funded health plans that it administers.
187. United has been unable to justify its Improper Record Request Scheme nor its
claims and appeals practices to any person that has inquired about its actions.
[INTENTIONALLY LEFT BLANK]
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 71 of 89

Page 72 of 89
CAUSES OF ACTION
COUNT I – VIOLATION OF THE FFCRA AND THE CARES ACT
(Against All Defendants)
188. The foregoing allegations are re-alleged and incorporated by reference as if fully
set forth herein.
189. Defendants offer group health plans and/or are health insurance issuers offering
group or individual health insurance coverage, as those terms are defined under Section 6001 of
the FFCRA.
190. The Covid Testing services that Plaintiff provided to members of the United Plans
and the Employer Plans administered by United constitute as in vitro diagnostic products for the
detection of COVID-19, as provided by Section 6001 of the FFCRA.
191. Plaintiff is an OON laboratory and did not have a negotiated rate with United for
the provision of Covid Testing services.
192. In compliance with the CARES Act, Plaintiff posted its cash prices for Covid
Testing services on its public website.
193. Under section 3202(a)(2) of the CARES Act, if a health plan does not have a
negotiated rate with a provider, such as Plaintiff, for providing Covid Testing services, the health
plan is obligated to pay the provider its posted cash price for providing those services.
194. United and the Employer Plans, despite numerous and persistent demands and
requests, have failed and refused to provide anything remotely close to Plaintiff’s cash price for
providing Covid Testing services. In fact, United has paid nothing for the vast majority of Covid
Testing claims Plaintiff has submitted to United.
195. By reason of the foregoing, Plaintiff has been injured.
196. Based on the above, Plaintiff is entitled to judgment against United and the
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 72 of 89

Page 73 of 89
Employer Plans in an amount to be determined at the trial of this matter, plus interest thereon,
together with the costs and disbursements of this action, including reasonable attorneys’ fees.
COUNT II – VIOLATION OF SECTION 502(a)(1)(B) OF ERISA
(Against All Defendants)
197. The foregoing allegations are re-alleged and incorporated by reference as if fully
set forth herein.
198. All of the Employer Plans at issue are benefit plans established pursuant to the
Employee Retirement Income Security Act of 1974 (“ERISA”).
66
199. ERISA, the FFCRA and the CARES Act require the Employer Plans and United to
reimburse OON providers for Covid Testing Services in a specific manner.
200. United’s denials and mis-adjudication of Covid Testing claims submitted by
Plaintiff on behalf of members of self-funded health plans administered by United (e.g. Employer
Plans) are a violation of the requirements of self-funded ERISA health plans to cover Covid
Testing services and a wrongful denial of benefits owed under ERISA.
201. Many of the members of plans either insured or administered by United who
received Covid Testing services from Plaintiff executed assignment of benefits documents.
202. Moreover, the FFCRA and the CARES Act, by directing all plans, including self-
funded ERISA health plans (e.g. Employer Plans), not just to cover Covid Testing and related
services, but to pay OON providers certain amounts for Covid Testing services provided to covered
members, have obviated the need for a provider to obtain a specific assignment of ERISA benefits
from a member of a health plan subject to ERISA to be entitled to seek reimbursement from the
health plan for Covid Testing services, or to be entitled to bring an action under ERISA for
reimbursement and/or injunctive relief.
66
9 U.S.C. §§ 1001, et seq.
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 73 of 89
Page 74 of 89
203. In effect, the FFCRA and the CARES Act have given OON providers of Covid
Testing services standing to sue self-funded health plans subject to ERISA (e.g. Employer Plans)
for violations of ERISA, including violations of the FFCRA and the CARES Act, regardless of
whether there has been an assignment of benefits. Indeed, the “benefit” Plaintiff is suing for is the
provider reimbursement required by the FFCRA and the CARES Act. The FFCRA and the CARES
Act do not merely require healthcare plans to “cover” Covid Testing services, they require self-
funded health plans to pay amounts directly to OON providers, because the Congressional intent
was to prevent patients from facing any possible out of pocket liability.
204. Pursuant to 29 C.F.R. § 2560.503-1(l) and 45 C.F.R. §§ 147.136(b)(2)(ii)(F)(1),
(b)(3)(ii)(F)(1), United and the Employer Plans’ internal claims and appeals processes (i.e. claims
procedures) failed to comply with or strictly adhere to the minimum requirements of the internal
claims and appeals processes, as prescribed by 29 C.F.R. § 2560.503-1 and/or 45 C.F.R. § 147.136;
therefore, the internal claims and appeals processes available under each United Plan and
Employer Plan are deemed to have been exhausted allowing Plaintiff to pursue any available
remedies under Section 502(a) of ERISA, or under State law on the basis that United and the
Employer Plans have failed to provide a reasonable claims procedure that would yield a decision
on the merits of the Covid Testing claims at issue.
206. Additionally, pursuant to 45 C.F.R. §§ 147.136(b)(2)(ii)(F)(2), (b)(3)(ii)(F)(2),
United, in its capacity as an insurer and third-party claims administrator, failed to respond to
Plaintiff’s written request for a written explanation of United and the Employer Plans’ patterns
and practices of violations as alleged and detailed in this Original Complaint within ten (10) days
of Plaintiff’s specific written request to United; therefore, the internal claims and appeals processes
available under each United Plan and Employer Plan are further deemed to have been exhausted.
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 74 of 89
Page 75 of 89
A specific written request for a detailed explanation of United and the Employer Plans’ numerous
violations was made by Plaintiff to United on May 3, 2021, but no response was ever provided.
Despite United’s failure to respond to Plaintiff within ten (10) days of Plaintiff’s written request,
Plaintiff attempted to again solicit a written explanation from United on two (2) subsequent
occasions – May 5 and May 20, 2021.
207. Thus, Plaintiff has exhausted available administrative remedies, or exhaustion of
administrative remedies would be futile given the above, and, alternatively, United’s utter
disregard for ERISA deadlines and procedures described above excuses any failure to exhaust
administrative remedies.
208. 29 U.S.C. § 1132 provides that a member of a self-funded health plan subject to
ERISA and Plaintiff under these circumstances may bring a civil action to recover benefits due
under the plan, to enforce rights under the plan and to clarify rights and future benefits under the
plan.
209. United and the Employer Plans’ failures to pay Plaintiff in full for covered Covid
Testing services rendered to the members constitutes a breach of these self-funded health plans,
and United and the Employer Plans’ failures were erroneous, arbitrary and capricious and were
without reason, were unsupported by substantial evidence, and were erroneous as a matter of law.
210. Plaintiff is entitled to payment, pursuant to the FFCRA and the CARES Act for the
bona fide Covid Testing services provided to United members.
211. Furthermore, the Court may equitably reform the Employer Plans that do not
comply with ERISA, the FFCRA, and the CARES Act, to render them compliant. Fairness and
justice require such equitable reformation, because the Plaintiff provided an invaluable service to
the community, in reliance on federal law regarding reimbursement, and United is violating that
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 75 of 89

Page 76 of 89
law, to its own benefit and the detriment of the Plaintiff and members of plans United insures and
administers. The Court should equitably reform any of United’s ERISA plans that do not comply
with the FFCRA and the CARES Act at issue to require that they mirror the language of the
FFCRA and the CARES Act.
212. Plaintiff is also entitled to reasonable attorneys’ fees, pursuant to 29 U.S.C. § 1132
(g)(1).
COUNT III – DENIAL OF FULL AND FAIR REVIEW
(Against All Defendants)
213. The foregoing allegations are re-alleged and incorporated by reference as if fully
set forth herein.
214. As assignees and authorized representatives of its patients’ claims, Plaintiff is
entitled to receive protection under ERISA, including (a) a “full and fair review” of all claims
denied by United on behalf of the Employer Plans and other self-funded health plans subject to
ERISA; and (b) compliance by United with applicable claims procedure requirements.
215. Based on all of the foregoing, United’s and the Employer Plans’ actions and
inactions relating to the Covid Testing claims at issue in this lawsuit are tantamount functionally
to an adverse benefit determination of these claims.
216. For denied claims pursuant to 29 U.S.C. § 1133, self-funded health plans subject to
ERISA must: (i) provide adequate written notice to any member whose claim for benefits under
the health plan has been denied, setting forth the specific reasons for such denial, written in a
manner calculated to be understood by the member; and (b) afford a reasonable opportunity to any
member whose claim for benefits has been denied for a full and fair review by the appropriate
named fiduciary of the decision denying the claim.
67
67
29 U.S.C. § 1133(1) and (2)
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 76 of 89

Page 77 of 89
217. ERISA regulations make clear that, in the case of post-service claims submitted
pursuant to group health plans, the required notification that the claim has been denied must be
issued within a reasonable period of time, but not later than 30 days after receipt of the claim,
unless the member or beneficiary is notified that, due to circumstances beyond the plan’s control,
the plan requires an additional 15 days to issue a required denial notification.
68
218. Although United, on behalf of the Employer Plans, is obligated to provide a “full
and fair review” of denied and underpaid claims pursuant to 29 U.S.C. § 1133, United has failed
to do so by, among other things: (a) refusing to provide the specific reason or reasons for the denial
or underpayment of claims; (b) refusing to provide the specific plan provisions relied upon to
support its denials or underpayments; (c) refusing to provide the specific rule, guideline or protocol
relied upon in making the decisions to deny or underpay claims; (d) refusing to describe any
additional material or information necessary to perfect a claim, such as the appropriate
diagnosis/treatment codes; (e) refusing to notify the relevant parties that they are entitled to have,
free of charge, all documents, records and other information relevant to the claims for benefits; (f)
refusing to provide a statement describing any voluntary appeals procedure available, or a
description of all required information to be given in connection with that procedure; (g) refusing
to provide Plaintiff with the documents and information relevant to United’s denial of the Covid
Testing claims; (h) refusing to timely issue required notifications that the claims have been denied
or underpaid; and (i) running a functionally meritless internal administrative appeals process.
219. By failing to comply with the ERISA claims procedure regulations, United and the
Employer Plans failed to provide a reasonable claims procedure.
68
29 C.F.R. § 2560-503.1(f)(2)(iii)(B)
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 77 of 89
Page 78 of 89
220. Because United and the Employer Plans have failed to comply with the substantive
and procedure requirements of ERISA, any administrative remedies are deemed exhausted
pursuant to 29 C.F.R. § 2560.503-1(I) and 29 C.F.R. § 590.715-2719(b)(2)(ii)(F)(1).
221. Exhaustion is also excused because it would be futile to pursue any administrative
remedies, because United does not acknowledge any legitimate basis for its denials, and thus offers
no meaningful administrative process for challenging its denials.
222. Additionally, pursuant to 45 C.F.R. §§ 147.136(b)(2)(ii)(F)(2), (b)(3)(ii)(F)(2),
United, in its capacity as an insurer and third-party claims administrator, failed to respond to
Plaintiff’s written request for a written explanation of United and the Employer Plans’ patterns
and practices of violations as alleged and detailed in this Original Complaint within ten (10) days
of Plaintiff’s specific written request to United; therefore, the internal claims and appeals processes
available under each United Plan and Employer Plan are further deemed to have been exhausted.
A specific written request for a detailed explanation of United and the Employer Plans’ numerous
violations was made by Plaintiff to United on May 3, 2021, but no response was ever provided.
Despite United’s failure to respond to Plaintiff within ten (10) days of Plaintiff’s written request,
Plaintiff attempted to again solicit a written explanation from United on two (2) subsequent
occasions – May 5 and May 20, 2021.
223. Plaintiff has been harmed by United and the Employer Plans’ failures to provide a
full and fair review of appeals submitted and their failure to comply with applicable claims
procedure regulations under ERISA. 29 U.S.C. § 1133.
224. Plaintiff is entitled to relief under 29 U.S.C. § 1132(a)(3), including declaratory and
injunctive relief, to remedy United and the Employer Plans’ failures to provide a full and fair
review, to disclose information relevant to appeals, and to generally comply with applicable claim
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 78 of 89
Page 79 of 89
procedure regulations.
COUNT IV – VIOLATION OF 18 U.S.C. § 1962(C) (NON-ERISA)
(Against United)
225. The foregoing allegations are re-alleged and incorporated by reference as if fully
set forth herein.
226. Plaintiff is a “person” within the meaning of 18 U.S.C. § 1961(3).
227. Each of the Employer Plans and self-funded health plans that United administers is
an “enterprise” within the meaning of 18 U.S.C. §§ 1961(4) and 1962(c). The Employer Plans and
self-funded health plans that United administers were engaged in activities affecting interstate and
foreign commerce at all times relevant to this Original Complaint.
228. United is associated with the Employer Plans and the other self-funded health plans
that it administers and has conducted or participated, directly or indirectly, in the conduct of the
Employer Plans and self-funded health plans that United administers in relation to Plaintiff through
a pattern of racketeering activity within the meaning of 18 U.S.C. § 1961(1) and (5).
229. The pattern of racketeering activity under 18 U.S.C. § 1961(1) and (5), described
more fully throughout this Original Complaint, includes United’s multiple, repeated, and
continuous use of the mails and wires in furtherance of the Improper Record Request Scheme,
meritless claims and appeals processes, its disinformation campaign in violation of 18 U.S.C. §§
1341 and 1343, and embezzlement and/or conversion of self-funded plans assets through its CRS
Benchmark Program in violation 18 U.S.C. § 664. United’s violations have occurred in relation
to, and/or involve benefits authorized, transported, transmitted, transferred, disbursed, or paid in
connection with this COVID-19 Public Health Emergency which is a presidentially declared
“emergency” as this term is defined in Section 102 of the Robert T. Stafford Disaster Relief and
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 79 of 89

Page 80 of 89
Emergency Assistance Act.
69
230. Specific and detailed explanations and examples of United’s use of the mails and
wires to engage in a pattern of racketeering activity and embezzlement, theft, and conversion of
self-funded health plan assets are detailed throughout this Original Complaint.
231. As a direct result of United’s violation of 18 U.S.C. § 1962(c), Plaintiff has suffered
substantial injury to its business and property within the meaning of 18 U.S.C. § 1964(c).
COUNT V – DECLARATORY JUDGMENT PURSUANT TO
28 U.S.C. § 2201 (NON-ERISA)
(Against United)
232. The foregoing allegations are re-alleged and incorporated by reference as if fully
set forth herein.
233. This is a count for declaratory relief pursuant to 28 U.S.C. § 2201.
234. The FFCRA and the CARES Act require health plans and issuers to cover all Covid
Testing services offered by providers, regardless of whether such provider is in network or OON,
and without the imposition of medical management and other requirements, and to reimburse OON
providers either the cash price for Covid Testing services publicized on its website or to negotiate
an amount less than the cash price to be paid to Plaintiff. The CARES Act directs health plans and
issuers to directly reimburse OON providers for their Covid Testing services.
235. United has engaged in unlawful and suspect conduct to circumvent its obligations
to cover bona fide Covid Testing services submitted by Plaintiff on behalf of members of health
plans either insured or administered by United, and has failed to reimburse Plaintiff, an OON
69
42 U.S.C. § 5122; Pursuant to 18 U.S.C. §§ 1341, 1343, if the violation occurs in relation to, or involving any benefit
authorized, transported, transmitted, transferred, disbursed, or paid in connection with, a presidentially declared major
disaster or emergency (as those terms are defined in section 102 of the Robert T. Stafford Disaster Relief and
Emergency Assistance Act (42 U.S.C. 5122)), or affects a financial institution, such person shall be fined not more
than $1,000,000 or imprisoned not more than 30 years, or both.
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 80 of 89

Page 81 of 89
provider, in accordance with the aforementioned methodology prescribed by the CARES Act.
236. United has failed to comply with its obligations to cover Covid Testing services
without the imposition of medical management and other requirements, and has failed to reimburse
Plaintiff in accordance with reimbursement methodology prescribed by the CARES Act. As a
result of United’s conduct and institutional failures, Plaintiff has sustained and will continue to
sustain damages and has been deprived of and will continue to be deprived of the compensation
that Plaintiff is entitled to for providing bona fide Covid Testing services to members of health
pans either insured or administered by United during this public health emergency.
237. The existence of another potentially adequate remedy does not preclude a judgment
for declaratory relief.
70
238. Plaintiff is entitled to supplemental relief pursuant to 28 U.S.C. § 2201, including
the payment of all money that was not paid by United, both either in its capacity as insurer or an
administrator to Plaintiff for providing bona fide Covid Testing as described in this Original
Complaint.
COUNT VI – UNJUST ENRICHMENT & QUANTUM MERUIT (NON-ERISA)
(Against United)
239. The foregoing allegations are re-alleged and incorporated by reference as if fully
set forth herein.
240. Plaintiff provided bona fide Covid Testing services to members of health plans that
United insures and administers.
241. By providing necessary Covid Testing services throughout the course of the
COVID-19 public health emergency to United members, Plaintiff conferred a benefit upon United
because Plaintiff’s provision of Covid Testing services facilitated United’s obligations to arrange
70
See Federal Rules of Civil Procedure, Rule 57.
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 81 of 89
Page 82 of 89
and pay for Covid Testing services for its members. Additionally, United benefited from the
insurance premiums from members and the compensation from Employer Plans and other self-
funded health plans to facilitate and cover Covid Testing services. To satisfy its legal obligations,
United required the Covid Testing services of Plaintiff. Because of Plaintiff’s Covid Testing
services for United’s members, Plaintiff conferred a benefit on United.
242. United knew that Plaintiff provided bona fide Covid Testing services to United
members in satisfaction of United’s obligations to its members. Moreover, at all relevant times,
United either virtually denied or underpaid Plaintiff for its bona fide Covid Testing services for
United members in contravention of its requirements under the FFCRA and the CARES Act.
243. United voluntarily accepted, retained, enjoyed, or continues to accept, retain, and
enjoy the benefits conferred by Plaintiff, with the knowledge that Plaintiff expects to and is entitled
to payment for such Covid Testing services.
244. Despite proper demand being made on United for payment for these services,
United has failed to reimburse Plaintiff for the Covid Testing services provided. United has
received and retained a benefit and has been unjustly enriched through the use of funds that earned
interest or otherwise added to its profits, when said money should have been paid in a timely and
appropriate manner to Plaintiff.
245. As a result of United’s unjust enrichment, Plaintiff has suffered damages. Based on
the above, Plaintiff is entitled to compensatory damages, interest, costs of suit, attorneys’ fees, and
such other relief as the Court deems equitable and just.
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 82 of 89
Page 83 of 89
COUNT VII – PROMISSORY ESTOPPEL (NON-ERISA)
(Against United)
246. The foregoing allegations are re-alleged and incorporated by reference as if fully
set forth herein.
247. United undertook conduct that conveyed to Plaintiff that coverage for COVID
testing would be afforded to its members, but then arbitrarily adjudicated claims and refused to
issue proper reimbursements when the claims were submitted on behalf of the members of health
plans insured or administered by United.
248. United expected, or reasonably should have expected, that Plaintiff would rely on
United’s compliance with the FFCRA and the CARES Act, especially given its public statements
and publications emphasizing its compliance with the aforementioned laws.
249. United’s publicized statements and publications regarding its compliance with the
requirements of the FFCRA and the CARES Act, its proper adjudication of Plaintiff’s Covid
Testing claims subject to the HRSA COVID-19 Uninsured Program, and the adjudication and full
payment of Plaintiff’s cash price on Covid Testing claims from time to time induced Plaintiff’s
reasonable reliance on the promise to pay.
250. Plaintiff detrimentally relied on United’s promises to pay by continuing to provide
Covid Testing services to United members. Plaintiff’s reliance on the promises caused it to suffer
a definite and substantial detriment and has caused it damage.
251. Based on the above, Plaintiff is entitled to compensatory damages, interest, costs
of suit, attorneys’ fees, and such other relief as the Court deems equitable and just.
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 83 of 89

Page 84 of 89
COUNT IX – VIOLATION OF THE
TEXAS PROMPT PAY ACT (“TPPA”) (NON-ERISA)
(Against United)
252. The foregoing allegations are re-alleged and incorporated by reference as if fully
set forth herein.
253. With respect to the plans that United insures, United’s processing of Covid Testing
claims of the claims it insures is governed by the prompt payment requirements of the TPPA
because the prompt payment deadlines apply to claims OON claims for emergency care.
71
254. The TPPA requires United to pay Plaintiff’s Covid Testing claims within 30 days
of the date Plaintiff electronically submits a clean claim and within 45 days of the date Plaintiff
submits a non-electronic clean claim, provided that the Covid Testing claims meets the
requirements of a clean claim.
72
255. Plaintiffs Covid Testing claims meet all the criteria for payment under the TPPA.
As detailed in this Original Complaint, on the dates the Covid Testing services were provided, the
United members of fully-insured health plans and the Covid Testing services were covered under
the terms of the relevant United health plans. Moreover, Plaintiff was eligible for OON payments
under the terms of the relevant United health plans as mandated by the FFCRA and the CARES
Act.
256. Moreover, as detailed throughout this Original Complaint, United accepted all
Covid Testing claims submitted, but failed to adjudicate claims within the prescribed timeframe
and/or continuously failed to adjudicate Covid Testing claims in accordance with the requirements
of the FFCRA and the CARES Act.
71
Texas Insurance Code §§ 843.351 and 1301.069; 28 Tex. Admin. Code § 21.2823
72
28 Tex. Admin. Code § 21.2807(b)
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 84 of 89
Page 85 of 89
257. Instead, as detailed throughout this Original Complaint, United engaged in
unscrupulous and fraudulent conduct to avoid its obligation to reimburse Plaintiff in accordance
with Section 3202(a) of the CARES Act. This unlawful conduct does not excuse United from
delaying payments and/or perpetually paying the improper amount on Covid Testing claims.
258. United’s failures to timely pay the full amounts due to Plaintiff of its Covid Testing
claims has resulted in overdue payment due to Plaintiff pursuant to the TPPA.
259. By reason of the foregoing, Plaintiff is entitled to recover from United the full
underpaid and unpaid amounts due to Plaintiff on all relevant Covid Testing claims, together with
any and all applicable statutory interests pursuant to 28 Tex. Admin. Code § 21.2815.
COUNT X – INJUNCTIVE RELIEF (NON-ERISA)
(Against United)
260. The foregoing allegations are re-alleged and incorporated by reference as if fully
set forth herein.
261. Currently, United is wrongfully denying payment in whole or in part for virtually
all bona fide Covid Testing service claims submitted during this COVID-19 public health
emergency by Plaintiff on behalf of members of health plans either insured or administered by
United. In doing so, United has failed and is failing to comply with the FFCRA, the CARES Act,
ERISA, the terms of the health plans, and other applicable Federal and State laws.
262. Furthermore, as detailed throughout the course of this Original Complaint, United
has engaged in unscrupulous and fraudulent conduct to circumvent its obligations to adjudicate
and reimburse Plaintiff for bona fide Covid Testing services.
263. Unless enjoined from doing so, United will continue to operate its fraudulent
schemes and meritless claims and appeals processes and fail to comply with all applicable
authorities to detriment of Plaintiff, members of health plans insured or administered by United,
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 85 of 89
Page 86 of 89
and the self-funded health plans that United administers. A monetary judgment in this case will
only compensate Plaintiff for past losses and will not stop United from continuing to engage in
unscrupulous and fraudulent conduct and to embezzlement and/or convert the assets of self-funded
health plans, which is necessary for Plaintiff to maintain its laboratory. Plaintiff has not practical
or adequate remedy, either administratively or at law, to avoid these future losses.
264. Plaintiff is entitled to a permanent injunction requiring United to comply with the
requirements of the FFCRA and the CARES for Covid Testing claims submitted on behalf of
members of plans that are insured by United, and removing United as claims administrator to the
self-funded health plans United administers so that United cannot continue to summarily deny
bona fide Covid Testing claims provided by Plaintiff.
JURY DEMAND
Pursuant to Rule 38 of the Federal Rules of Civil Procedure, Plaintiff hereby requests a
trial by jury on all issues so triable.
PRAYER FOR RELIEF
WHEREFORE, Plaintiff demands judgment in its favor against United as follows:
A. Declaring all Defendants have breached the FFCRA and the CARES Act regarding
the coverage and reimbursement of Covid Testing service claims submitted by Plaintiff on behalf
of members of the aforementioned health plans, as well as awarding injunctive and declaratory
relief to prevent United and the Employer Plans’ continuous actions detailed herein;
B. Declaring that Defendants have breached the FFCRA, the CARES Act, ERISA,
and the terms of their health plans regarding the coverage and reimbursement of Covid Testing
service claims submitted by Plaintiff on behalf of members of the aforementioned health plans, as
well as awarding injunctive and declaratory relief to prevent United and the Employer Plans’
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 86 of 89
Page 87 of 89
continuous actions detailed herein;
C. Declaring that all Defendants failed to provide a “full and fair review” under § 503
of ERISA, 29 U.S.C. § 1133, and applicable claims procedures regulations, and that “deemed
exhaustion” under such regulations is effect as a result of Defendants actions and/or inactions, as
well as awarding injunctive, declaratory, and other equitable relief to ensure compliance with
ERISA and its claims procedure regulations;
D. Declaring that Defendants failed to provide a “full and fair review” under § 503 of
ERISA, 29 U.S.C. § 1133, and applicable claims procedures regulations, and that as a result
Defendants’ failures to provide to Plaintiff its requested documents and information, Plaintiff is
entitled to statutory damages under Section 502(c)(1) of ERISA, 29 U.S.C. § 1132(c)(1);
E. Treble the damages sustained by Plaintiff as described above under 18 U.S.C. §
1962(c);
F. Declaring that United violated its statutory obligations to process Covid Testing
claims in accordance with the Section 6001 of the FFCRA and Section 3202(a) of the CARES Act.
G. Statutory interest in prescribed by 28 Tex. Admin. Code § 21.2815;
H. Punitive damages;
I. Compensatory and consequential damages resulting from the injury to Plaintiff’s
business in the millions of dollars, as detailed throughout this Original Complaint and to be further
established at trial;
J. Awarding damages based on United’s misrepresentations and misconduct
regarding its fraudulent schemes and actions employed by United to damaged Plaintiff and
embezzle and/or covert the assets of self-funded plans to the detriment of Plaintiff, members of
plans either insured or administered by United, and the self-funded health plans (e.g.. Employer
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 87 of 89
Page 88 of 89
Plans).
K. Permanently enjoying United from continuing to administers claims processing for
the Employer Plans and other self-funded health plans;
L. Appointing an independent fiduciary at United’s expense to re-adjudicate all of
Plaintiff’s Covid Testing claims initially processed by United, and to reimburse Plaintiff all
amounts United, the Employer Plans, and other self-funded health plans were required to
reimburse Plaintiff pursuant to the FFCRA, the CARES Act, ERISA, and the terms of the health
plans.
M. Ordering United to pay all reasonable costs and expenses of the independent
fiduciary in re-adjudicating the Covid Testing claims.
N. Awarding los profits, contractual damages, and compensatory damages in such
amounts as the proofs at trial will show;
O. Awarding exemplary damages for United’s intentional and tortious conduct in such
amounts as the proofs at trial will show;
P. Awarding restitution for payments improperly withheld by United;
Q. Declaring that United has violated the FFCRA, the CARES Act, and the terms of
the health plans fully-insured by United;
R. Awarding reasonable attorneys’ fees, as provided by common law, Federal or State
statute, or equity, including 18 U.S.C. § 1964(c) and 29 U.S.C. § 1132(g);
S. Awarding costs of suit;
T. Awarding pre-judgment and post-judgment interest as provided by common law,
Federal or State statute or rule, or equity; and
U. Awarding all other relief to which Plaintiff is entitled.
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 88 of 89

Page 89 of 89
Respectfully submitted,
By: /s/ Ebad Khan
Ebadullah (Ebad) Khan
Federal Bar No. 2810999
State Bar No. 2409265
23330 US-59, Suite 300
Kingwood, Texas 77339
(281) 319.8306 Direct
(281) 605.6690 Facsimile
Attorney for Plaintiff
Case 2:21-cv-00131 Document 2 Filed on 06/29/21 in TXSD Page 89 of 89
